Estudios originales
← vista completaPublicado el 29 de diciembre de 2025 | http://doi.org/10.5867/medwave.2025.11.3114
Desigualdades en salud en Chile post COVID-19: adscripción y acceso efectivo según sexo y condición migrante
Health inequalities in post-COVID-19 Chile: Health system coverage and effective access by sex and migrant status
Abstract
Introduction In 2022, after the COVID-19 pandemic, approximately 93% of the countries in the Region of the Americas continued to report interruptions in essential health services, with worse outcomes in vulnerable social groups. The present study aims to describe barriers to access to health care in Chile, disaggregated by sex and international migrant status.
Methods Cross-sectional study, analyzing the results of the CASEN 2022 survey of persons ≥18 years of age. We calculated ascription, effective access and health barriers by international migrant status and sex. Multiple logistic regression models were performed adjusting for age, rurality, educational level, occupation, and income quintile. The model was expressed as an adjusted Odds Ratio (ORadj) with a 95% confidence interval in STATA v.18.5.
Results For the year 2022 in Chile, a total of 14,767,688 people were represented in this study, with a mean age of 45.4 years (SD: 17.8), 51.2% were women and 9.27% were migrants. Regarding health insurance, 3.11% of the population was not affiliated with the health system, with men (ORadj: 0.6; 95% CI: 0.54-0.68) and immigrants (ORadj: 10.3; 8.78-12.15) being the most affected groups. In terms of effective access, 17.4% had health needs, with a predominance of the female sex (ORadj: 1.3; 95% CI: 1.21-1.32). However, of those who had needs and expressed them, 39.2% expressed unmet needs, with a higher probability of showing it in women (ORadj: 1.2; 95% CI: 1.10-1.27).
Conclusions In Chile, health system coverage remains a challenge for men and the migrant population. We observe with concern high percentages of unmet health needs, particularly among women. The intersection of sex and international migration reveals a dual vulnerability in access to health care that warrants further study.
Main messages
- Affiliation with the health system remains a challenge for males and the migrant population. The intersection of sex and international migration reveals a double vulnerability in access to health care that warrants further study.
- This study is nationally representative and describes the population that reports belonging to a health insurance system, taking into account their main conditions of vulnerability. This facilitates the identification of needs and barriers for evaluating health policies.
- Our results highlight the importance of moving toward more robust studies that inform public policies on how sex interacts with other social determinants within the migrant population.
- The results presented are exploratory in nature and do not imply causality. In addition, the information comes exclusively from heads of households, potentially leading to underrepresentation of the migrant population. Both aspects may limit the projection of the results of this study.
Introduction
In various regions of the world, the COVID-19 pandemic-related health emergency increased barriers to universal access to health care [1,2]. By 2022, approximately 93% of countries in the Americas continued to report disruptions in the response of essential health services [3]. It was estimated that these disruptions could have a greater impact than that caused directly by the COVID-19 pandemic itself [4]. Certain social groups, such as the international migrant population and women, had fewer opportunities to cope with the aftermath of the pandemic and are therefore among the most affected groups [1].
Chile is no exception to this reality. During the COVID-19 pandemic, females faced multiple difficulties, including a higher probability of losing their jobs, taking on additional roles to those they already performed, and returning to work at a slower pace than males [5]. On the other hand, the migrant population, which in 2021 represented 8% of the national population, experienced high levels of socioeconomic precariousness, a greater risk of illness, and a lower probability of being affiliated with a health system [6]. However, knowledge of the context in which these groups operate and the response to the impact of the pandemic on access to public health care in the country, the National Health Fund, remains limited. In this context, it is necessary further to analyze enrollment gaps and effective access to health care.
Effective access occurs when all barriers (economic, organizational, sociocultural, or geographic) that hinder the use of such services have been overcome, allowing people to receive the care they need [7,8].
On the eve of the United Nations Sustainable Development Goals for 2030 [9], the Pan American Health Organization predicts that, after the pandemic, we will see decreases in potential and effective access [3]. In this context, understanding the situation of health coverage in Chile after the pandemic among migrants, especially migrant women, is of vital importance.
In Chile, the National Socioeconomic Characterization Survey (CASEN), conducted by the Ministry of Social Development and Family, has the largest sample size in Latin America [10]. Its objective is to monitor the impact of public policy, taking into account the socioeconomic realities of the population [11]. In particular, it identifies deficiencies and assesses gaps, with special attention to priority groups, such as the migrant population, as measured by the country of birth of the mother [11]. The 2022 National Socioeconomic Characterization Survey is a key tool for identifying gaps in the wake of the health emergency [1]. The present study aims to evaluate access to health care among individuals aged 18 years and older in Chile in 2022, while accounting for sociodemographic variables. The specific objectives are as follows:
-
Measuring access to healthcare among the migrant and Chilean populations
-
Describe access to healthcare by sex.
-
Measure access to healthcare among the migrant and Chilean populations.
-
Measure access to healthcare among the migrant population, broken down by sex.
Methods
Study design
This is a quantitative, observational, cross-sectional study, following the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) checklist guidelines [12]. A secondary analysis was performed using the results of the 2022 National Socioeconomic Characterization Survey [13]. The level of representativeness is national, regional, and by urban/rural areas. The sampling frame was probabilistic, stratified, and two-stage. In the 2022, 72 056 households and 202 231 individuals were interviewed, of whom 106 575 were women and 11 894 were immigrants [11,13].
Participants
This study included responses from individuals aged 18 and older who responded to the 2022 National Socioeconomic Characterization Survey. Individuals without information on their place of birth or who responded to the study variables with "does not remember information" or "does not know" were excluded.
Study variables
Access to health care, divided into affiliation and effective access, was defined as a dependent variable to examine its association with sex, migrant status, and sex by migrant status. Migrant status was assessed by self-reporting the country of residence of the mother at the time of birth (Chilean or international migrant). Affiliation and effective access to the health system were calculated following the methodology of previous studies [14].
Affiliation with the health system
Whether the individual reported having affiliation or not with a health insurance system (yes/no).
Effective access
-
Expressed demand measured by the question: Did you have any health problems in the last 3 months and seek medical attention for this reason? (Yes/no).
-
In the case of unexpressed demand, the main barriers to access were characterized.
-
Satisfied demand measured by the question: Did you encounter any barriers during medical care? (Yes/no).
-
In the case of unmet demand, the main barriers to access were characterized.
The following variables were included: age, rural status, affiliation with the public National Health Fund system (yes/no), educational level (no education, basic, secondary, and higher education), activity (employed, unemployed, inactive), and autonomous income quintile (poorest I, II, III, IV, richest V).
Statistical analysis
To evaluate the association between variables, bivariate analyses were performed using chi-square tests for categorical variables and comparisons of means for quantitative variables. The magnitude and direction of the associations were estimated using multiple logistic regression models, calculating odds ratios for not being enrolled and for not having effective access to the health system, adjusting for age, rural status, educational level, occupational status, and income quintile. The results include 95% confidence intervals. The analysis was performed in Stata v18.5, accounting for the complex sample design using the svyset and svy commands.
Results
In Chile, a total of 15 427 459 people aged 18 and over were represented in the 2022 National Socioeconomic Characterization Survey. After applying the exclusion criteria (4.3%), a total of 14 767 688 people were included in the analysis (Figure 1).
Flow chart of adults aged 18 and over represented in the 2022 CASEN survey.
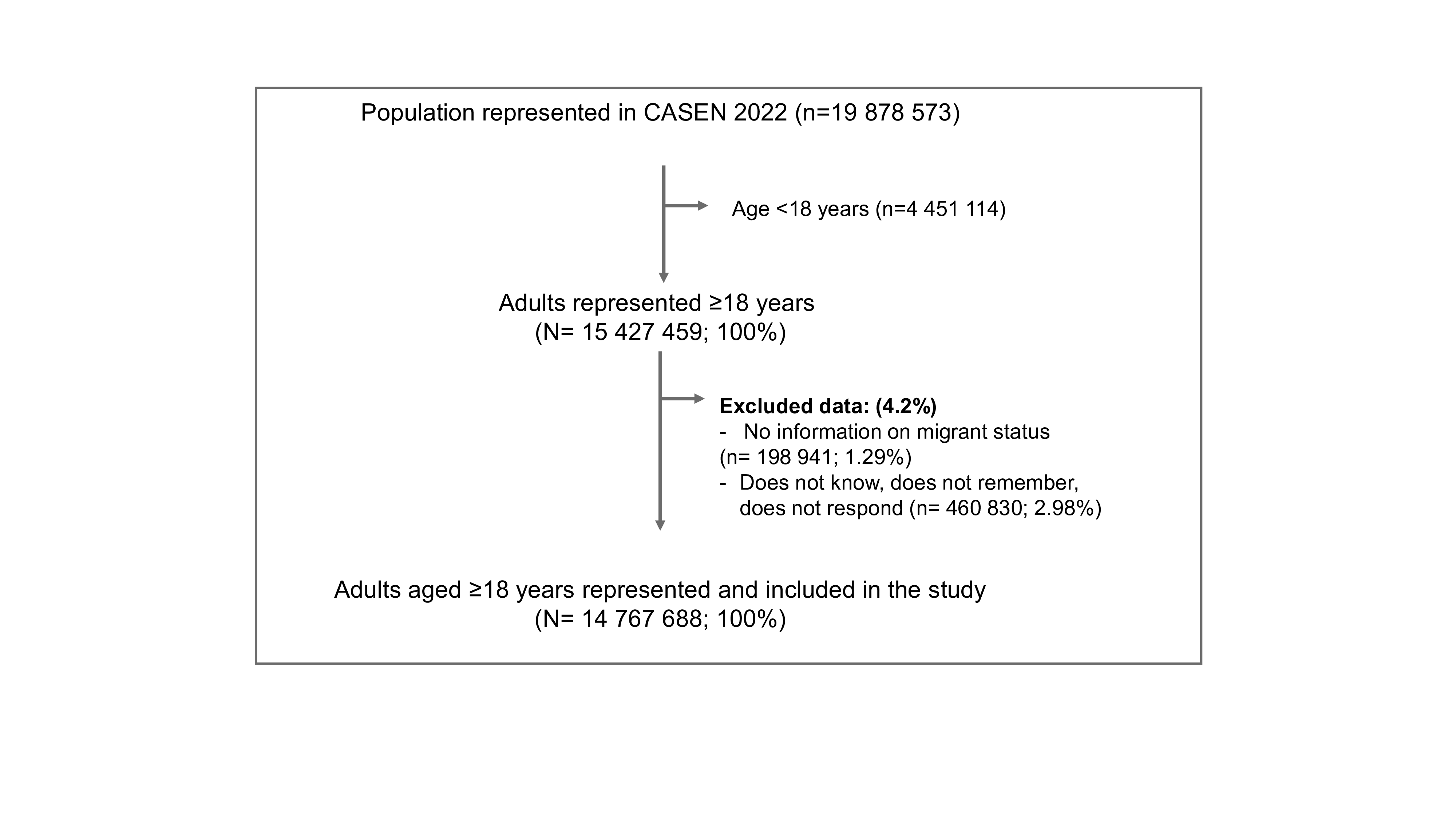
Source: Prepared by the authors based on the study results.
Of the total population included in the study, 51.2% were female, with an average age of 45.4 years (standard deviation = 17.8), and 9.3% were migrants. Most resided in urban areas (88.4%), had a medium- to high-level of education (69.8%), and were employed (59.4%). 96.9% were enrolled in a health care system (Table 1).
17.4% of the population had a health need, of which 89% achieved effective access, and 11% faced barriers to expressing their needs (Figure 2). Having a health need and not having effective access was mainly due to the individual "considering it unnecessary."
Effective access to healthcare for individuals aged 18 and over in Chile, 2022.
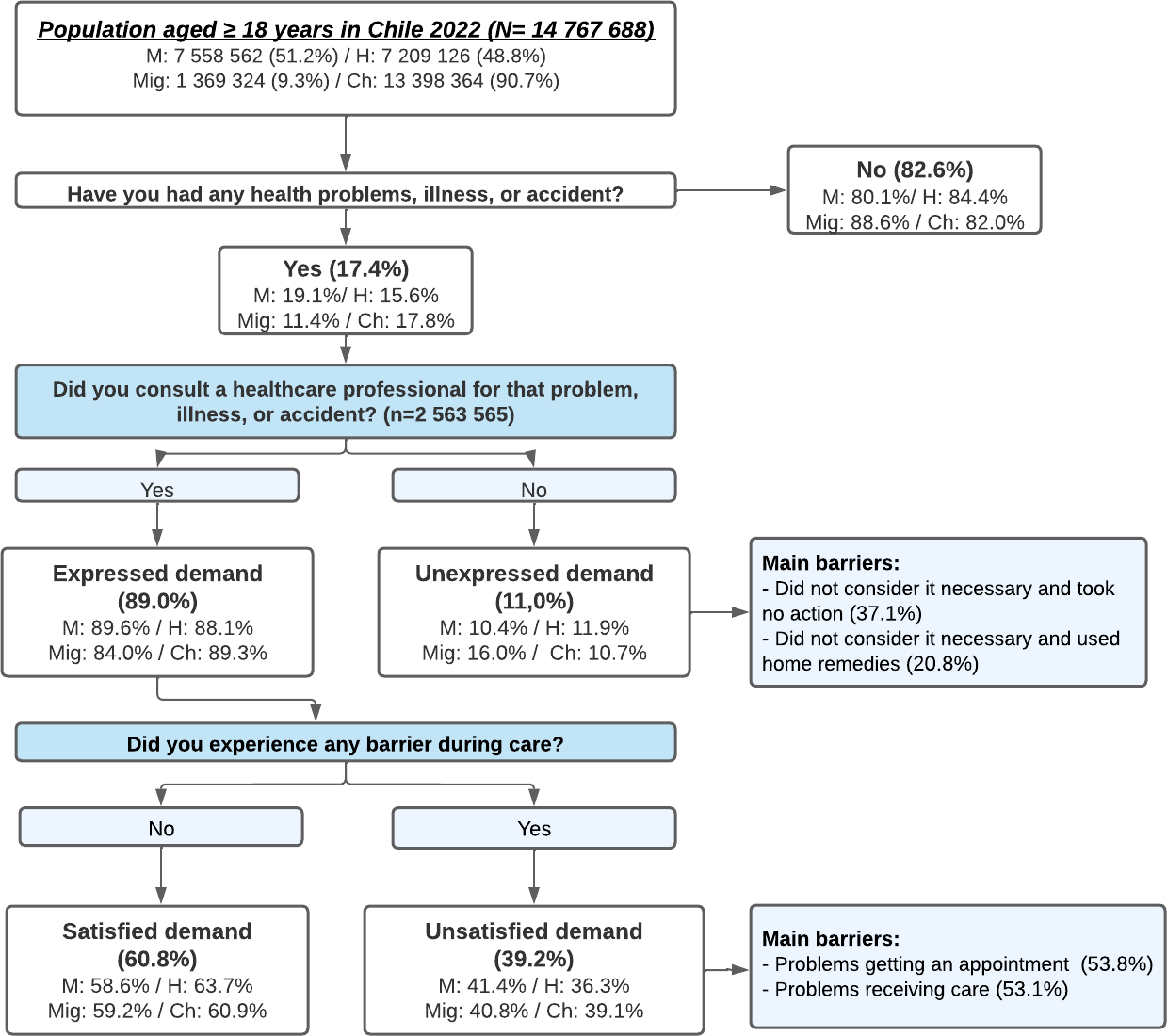
Source: Prepared by the authors based on the study results.
Of the individuals who had effective access (n = 2 280 351), 60.8% reported that their needs were met. The remaining 39.2% reported barriers to care. Most people with unmet demand had problems getting an appointment (53.8%) and receiving care (delays in care, changes in appointment times; 53.1%) (Table 2).
The analysis by sex showed that females were longer-lived, had a lower level of education, with a high percentage of labor inactivity, and belonged to a lower autonomous income quintile than males (Table 1). After adjusted analysis, affiliation in the health system showed that females were less likely to have no affiliation compared to males (adjusted odds ratio: 0.6; 95% confidence interval: 0.54 to 0.68). With regard to effective access, females were more likely to have health needs (illnesses, accidents; adjusted odds ratio: 1.3; 95% confidence interval: 1.21 to 1.32) and less likely to have unexpressed demands (adjusted odds ratio: 0.9; 95% confidence interval: 0.73 to 0.98). However, females were more likely to encounter barriers during care compared to males (adjusted odds ratio: 1.2; 95% confidence interval: 1.10 to 1.27) (Table 3).
In the analysis by migrant status, 51.3% were female. Migrants lived mainly in urban areas, had higher levels of education, and were predominantly in income quintiles III and IV, compared with Chileans (Table 1). After adjustment for affiliation in a health system, migrants were more likely to be uninsured than Chileans (adjusted odds ratio: 10.3; 95% confidence interval: 8.78 to 12.15) (Table 3). Concerning effective access, although migrants were less likely to have health problems (illnesses or accidents; adjusted odds ratio: 0.7; 95% confidence interval: 0.59 to 0.76), when migrants had health needs, they were more likely not to express their needs compared to Chileans (adjusted odds ratio: 1.5; 95% confidence interval: 1.06 to 2.21). No differences were found between migrants and Chileans in the presence of barriers to health care (p = 0.11). Barriers to effective access in migrant and Chilean populations are shown in Table 2.
In the subgroup analysis by migrant status according to sex (n = 1 369 324), the characteristics are shown in Table 1. After adjusted analysis and in relation to enrollment in the health system by migrant status by sex, migrant females were less likely to have no affiliation compared to migrant males (adjusted odds ratio: 0.8; 95% confidence interval: 0.61 to 0.94) (Table 4).
With regard to effective access, no significant differences were found among migrants according to sex (p = 0.45). However, migrant women were less likely than men to express their demands when they arose (adjusted odds ratio: 0.6; 95% confidence interval: 0.37 to 0.90) (Figure 3). No gender differences in barriers to healthcare were observed among the migrant population (p = 0.10).
Inequalities in access to healthcare in Chile following the COVID-19 pandemic.

Source: Prepared by the authors based on data from the study.
Discussion
This study examines the current situation of access to healthcare in Chile following the COVID-19 health emergency, broken down by sex and migrant condition. The main finding is that, despite a significant proportion of people have affiliation in the Chilean health system, some populations remain without affiliation or face barriers to effective access to health care, making them vulnerable. Over the last few decades in Chile, access to health care has undergone significant changes. Specifically, between 2000 and 2010, there was a notable reduction in lack of non-affiliation the health system, narrowing the gap from 11% to 3% [15]. However, despite achieving 97% affiliation and maintaining it over time, even after the pandemic, there is concern about rising barriers to effective access. A study prior to the COVID-19 pandemic reported barrier rates of around 25%, while after the pandemic, we observed a rate of around 40%[16].
Currently, affiliation in Chile’s health insurance system is almost universal, with public insurance predominating. The latter has intensified in recent years, as the population has migrated from the private to the public system [17]. Despite these significant advances, our findings show how men continue to be less likely than women to have affiliation in the insurance system and to seek medical care because they do not consider it necessary. Non-affiliation, predominantly among males, has been reported in Chile since 2000 [14] and has continued even after the pandemic. It is likely that, as in other countries, the cultural construction of masculinity [18] could override the need for medical care. In this construction, men tend to approach the health system only when there is a serious health need or problem [19]. For its part, enrollment in the social security system among the migrant population does not seem to have changed after the pandemic. The high non-affiliation rate remains similar to pre-pandemic levels (2017: 16.3% versus 2022: 15.7%). However, it is crucial to consider that there could be underreporting of post-pandemic information, given the deepening inequalities in the migrant population during the health emergency. In other countries, the COVID-19 pandemic has exacerbated health inequalities in vulnerable populations [20]. This is due to socioeconomic factors and legal, administrative, cultural, and linguistic barriers [2,21].Regarding effective access to healthcare in Chile, robust programs and policies aimed at guaranteeing this right have been implemented over the past few decades. Examples of this include the Explicit Health Guarantees regulated by Laws 19 966 and 20 850 (Ricarte Soto Law). Both constitute concrete mechanisms to ensure access, opportunity, financial protection, and quality of care for specific pathologies and high-cost treatments, regardless of the individual’s socioeconomic status [22,23]. However, the results of this study show that women face greater barriers to health care than men, mainly due to external factors such as difficulties in obtaining medical appointments or affording medication, among others. A greater likelihood of perceiving their health as poor or fair [18] and greater adherence to the health system through preventive and reproductive check-ups for themselves and their families may contribute to women having better self-awareness of their health status. In Chile, women may be moving from a lower likelihood of unmet needs in 1998 [15] to a higher likelihood of unmet medical needs in 2022. A recent study shows that the incorporation of women into the workforce over the last two decades has likely been characterized by precarious work, lower wages, and inflexible hours, hindering access to medical services and appointments [24]. During the pandemic, dissatisfaction with medical needs among women compared to their peers worsened, with a decrease in income and an increase in the burden of care in families, creating problems in paying for care and the cancellation of scheduled appointments. This is particularly noticeable in oncology and cardiovascular consultations compared to their male counterparts [24,25].
The intersection between sex and international migration highlights a double vulnerability in access to health care in these population groups. Although women are more integrated into the health care system, there were no differences in health needs or barriers to care. This could indicate underlying reasons that differ by sex in this population. Our results highlight the importance of advancing more robust studies that will enable the development of public policies focused on how sex interacts with other social determinants in the migrant population.
This study has important limitations that must be considered. The results presented are exploratory and do not imply causality, given the impossibility of evaluating temporal relationships. The information comes exclusively from household heads, and there may be an underrepresentation of the migrant population. However, the survey has important strengths: it allows for analysis with national representativeness, describes the population that declares belonging to a health insurance system, taking into account their main conditions of vulnerability, and facilitates the identification of needs and barriers to evaluate health policies in these groups after the pandemic.
Conclusions
In Chile, affiliation in the health system remains a challenge for males and the migrant population. We note with concern the high percentages of unmet demands, especially among women. The intersection of gender and international migration reveals a double vulnerability in access to health care that warrants further study.

