Estudios originales
← vista completaPublicado el 22 de octubre de 2025 | http://doi.org/10.5867/medwave.2025.09.3129
Explorando el rendimiento muscular axial con actividad de puente en decúbito supino durante la recuperación de la enfermedad crítica: estudio observacional prospectivo
Exploring axial muscle performance with the supine bridging activity across critical illness recovery: A prospective observational study
Abstract
Introduction Limb and respiratory muscle weakness acquired in the intensive care unit (ICU) are commonly associated with long-term functional impairments. However, the extent to which axial muscles might be affected remains poorly understood. Therefore, this study aims to explore the association between axial muscle performance assessed through a supine bridging activity and physical function across critical illness recovery. Secondarily, we investigated the predictability of the supine bridging activity with the walking ability.
Methods Prospective observational study of patients who walked independently before admission and were mechanically ventilated for ≥48 hours in a Chilean medical ICU. The assessment session, conducted on awakening, ICU discharge, and high-dependency unit (HDU) discharge, included the supine bridging activity (performance scored from 0 to 5, with higher scores representing better performance, and lifting duration in seconds) and walking ability. Performance over-time was compared by Friedman’s test for multiple comparisons (Bonferroni corrections). Logistic regressions were used to explore the association of supine bridging activity with in-hospital walking ability. We also produced a Receiver Operating Characteristic curve for the predictability of walking ability.
Results We enrolled 33 adults, completing 86 supine bridging activity assessments across time points. Supine bridging activity performance improved significantly over time, with a median (P25 to P75) of 2 (1 to 4) on awakening, 3 (1 to 5) at ICU discharge, and 5 (2 to 5) at HDU discharge (p<0.001). Higher supine bridging activity scores on awakening were associated with a significantly higher likelihood of walking at HDU discharge (odds ratio: 12.17; 95% CI: 1.36 to 108.68; p=0.025). Lifting >14.5 seconds during the supine bridging activity at awakening predicted walking ability at HDU discharge (area under the curve=0.77).
Conclusions Supine bridging activity performance on awakening was associated with walking ability post ICU discharge, with potential implications on rehabilitation interventions aimed at improving axial muscle strength from early stages of critical illness.
Main messages
- ICU-acquired weakness typically focuses on limb and respiratory muscles, but the role of axial muscles in early recovery remains underexplored.
- This study introduces the supine bridging activity as a pragmatic bedside assessment of axial muscle performance in patients with critical illness.
- A higher bridging score or lifting time at awakening was associated with walking ability.
- The use of a self-selected knee flexion angle enhances clinical applicability and performance sensitivity.
- Limitations include single-center design, small sample size, and the need for clinimetric validation of this novel functional assessment.
Introduction
Intensive care unit acquired weakness is a common complication among patients with critical illness, affecting up to 50% of patients who were mechanically ventilated in the intensive care unit (ICU) [1,2,3]. This condition arises from a combination of muscle atrophy and dysfunction [1,2,4], with studies showing a daily loss of approximately 2% in limb muscle size during the first week of critical illness [4]. Muscle weakness is associated with prolonged ICU and hospital stay, duration of mechanical ventilation, and increased ICU and hospital mortality [3,5,6]. Respiratory muscle weakness, particularly diaphragmatic dysfunction, is frequently associated with prolonged ventilator dependence and difficulty in weaning [7,8]. While changes over time of limb and respiratory muscle weakness have been extensively studied in ICU patients [1,2,3,4,5,6], the association between axial muscles performance and recovery of physical function at early stages of critical illness remains poorly understood, with data limited to imaging findings of trunk muscles [9,10].
Biomechanical and electromyographic studies have demonstrated that trunk muscles are essential for standing, stabilizing the spine while simultaneously preserving static and dynamic balance [11,12]. Prolonged bed rest affects axial muscles in a similar way it affects limb muscles [9,10,13,14,15,16], particularly the erector spinae [10]. Imaging techniques such as computed tomography and magnetic resonance imaging have demonstrated reductions in the size of axial muscles during critical illness, including abdominals, multifidus, psoas major, and erector spinae muscles [9,10,13,17]. Moreover, in hospitalized patients the loss of axial muscle density has been associated with functional impairments [10,17,18]. However, imaging techniques have limited clinical applicability in the ICU setting due to their cost, complexity, and logistical challenges [9].
The supine bridging activity is an in-bed functional task that challenges axial muscles, especially the posterior muscular chain [19,20]. In acute stroke patients with hemiplegia, the test demonstrated good concurrent validity and almost perfect intra and inter-rater reliability, with weighted kappa coefficients of 0.95 (95% CI: 0.88 to 1.00) and 0.98 (95% CI: 0.94 to 1.00), respectively [21]. In hospitalized patients [22], the supine bridging activity showed excellent test–retest reliability, with an intraclass correlation coefficient greater than 0.87 [21,22]. For patients with critical illness, physical functioning measurement instruments have been mainly focused on limb muscles strength and function [3,4,6,23], with the supine bridging activity limited to a sub-item of the De Morton Mobility Index [24] and the Physical Function in Critical Care or PaciFIC tool [25]. However, the supine bridging activity is not routinely assessed in clinical practice, with the axial muscles making an essential contribution to standing and mobilization. Therefore, this study aimed to explore the association between axial muscle performance, assessed through the supine bridging activity, and physical function across critical illness recovery. Moreover, we explored whether axial muscle performance could predict walking ability at discharge. We hypothesized that axial muscle performance, assessed through the supine bridging activity, may be associated with walking ability at discharge in patients recovering from critical illness.
Methods
Study design and setting
This single-center prospective observational study was conducted in a 28-bed medical ICU at an academic Chilean hospital, with follow-up from ICU awakening to the high dependency unit (HDU) discharge. This ICU has, as standard of practice, protocols for sedation, pain management, and ventilator weaning, along with routine physiotherapy interventions such as chest physiotherapy, passive/active mobilization, in-bed and out-of-bed cycling, tilting-table, progressive mobility, and neuromuscular electrical stimulation [26]. The study protocol was approved by the institutional Comité de Ética Científico of Clínica INDISA (#94-08-2022), and written informed consent was obtained from all participants. As an observational study, we followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [27].
Participants
All patients admitted to the adult ICU over a 12-month period were consecutively screened for eligibility. No formal a priori sample size calculation was conducted due to the exploratory nature of this study. We included adult patients (≥18 years old) who were invasively mechanically ventilated for
Definition of the supine bridging activity
The supine bridging activity was evaluated on awakening, ICU discharge, and HDU discharge following a standardized protocol by four trained clinicians (JLG, FMM, NP, CH) with >4 years of clinical experience in the ICU. In this study, the term “axial muscles’” refers trunk extensors and proximal hip extensors, most notably the erector spinae and gluteus maximus, which play a key role in generating and sustaining the bridging position. These postural muscles are involved in stabilizing axial structures during movement and upright transitions [11,12,28,29].
The supine bridging activity was defined as the patient’s ability to lift the pelvis from a fully supine position on a horizontal bed (0° angle) to achieve and maintain a neutral hip flexion angle as the final position. In the standardized starting position, the patient lay supine with knees flexed, feet flat on the surface, toes pointing forward, and arms resting by the sides with palms facing down. From this position, the patient was instructed to actively raise the pelvis until the trunk, pelvis, and thighs formed a straight line, without assistance from the upper limbs. The final posture—neutral hip flexion angle—was held isometrically to assess axial muscle performance. This operational definition was based on previously published descriptions [19,20]. Performance was rated using a six-point scale based on the Medical Research Council Sum Score [30], with higher scores indicating better performance. Scores from 0 to 3 were based on the degree of visible muscle contraction and the ability to move against gravity, while scores 4 and 5 were based on the duration (in seconds) of patient maintaining an isometric maximal elevation in the final position (
Additional in-hospital physical functioning outcomes
We also evaluated limb muscle strength and mobility at three time points: on awakening, ICU discharge, and HDU discharge. Limb muscle strength was measured using the Medical Research Council Sum Score, following the standard protocol [30]. The Medical Research Council Sum Score assesses six bilateral muscle groups (shoulder abduction, elbow flexion, wrist extension, hip flexion, knee extension, and ankle dorsiflexion), each scored from 0 (no visible contraction) to 5 (normal strength), with a total possible score ranging from 0 to 60. To characterize the distribution of muscle weakness, we analyzed Medical Research Council Sum Score score grouped by upper limbs, lower limbs, right side, left side, proximal (shoulder abduction and hip flexion) and distal (wrist extension and dorsiflexion) muscles.
Mobility was assessed using the Chilean version of the Functional Status Score for the ICU [32]. The Functional Status Score for the ICU includes five items—rolling, supine to sit transfer, sitting at the edge of the bed, sit to stand transfer, and walking—each scored from 0 (unable to perform) to 7 (complete independence), for a total score ranging from 0 to 35. Walking ability was defined as a score >2 in the walking item and sit-to-stand ability as a score >1 in the corresponding item. We measured the Short Physical Performance Battery [33] at HDU discharge when the patient was able to perform all components of the test without requiring physical assistance from clinical staff. The Short Physical Performance Battery includes three items: standing balance tests, 4-meter walking speed, and five-times sit-to-stand; each item is scored from 0 to 4, with a maximum total score of 12. These instruments were chosen to address complementary constructs of physical recovery: axial muscle performance (supine bridging), muscle strength (Medical Research Council Sum Score), ICU mobility (Functional Status Score for the ICU), and global physical function at discharge (Short Physical Performance Battery).
Data extraction and analysis
Clinical and baseline variables were extracted from the electronic clinical records including age, gender, body mass index, baseline Clinical Frailty Scale, Charlson Comorbidity Index, Sequential Organ Failure Assessment at ICU admission, admission diagnosis, duration of mechanical ventilation, and ICU and hospital length of stay.
Descriptive statistics were used to summarize patient characteristics and outcomes. Categorical variables were reported as frequencies (n) and percentages (%), while results from physical assessments (i.e., supine bridging activity score and lifting times, Medical Research Council Sum Score, Functional Status Score for the ICU and Short Physical Performance Battery scores) were reported as medians with percentile 25 and percentile 75 (P25 to P75) due to their ordinal nature and non-normal distribution. Performance over time was compared using a Friedman’s test with correction for multiple comparisons (Bonferroni), and p-values below 0.01 indicating significance. Using the Mann-Whitney test, we compared the physical function on awakening by the ability to walk (i.e., Functional Status Score for the ICU score>2 in the walking item) and the ability to perform a sit-to-stand transition (i.e., Functional Status Score for the ICU score>4 in the sit-to stand item) on awakening. Additionally, we compared physical function on awakening by ability to walk at HDU discharge.
The correlation between the supine bridging activity (as a score and duration in seconds) and muscle strength and physical function were assessed using Spearman rho correlation coefficients. Spearman rho correlation coefficient was interpreted as little (0.00 to 0.25), weak (0.26 to 0.49), moderate (0.50 to 0.69), strong (0.70 to 0.89), and very strong (0.90 to 1.00) correlation [34].
With an exploratory approach, logistic regressions were used to determine the association of supine bridging activity score and lifting time with in-hospital physical function. Additionally, we estimated the predictive ability of supine bridging activity on walking ability as an outcome, defined in two ways: >2 points and >1 point in the walking Functional Status Score for the ICU item; both indicating the ability to walk at least 15 meters with physical assistance. We also produced a Receiver Operating Characteristic curve to show the proportion of individuals correctly classified by different lifting times/scores in the supine bridge activity. Analyses were performed using all available data at each assessment point (awakening, ICU discharge, HDU discharge). All statistical analyses were performed using Stata MP version 18.0 (StataCorp, College Station, TX, USA).
Results
Between October 2022 and October 2023, a total of 1074 adults were admitted to the ICU. Of these, 431 required invasive mechanical ventilation, with 33 patients being enrolled in the study (
Flow diagram of study participants.
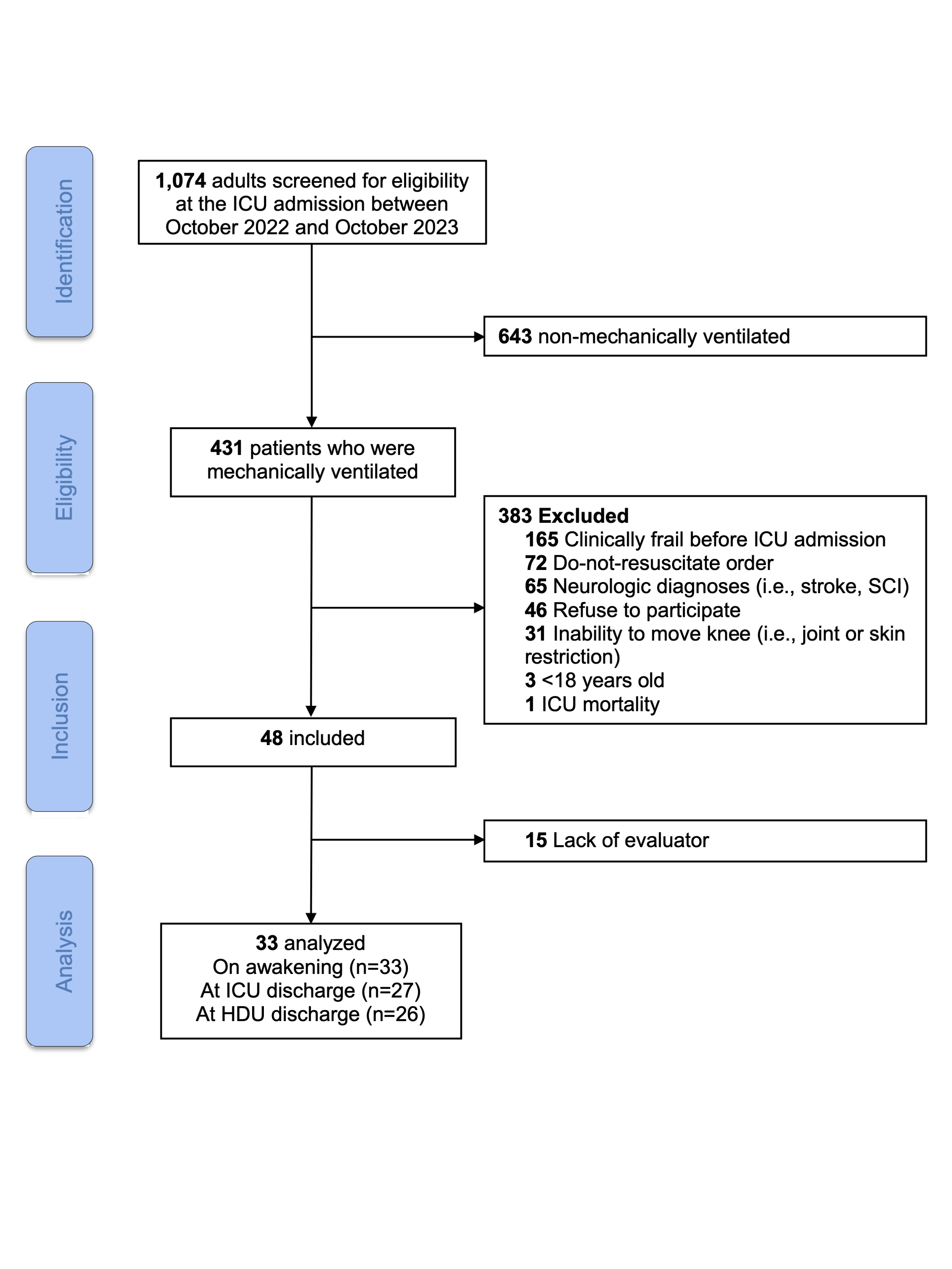
Source: Prepared by the authors of this study.
Overall, supine bridging activity, limb muscle strength, and physical function variables showed significant increases across time-points (
Both scoring and lifting time of supine bridging activity on awakening had mostly moderate to strong significant correlations with Medical Research Council Sum Score, Functional Status Score for the ICU, and Short Physical Performance Battery score (Table 3).
Spearman’s rho values of supine bridging activity ranged from 0.64 to 0.74 with muscle strength variables and from 0.46 to 0.73 with physical function. The Short Physical Performance Battery at HDU discharge showed a non-significant and weak correlation with the supine bridging activity score on awakening (rho=0.41), but significant correlation with the supine bridging activity lifting time (rho=0.60).
Patients who were unable to walk at HDU discharge presented significant differences (p < 0.01) in supine bridging free knee flexion score as well as in limb muscle strength and physical function at awakening, compared with those who were able to walk (Functional Status Score for the ICU walking item > 2).
Importantly, all individuals scoring ≥3 in the supine bridging activity with free knee flexion at awakening walked at HDU discharge, while 75% of those scoring <3 did not, reinforcing the clinical value of this early in-bed measure as a functional indicator (Table 4).
Similarly, in-bed physical performance differed significantly at awakening between patients stratified by their ability to walk and stand. Those who were able to walk (Functional Status Score for the ICU >2) or stand (Functional Status Score for the ICU >4) exhibited higher supine bridging activity free knee flexion scores, longer lifting times, and greater proximal and distal muscle strength, reflected by higher Medical Research Council Sum Scores. They also showed better performance in early functional tasks, including rolling and transitions from supine to sitting (
All patients who achieved good performance in the supine bridging activity (scoring ≥3) on awakening were able to walk at HDU discharge, while 75% of patients not able to lift pelvis against gravity (<3 points) on awakening were not able to walk at HDU discharge (p=0.01). Similarly, all patients who achieved good performance in the supine bridging activity (scoring ≥3) on awakening were able to sit-to-stand without physical assistance at HDU discharge (p=0.06). A score ≥3 in supine bridging activity on awakening were associated to higher odds of walking (Functional Status Score for the ICU >2) at HDU discharge (odds ratio [95% CI] = 12.2 [1.4 to 108.7]; p=0.025).
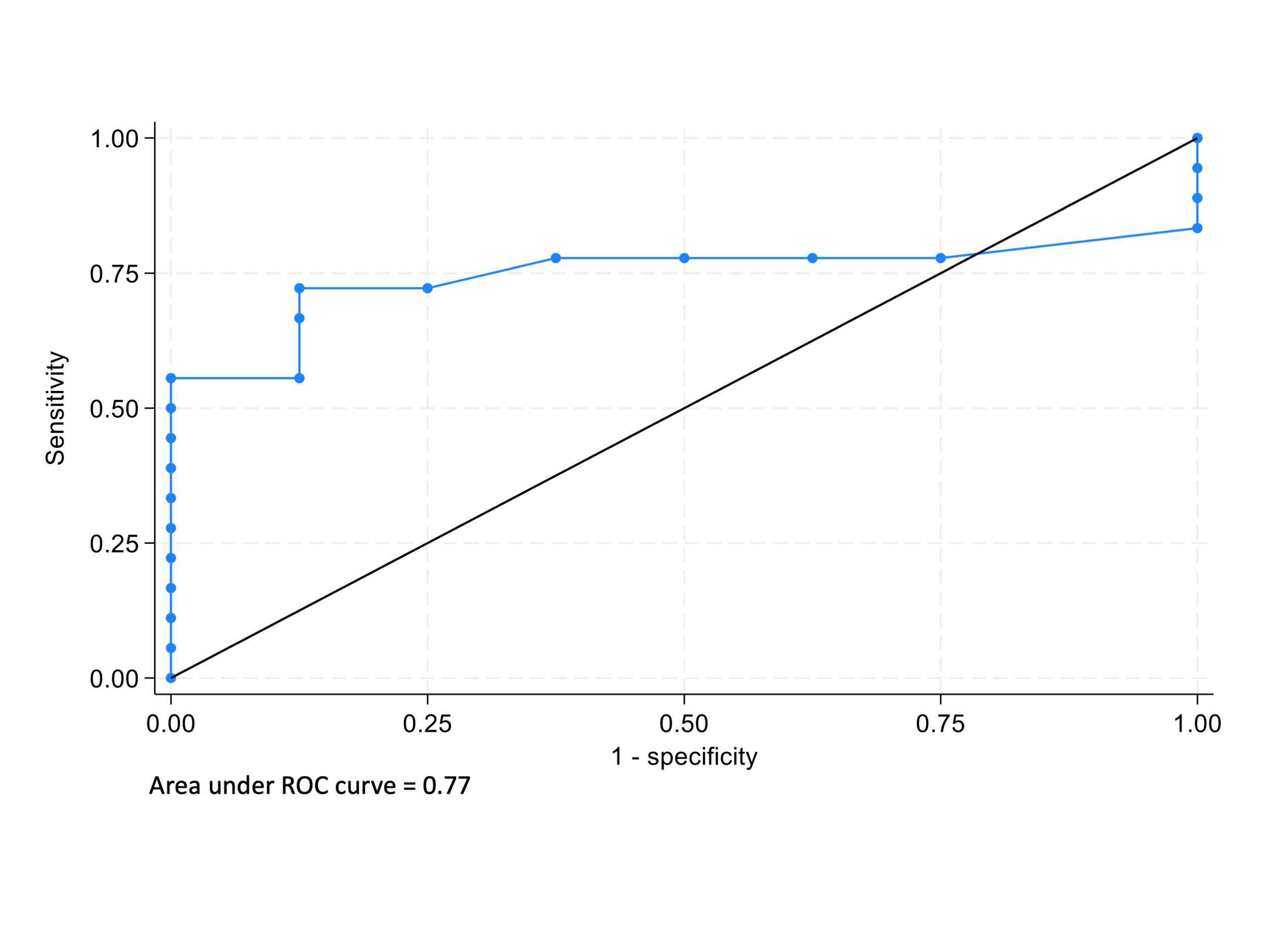
We explored the accuracy of the supine bridging activity lifting time on awakening for predicting being able to walk at HDU discharge using two cut-off points of the Functional Status Score for the ICU walking item: a score >1 and a score >2. The lifting time during supine bridging activity on awakening revealed significant predictability of walking ability when defined by Functional Status Score for the ICU walking item>1 at HDU discharge (area under the curve =0.77), with 14.5 seconds of lifting time as cutoff (sensitivity=68%, specificity=86%) (
Receiver operating characteristic (ROC) curve with sensitivity and specificity of the supine bridging activity on awakening for predicting the ability of walking at high dependency unit discharge, defined as Walking Functional Status Score for the ICU item >1.
Discussion
This prospective observational study provides novel evidence on the value of assessing axial muscle performance early in the recovery of patients with critical illness by using a clinical and simple in-bed supine bridging activity. Our findings show that both the score and lifting duration of the supine bridging activity improved significantly over time and was moderately to strongly associated with limb muscle strength and physical function assessments. Both lower scores and shorter lifting times of the supine bridging activity were associated with lower likelihood of achieving the sit-to-stand transition and walking, suggesting its potential value as an early functional measure for guiding physical rehabilitation strategies in the ICU.
In the context of intensive care unit acquired weakness, the association between decreased limb and respiratory muscles strength and long-term functional limitations is well-established [1,3,5,6]. However, axial muscles have received comparatively limited attention despite their essential role in balance, trunk control, and transfer activities [10,11,12,28]. Our findings extend prior imaging-based evidence on trunk muscle wasting [9,10,13,15,16] by offering a pragmatic and bedside performance-based measure that can be used in routine ICU care without the practical constraints of advanced imaging modalities. The supine bridging activity was associated with physical function, with lifting durations above 14.5 seconds suggesting patients likely to walk at least 15 meters at HDU discharge. This aligns with literature supporting the prognostic value of early in-bed mobility outcomes for discharge readiness and physical functioning [25,30,35,36].
Notably, supine bridging activity is underutilized in ICU assessment tools, often appearing as a sub-item within broader indices like De Morton Mobility Index and Physical Function in Critical Care tool [24,25], where supine bridging is evaluated as binary variable (able/unable). Our assessment approach allows for a more detailed evaluation of the patient’s performance by an ordinal scale from 0 to 5 and adding a time limit when the patient achieved the final bridging position. This is consistent with current published studies with novel data on supine bridging activity in similar populations such as the Bed Bridge Test for general medical inpatients [22] and Functional Bridge Test for patients after a stroke [21].
This is the first study evaluating supine bridging activity performance in patients with critical illness. While the Bed Bridge Test in hospitalized patients demonstrated strong test–retest reliability (Intraclass Correlation Coefficient >0.87) and moderate-to-strong correlations with Short Physical Performance Battery and sit-to-stand test [22], and the Functional Bridge Test in acute stroke showed excellent inter- and intra-rater reliability (κ=0.95 to 0.98) [21], our findings explored the accuracy of supine bridging activity lifting time to predict walking and sit-to-stand ability at HDU discharge. As expected, Bed Bridge Test showed similar correlation values against Short Physical Performance Battery and sit-to-stand test (rho=0.47 to 0.64) compared to our supine bridging activity against the same variables (rho=0.41 to 0.63). However, the correlation between bridging activity and Functional Status Score for the ICU was lower for Bed Bridge Test (rho=0.27 to 0.37) compared to our supine bridging activity (rho=0.59 to 0.69) [22]. This can be explained because Functional Status Score for the ICU is a scale developed for the ICU setting, with higher ceiling and floor effects in hospitalized patients without critical illness [37].
From a biomechanical point of view, our study allowed patients to perform the supine bridging activity with a median [P25 to P75] self-selected knee flexion angle of 105° [100 to 110], reflecting individualized biomechanics and functional strategies in patients with critical illness. However, both Bed Bridge Test and Functional Bridge Test used fixed knee angles (45° and 120°, respectively) [21,22]. Indeed, we found higher performance across time-points when supine bridging activity was carried out with a self-selected knee flexion angle compared with 90°-fixed knee angle. Biomechanical and electromyographic reports indicate that a knee flexion angle of 90° represents a biomechanical equilibrium, as it effectively reduces lumbar spine loading without significantly increasing stress on the hip joint [31,38,39]. At this angle, the gluteus maximus and adductor magnus exhibit substantial activation, while the involvement of the biceps femoris and spinal erectors remains moderate, thereby preventing excessive muscular demand. In our sample, the preference for a greater knee flexion angle (with a median of 105°), which was also associated with improved performance, may reflect a compensatory strategy that promotes increased recruitment of the hip extensor muscles. These muscles show progressively greater activation at flexion angles beyond 90°, while the spinal erectors display a concomitant decline in activity [31,38,39], suggesting a redistribution of axial effort as the knee flexion angle increases. The use of a self-selected knee flexion angle in this study, closely mimics the functional adaptations patients use during recovery, compared to standardized fixed angles that may not reflect real-world biomechanics.
This study is not free from limitations. First, the single-center design and modest sample size limit generalizability; therefore, replication in diverse ICU settings is needed. The exclusion of frail patients and those with neurologic conditions restricts applicability to lower-risk populations. Second, we did not evaluate respiratory muscles, providing a partial view of muscle recovery over time by including the assessment of axial and limb muscles. Third, while this study provides preliminary predictive validity, the clinimetric properties of the supine bridging activity—including validity, reliability, responsiveness, measurement error, and minimal important difference—remain to be established for patients with critical illness. Fourth, the HDU discharge is an intermediate or transition unit that may not be equivalent to hospital discharge in other countries, limiting the interpretation of functional findings at HDU discharge. However, in this study the median difference between the HDU discharge and hospital discharge was 2 days. Finally, the observational nature of the study also precludes causal inference. Nonetheless, these findings underscore the need to integrate axial muscle performance into ICU physical rehabilitation paradigms.
Conclusions
Axial muscle weakness, evaluated clinically in bed and early in the ICU via the supine bridging activity, showed improvements over time during the hospital stay and may help identify patients with delayed mobility recovery (walking and sit-to-stand) before hospital discharge. These preliminary findings should be interpreted with caution and may support rehabilitation interventions aimed at strengthening axial muscles from early stages of critical illness. Future studies are needed to confirm these associations and to evaluate the clinimetric properties of the supine bridging activity to guide ICU physical rehabilitation strategies.

