Estudios originales
← vista completaPublicado el 24 de septiembre de 2025 | http://doi.org/10.5867/medwave.2025.08.3111
Estudio observacional del perfil de pacientes operados de artroplastia de cadera y rodilla en hospitales públicos chilenos financiados mediante Grupos Relacionados por Diagnóstico, de 2019 a 2023
Observational study of the profile of patients undergoing hip and knee arthroplasty in Chilean public hospitals funded through Diagnosis-Related Groups, from 2019 to 2023
Abstract
Introduction Hip and knee osteoarthritis are common causes of disability, with high social and economic impact. Total hip and knee arthroplasties are cost-effective interventions that significantly improve quality of life. However, timely access to these surgeries in the Chilean public healthcare system remains limited. Since 2019, the Diagnosis-Related Groups (DRG) system has enabled the financing of hospital surgical procedures by adjusting payments according to case complexity. The objective of our study was to describe the hospital volume, clinical profile of patients, and financing situation of arthroplasties performed between 2019 and 2023 in public hospitals operating under the Diagnosis-Related Groups system.
Methods Observational, cross-sectional, and retrospective study. All procedures coded as primary total hip arthroplasty or total knee arthroplasty recorded in the Diagnosis-Related Groups database of the National Health Fund (FONASA) between January 2019 and September 2023 were analyzed. Clinical, demographic, geographic, and economic variables were extracted. Comorbidities were identified using the International Classification of Diseases, 10th revision (ICD-10)
Results A total of 29 409 primary and 1993 revision arthroplasties were performed. Surgical volume decreased in 2020 and recovered progressively. Hospital productivity varied across regions. One-third of the total hip arthroplasties were performed in patients under 65 years old. The most frequent comorbidities were hypertension (43.4%) and diabetes (16.6%). The average reimbursement for revision surgeries was similar to that of primary procedures.
Conclusions We identified regional inequities in access to total hip and knee replacements. We also found possible underreporting of comorbidities and underfunding of revisions, which highlights the need for specific adjustments to the Diagnosis-Related Groups system. In the future, it will be necessary to improve the quality of coding, expand financial coverage for patients excluded from the Explicit Health Guarantees, and incorporate technological adjustments that adequately reflect the costs of revisions, to move toward equitable and sustainable access to these surgeries.
Introduction
Hip and knee osteoarthritis significantly impair quality of life, especially physical function, pain, and social participation. In addition, it is often associated with social isolation, psychological distress, and increased vulnerability in older adults with comorbidities [1,2]. Given the aging population, a sustained increase in the prevalence of these pathologies is projected, a phenomenon that also affects Latin America [3]. In Chile, according to the 2017 National Health Survey, the estimated prevalence of knee osteoarthritis in people over 65 was 13.6% (95% confidence interval: 10.8 to 17.0%) and 20.4% (95% confidence interval: 16.8 to 24.5%) for hip osteoarthritis [4].
Total hip and knee arthroplasties have proven to be cost-effective interventions with a positive impact on quality of life, reducing pain and improving overall patient function [5,6,7,8]. However, timely access to these surgeries in public health systems remains a challenge, especially in contexts of high healthcare demand, such as Chile. Although the annual frequency of total hip and knee arthroplasties has increased steadily between 2004 and 2019, Chile ranks among the lowest countries in the Organization for Economic Cooperation and Development (OECD) in terms of the number of surgeries performed and associated waiting times [9]. In addition, recent studies have shown a growing migration of patients with public coverage to the private sector, with a significant increase in out-of-pocket expenses to access these interventions [10].
The Chilean healthcare system consists of a public component, financed mainly by the National Health Fund (FONASA), and a private component. In recent years, the public sector has promoted efficiency-based financing models, with the Diagnosis-Related Groups system being one of the main advances in this area. Implemented in 2019, DRGs allocate hospital resources according to assessment, complexity, and procedures performed, allowing for more transparent, evidence-based, and comparable management between facilities [11,12]. This model has facilitated the monitoring of institutional performance and serves as a strategic tool for public policy decision-making, particularly in high-volume surgeries such as total hip and knee arthroplasties [13].
The analysis of these surgical interventions through Diagnosis-Related Groups enables not only the characterization of the epidemiological and clinical profiles of beneficiary patients but also the estimation of the economic burden and associated care patterns. This approach is particularly relevant in the context of population aging, the high prevalence of chronic comorbidities, and the increasing incorporation of high-cost medical technologies such as prosthetic implants. To ensure their timely inclusion in the financing system, complementary mechanisms have been developed, such as the technology adjustment, which allows payment to be adapted in cases where the Diagnosis-Related Groups weight does not fully reflect the actual cost of treatment [11]. This strategy is crucial for maintaining the financial sustainability of the system, promoting equity in access, and ensuring the efficient regulation of health technology use, as documented in the international literature on health policy and technology assessment [14].
The purpose of this study is to provide a comprehensive description of the volume, distribution, and clinical and economic characteristics of primary total hip and knee arthroplasties performed in Chilean public hospitals between 2019 and 2023. The study seeks to quantify the annual number of procedures and analyze their distribution by institution, to identify potential access gaps at the national level. Patient age at the time of surgery is also described, with particular emphasis on hip arthroplasties in individuals under 65 years of age, a group that represents a cohort of high functional and social impact. Reported comorbidities are characterized using the International Classification of Diseases, 10th Revision (ICD-10). These comorbidities are determinants both for surgical planning and for risk stratification, as well as for calculating the Diagnosis-Related Groups weight that defines the financing assigned to each episode. Finally, the average reimbursement cost for each type of procedure is estimated, providing key information for system performance assessment and health policy planning.
Methods
This is a cross-sectional observational study with a retrospective approach, based on the analysis of the open database published by the National Health Fund. It compiles records of services provided by the 68 public hospitals financed through the Diagnosis-Related Groups system between 2019 and 2023. The database is available on the National Health Fund website, which corresponds to the public health insurer (available at
All procedures performed between January 1st, 2019, and September 4th, 2023 (244 weeks) were included, identified in the database with the following general procedure codes:
-
81.51: total hip replacement.
-
81.52: partial hip replacement.
-
81.53: hip replacement revision.
-
81.54: total knee replacement.
-
81.55: knee replacement revision.
All patients with a primary diagnosis of a hip or knee fracture were excluded using the ICD-10 codes S72 (femur fracture) and S82 (patella or tibia fracture). A total of 9939 patients were excluded for fractures around the hip, 16 for fractures around the knee, and 21 for both.
In general terms, primary arthroplasty refers to the first implantation of a prosthesis in a joint, whether hip or knee. Revision arthroplasty, meanwhile, involves the partial or total replacement of a previously implanted prosthesis, usually due to complications such as loosening, infection, deterioration, or mechanical failure. During the review and analysis of the database, centers were identified that use general codes with and without specific codes. For this study, procedures with general codes for primary hip or knee arthroplasty (81.51, 81.52, 81.54), with or without specific codes, were considered patients who underwent primary surgery. Knee or hip revisions were considered to be those procedures coded with general codes 81.53 and 81.55, and those procedures that are coded with a specific revision code rather than a general code. Biases are discussed along with limitations. Table 1 shows the distribution of procedures found after applying the inclusion and exclusion criteria.
The following variables were extracted for analysis: age (in years), sex (female/male), hospital where the procedure was performed and its geographical location, primary diagnosis coded using ICD-10, length of hospital stay (in days), and the cost associated with the episode according to the reimbursement value recorded by the National Health Fund for each Diagnosis-Related Group. Likewise, relevant comorbidities reported using ICD-10 codes were identified, including high blood pressure. (I10, I11.0, I11.9, I12.0, I13.1, I15.0, I15.1), diabetes mellitus (E10.2, E10.5, E10.6, E10.8, E10.9, E11.2, E11.3, E11.4, E11.5, E11.6, E11.7, E11.8, E11.9, E13.9, E14.9, H36.0, N08.3, G63.2), hypothyroidism (E03.2, E03.4, E03.8, E03.9, E89.0), obesity (E66.0, E66.2, E66.8, E66.9), asthma (J45.0, J45.1, J45.8, J45.9, J46), chronic obstructive pulmonary disease (J44.0, J44.1, J44.8, J44.9), mood disorders (F31.9, F32.0, F32.1, F32.2, F32.3, F32.8, F32.9, F33.2, F33.4, F33.8, F33.9, F34.1, F34.9, F38.8, F39), fibromyalgia (M79.70, M79.78, M79.79), rheumatoid arthritis (M05.09, M05.39, M05.96, M05.98, M06.86, M06.88, M06.89, M06.90, M06.95, M06. 96, M06.97, M06.98, M06.99), penicillin allergy (Z88.0), and tobacco use (F17.1, F17.2, Z72.0, Z87.891, Z71.6, T65.2, O99.33, P96.81). These variables enabled us to characterize the clinical and demographic profiles of patients who underwent surgery, as well as to evaluate the geographical and financial distribution of arthroplasties performed within the public system. The productivity of each hospital was calculated by dividing the number of surgeries in each center by the number of weeks between January 1st, 2019, and September 4th, 2023 (244), which gives the average number of surgeries per week.
The data were processed and organized using Microsoft Excel, and descriptive analyses were performed using Stata software version 17.
Results
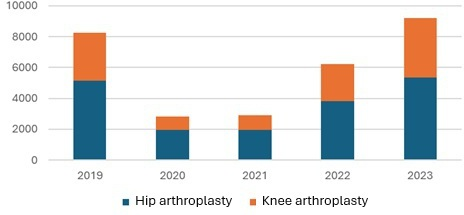
A total of 29 409 procedures were included, of which 18 263 corresponded to total hip arthroplasty (62.1%) and 11 146 to total knee arthroplasty (37.9%). The year 2023 saw the highest number of procedures, totaling 9,205 (31.3%), followed by 2019 with 8,241 (28.0%). This indicates that, following the COVID-19 pandemic, it was not until 2023 that the volume of arthroplasties returned to pre-pandemic levels (Figure 1). The percentage of revisions in hip arthroplasty is 8.3% compared to 4.3% in knee arthroplasty with respect to the total number. In comparison, the ratio of primary knee arthroplasty to the total number of primary procedures is 39% (Table 2).
Number of knee and hip arthroplasty procedures between 2019 and 2023.
Regarding the average age of patients, the average age was 64.4 years (standard deviation: 12.9) in primary hip arthroplasty, with 44.8% under the age of 65. In primary knee arthroplasty, the average age was 68.9 years (standard deviation: 9.1), and 38.2% were under 65 years of age. Patients who underwent hip revision surgery were on average three years older than primary cases (average: 67.5; standard deviation: 14.5), while knee revision patients were one year younger (average: 67.4; standard deviation: 12.9). Women predominate in all scenarios, from 67.4% in hip revision, 62% in primary knee, 59.9% in primary hip, and finally 57.9% in knee revision.
The median hospital stay was three days for both primary hip (range: 1 to 255; interquartile range: 2 to 4) and primary knee (range: 1 to 218; interquartile range: 2 to 4). For revisions, the hospital stay increased to eight days for hip (range: 1 to 341; interquartile range: 4 to 21) and seven days for knee (range: 1 to 325; interquartile range: 4 to 17).
Regarding productivity per hospital, 52 hospitals reported at least one arthroplasty during the period (52 of 68 hospitals included, 76%), while 43 hospitals reported at least one knee arthroplasty (43 of 68, 63%). During the period analyzed, two hospitals exceeded 1000 primary total hip arthroplasty procedures: Dr. César Garavagno Burotto Hospital (Talca) and San Pablo Hospital (Coquimbo). Likewise, five hospitals reached an average of three or more procedures per week. In terms of primary total knee arthroplasty, only one hospital exceeded 1000 procedures during the period: Hospital Clínico Metropolitano La Florida Dra. Eloísa Díaz Inzunza, which was also the only center with an average of more than four procedures per week (4.43). Only one other hospital (Hospital Dr. César Garavagno Burotto, Talca) achieved an average of more than three procedures per week. tables 3 and 4 have the 25 hospitals with the highest volume of primary hip and knee surgery, respectively.
In the clinical characterization of patients undergoing primary total arthroplasty, notable differences were observed in the frequency of comorbidities between knee and hip procedures (Figure 2). In the total knee arthroplasty group, the most frequent comorbidities were hypertension (56.9%), diabetes mellitus (21.7%), hypothyroidism (13.8%), and obesity (12.0%). To a lesser extent, mood disorders (4.2%), asthma (4.0%), rheumatoid arthritis (3.2%), penicillin allergy (2.4%), chronic obstructive pulmonary disease (1.8%), fibromyalgia (0.9%), and smoking (0.03%) were identified. In patients who underwent total hip arthroplasty, the most prevalent comorbidities were hypertension (25.2%), diabetes mellitus (11.3%), hypothyroidism (7.0%), and obesity (4.8%). A lower frequency of mood disorders (2.0%), asthma (1.9%), rheumatoid arthritis (1.1%), penicillin allergy (1.3%), chronic obstructive pulmonary disease (1.2%), fibromyalgia (0.5%), and smoking (0.02%) was also observed. In general, the presence of comorbidities was higher in the total knee osteoarthritis group (Table 5), which could reflect differences in the clinical profile of patients according to the type of procedure, or it could be underreported.
Percentage frequency of the most common comorbidities reported in primary hip and knee arthroplasty.
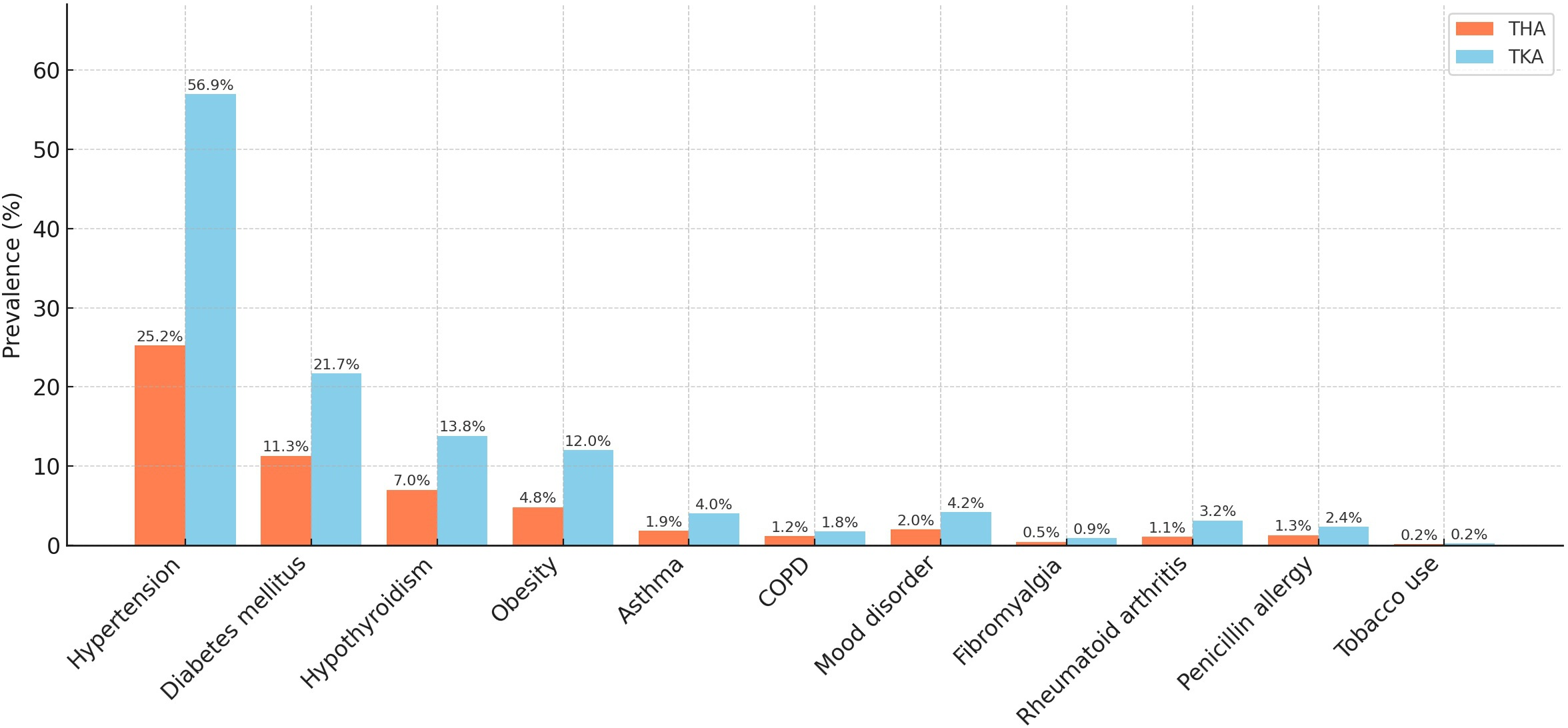
Source: Prepared by the authors based on the study results.
The average reimbursement for each procedure varies according to specific codes. Most primary procedures were performed without specific codes for both knee and hip replacements. For this reason, they obtained a similar average between procedures ($5 873 313 for hip and $5 802 309 for knee). As for revision without special codes, the difference in the average reimbursement is more than one million pesos, with $5 563 625 for hip and $6 693 706 for knee. It is also noteworthy that the average for primary hip surgery is higher than for revision. Although the average reimbursement is higher in knee revision cases, the difference in the average is less than one million pesos (Table 6).
Discussion
The results of this study show that, despite a sustained increase in the number of hip and knee arthroplasties performed in Chilean public hospitals between 2019 and 2023, the overall volume of procedures remains low compared with Organization for Economic Cooperation and Development (OECD) member countries. According to the Health at a Glance 2023 report, Chile ranks among the lowest in the number of hip and knee arthroplasties per 100 000 inhabitants. Although the country has a relatively younger population than other OECD members, this phenomenon cannot be explained solely by age structure, but also by access barriers [15]. This is particularly significant in the public system, where a considerable proportion of patients must seek care from private providers, incurring substantial out-of-pocket expenses [10]. A key finding of this study is that a large proportion of patients undergoing arthroplasty are younger than 65 years: 44.8% for hip arthroplasty and 38.2% for knee arthroplasty. This age group, in their most active working years, is not covered under the Explicit Health Guarantees scheme, as hip arthroplasty is guaranteed only for patients over 65 years, and knee arthroplasty is not included at all. Notably, this policy has not been revised since its original enactment in 2006 [16], that is, for almost 20 years, despite significant changes in demographic, epidemiological, and healthcare needs over time. As a result, these patients remain on waiting lists outside the Explicit Health Guarantees scheme, facing substantially longer delays than for guaranteed interventions, which negatively affects their functionality, quality of life, and social participation [17,18]. As previously documented, publicly insured patients with conditions not covered by the Explicit Health Guarantees scheme wait significantly longer than those with private insurance, perpetuating inequities in access to high-impact surgical procedures [19]. In fact, Chile has one of the longest median waiting times for hip and knee arthroplasty in patients under 65 among OECD countries, with a median of 628 days for knee arthroplasty outside the Explicit Health Guarantees scheme, according to the latest international report [15]. In light of this evidence and given the proven clinical effectiveness and cost-effectiveness of these interventions [6,7], there is an urgent need to reassess current coverage policies, extending the Explicit Health Guarantees scheme to include patients under 65 with severe hip osteoarthritis and incorporating knee arthroplasty as a guaranteed service, regardless of age.
One of the most relevant findings of our study is the low frequency of significant comorbidities such as obesity, hypertension, diabetes mellitus, and smoking, compared to what has been reported in the international literature. These conditions are highly prevalent in patients with osteoarthritis and have been linked to both greater radiographic progression of osteoarthritis [20] and an increase in perioperative complications [21].
In the cohort of our study, the prevalence of obesity was 12% in total knee arthroplasty and 4.8% in hip arthroplasty, figures considerably lower than those estimated in international studies, where the prevalence of obesity in patients undergoing these surgeries ranges from 36% to 64% [22,23]. Similarly, although a high prevalence of hypertension was observed in knee arthroplasty (56.9%), it fell sharply in patients with hip arthroplasty (25.2%). This suggests underreporting, considering that international studies report prevalences close to 67.8% in mixed cohorts [24]. In the particular case of diabetes, our results show prevalences of 21.7% in the knee and 11.3% in the hip, which is in line with the range reported (11 to 20%) in international series, where a higher frequency is also observed in knee arthroplasty than in hip arthroplasty [25,26,27].
The case of smoking is particularly striking. It was reported in less than 1% of patients, despite the fact that 20% of older adults in Chile report being smokers [28], and international registries have documented a prevalence between 8% and 19% among patients undergoing hip and knee arthroplasty [29,30,31]. This widespread trend of lower recorded prevalence suggests a systematic underreporting of comorbidities in the Diagnosis-Related Groups database. Such underreporting limits the accurate clinical characterization of the beneficiary population and may negatively impact risk estimation, expected outcomes, and resource allocation. This issue is critical considering that all these conditions (obesity, hypertension, diabetes, and smoking) have been associated with higher rates of perioperative complications, including wound infection, sepsis, deep vein thrombosis, pneumonia, increased opioid use, prolonged hospital stay, need for revision surgeries, and higher healthcare costs [25,32,33,34,35,36,37]. In this context, the quality of diagnostic and comorbidity coding plays a central role, as it determines the Diagnosis-Related Groups weight and, consequently, the reimbursement amount received by each institution. Underreporting of relevant conditions such as obesity, diabetes, or smoking may lead to an underestimation of clinical risk and to lower allocation of financial resources. This, in turn, affects perioperative planning and the financial viability of facilities financed through the Diagnosis-Related Groups system. Accurate clinical coding not only enables a more precise reflection of case complexity but also serves as a key tool for fairer resource allocation, grounded in the realities of healthcare delivery.
On the other hand, our results show that it was not until 2023 that the pre-pandemic surgical volume observed in 2019 was reached and exceeded. This delayed recovery reflects the profound impact that the COVID-19 pandemic had on elective surgical activity, particularly in the public system. According to previous analyses, knee arthroplasty decreased by 64% and hip arthroplasty by 41% during 2020, compared to the previous year [38]. Although the system has shown some capacity for recovery, the actual magnitude of the accumulated delay and its effect on the clinical and social outcomes of patients on the waiting list remain unknown.
Additionally, the analysis revealed a high concentration of procedures in a small number of hospitals, with only two facilities performing more than 1,000 total hip arthroplasties and one facility performing more than 1,000 total knee arthroplasties during the analyzed period. On the one hand, high-volume centers tend to have better functional outcomes, prosthesis survival, and lower complication rates [39].
However, this disparity in surgical volume reflects significant inequalities in the public system’s capacity to respond at the territorial level, which translates into gaps in access. In regions with lower surgical volume, patients face additional barriers to access, resulting in longer delays, progression of disability, and a significant functional and socioeconomic impact, especially for those of working age [17,18]. Given these findings, it is essential to move toward a management model that incorporates surgical performance indicators, such as the annual volume of arthroplasties per hospital adjusted for the beneficiary population. This approach would make it possible to monitor regional inequalities, strategically target resources, and establish minimum production standards that guarantee equitable and timely access at the national level.
In addition, the response capacity of low-productivity centers needs to be strengthened through strategies such as training surgical teams, implementing early discharge protocols, and optimizing the use of operating rooms, to improve efficiency without compromising the quality of care [40,41]. The adoption of these standards would also facilitate a more transparent evaluation of institutional performance. In addition, this would generate incentives for continuous improvement and support informed decisions on investment in infrastructure and the provision of specialized human resources.
Another critical aspect identified in our study is related to financing. Our results show that the average reimbursement associated with hip and knee arthroplasty revisions is similar to that of primary arthroplasties, even though the actual cost of a revision is considerably higher [42,43]. The cost of the implant used in revision surgery alone can triple the value of that used in primary surgery, considering the greater surgical complexity and extended hospital stay. This discrepancy has historically created a disincentive for performing complex revisions in the public system. However, in 2025, a specific technological adjustment for arthroplasty revision procedures was approved, which partially remedies the previous financial deficit. This change is consistent with our findings, which show that the average cost observed before the implementation of the adjustment did not reflect the actual technical and economic demands of this type of surgery. Consequently, this new financing policy represents an important step toward greater equity and sustainability in the public health system.
Our study has some limitations inherent to the use of administrative databases. First, data quality depends on the accuracy and completeness of clinical records, as well as on the coding performed at each hospital. This could explain the underreporting observed in specific high-prevalence comorbidities. Second, the Diagnosis-Related Groups database does not include detailed clinical variables such as the type of implant used, the surgical approach, the specific indication for surgery (e.g., fracture versus osteoarthritis), or preoperative functional scales, which limits the analysis of more refined clinical outcomes. Furthermore, the study is limited to procedures performed in public hospitals. Therefore, it does not consider the total volume of arthroplasties financed through other mechanisms, such as private insurance or external agreements with private providers. All of this could underestimate the actual burden of disease at the country level. Despite these limitations, the analyzed information allows for a robust characterization of the public health system’s performance in this area. It provides a valuable basis for guiding coverage policies, resource allocation, and health planning.
Conclusions
This study provides a comprehensive overview of the volume, geographic distribution, clinical profile, and financing situation of primary total hip and knee arthroplasties performed in Chilean public hospitals between 2019 and 2023. The findings show a gradual recovery in surgical volume following the impact of the COVID-19 pandemic. However, marked differences persist between facilities in the number of procedures performed, suggesting regional inequalities in access to this service.
Likewise, demographic analysis revealed a considerable proportion of patients under 65 years of age undergoing total hip arthroplasty, highlighting the functional and economic burden of joint disease in the working population.
Regarding the comorbidity profile, a high frequency of relevant conditions such as hypertension and diabetes was identified. Likewise, there is also evidence of possible underreporting of prevalent conditions such as obesity and smoking, which have direct implications for surgical planning, perioperative risk, and the calculation of Diagnosis-Related Group weights. This limitation in coding could result in an inadequate estimate of the funding allocated.
Finally, the study documents that, until 2025, joint revision procedures were funded similarly to primary surgeries, despite their greater complexity and technical requirements. The incorporation of the technological adjustment in February 2025 for revision and tumor arthroplasties represents a substantial step toward a more equitable allocation of resources that is aligned with clinical reality, contributing to the strengthening of self-management in Chile’s public health system.

