Estudios originales
← vista completaPublicado el 22 de diciembre de 2025 | http://doi.org/10.5867/medwave.2025.11.3135
Predictores clínicos y relacionados con las heridas para la estancia hospitalaria prolongada en infecciones del pie diabético en un entorno de recursos limitados: un estudio de cohorte retrospectivo
Clinical and wound-related predictors for prolonged hospital stay in diabetes-related foot infections in a resource-limited setting: A retrospective cohort study
Abstract
Introduction Diabetes-related foot infections are a common cause of hospitalization and are associated with prolonged hospital stays, higher healthcare costs, and poor outcomes. However, information on clinical risk factors for prolonged hospital stay in resource-limited settings is scarce. The aim of this study was to identify clinical factors associated with prolonged hospital stay in patients hospitalized for diabetes-related foot infection.
Methods We conducted a retrospective cohort study of patients admitted with diabetes-related foot infection at Hospital Nacional Alberto Sabogal Sologuren part of the Peruvian Social Security system, between 2020 and 2021. Clinical characteristics, wound features, and treatment types were collected from electronic medical records. Prolonged hospital stay was defined as more than 10 days according to national guidelines. Associations with prolonged hospital stay were assessed using Poisson regression with robust variance.
Results A total of 228 patients were included (76.3% male; median age: 66 years). The most frequent comorbidities were atherosclerotic cardiovascular disease (56.6%), arterial hypertension (54.8%), and chronic kidney disease (42%). Overall, 50.5% of patients were treated with bedside wound debridement; 25.4% underwent minor amputation; and 24.1% received surgical management (major amputation or operating-room debridement). Prolonged hospital stay occurred in 49.6% of patients. Independent risk factors included wound length >5 cm (adjusted relative risk: 1.63; 95% confidence interval: 1.17 to 2.26), surgical management (1.63; 1.40 to 2.97), minor amputation (1.63; 1.22 to 2.63), and a history of atherosclerotic cardiovascular disease (1.63; 1.08 to 1.84).
Conclusions Nearly half of patients with diabetes-related foot infection experienced prolonged hospital stay. Larger wound size, surgical treatment, minor amputation, and atherosclerotic cardiovascular disease were associated with prolonged hospitalization. Identifying these factors may guide clinical decisions to reduce hospital stays in resource-limited health systems.
Main messages
- Prolonged hospital stay is a common and costly complication among patients with diabetes-related foot infections.
- This study identifies specific patient- and wound-related predictors of prolonged hospitalization in a resource-limited setting where access to vascular treatments is restricted.
- History of atherosclerotic cardiovascular disease, wound length > 5 cm, and undergoing minor amputation or surgical treatments (major amputation or debridement) were independently associated with hospital stay longer than 10 days.
- As a single-center retrospective cohort, our findings have limited generalizability; however, early identification of these predictors may improve management and outcomes of diabetes-related foot infection in similar resource-limited settings.
Introduction
Diabetes-related foot infection is a serious complication of diabetes mellitus, affecting about 6% of individuals worldwide [1]. Up to 25% of people living with diabetes will develop a diabetes-related foot infection during their lifetime [2], which accounts for more than 50% of non-traumatic lower-limb amputations [3]. In Latin America, diabetes-related foot infections account for nearly 20% of diabetes-related hospital admissions [4], and in Peru, their prevalence among general admissions is approximately 3% [5].
Beyond the impact on morbidity and mortality [6,7], diabetes-related foot infections represent a significant financial burden for patients and healthcare systems [8,9]. In Peru, the cost attributable to these infections was estimated at USD 74.5 million in 2012 [9]; at the national level, the total economic burden related to diabetes mellitus care was USD 15.4 billion in 2019 [10]. The high costs are largely driven by hospital admissions, diagnostic tests, complex and multidisciplinary treatments, and prolonged hospital stays [11,12].
Prolonged hospitalization is common among patients with diabetes-related foot infections [13]. Although most prior studies used non-standardized definitions of prolonged hospital stay [14,15], they consistently reported associations with ulcer severity, inflammatory markers, glycemic control, surgical management, and cardiovascular comorbidities. In Peru, the Social Security system (EsSalud) recommends a 10-day hospital stay for general admission [16]. Evidence from low- and middle-income countries remains limited, particularly in hospitals where access to vascular treatments is limited, remains scarce and may influence outcomes.
Understanding the factors associated with prolonged hospitalization in this context is relevant for improving clinical outcomes and optimizing hospital efficiency. This study aimed to identify factors associated with prolonged hospital stays (>10 days) among patients admitted for diabetes-related foot infections at a tertiary hospital within the EsSalud system in Peru. Specifically, we sought to examine patient characteristics, wound features, and treatment types in relation to length of hospital stay.
Methods
Study design and population
This was a retrospective cohort study including patients aged 18 years or older who were hospitalized for diabetes-related foot infection in the diabetic foot unit of the endocrinology department at Hospital Nacional Alberto Sabogal Sologuren, a tertiary hospital within the EsSalud system, between 2020 and 2021.
Patients were excluded if they had been transferred from another hospital, referred to another facility or intensive care unit due to medical complications, or diagnosed with COVID-19 infection, as these conditions could independently prolong hospital stay [17]. Additional exclusion criteria included voluntary discharge against medical advice, in-hospital death, or admission for elective procedures (e.g., angioplasty or arteriography).
Data source and variables
Data were extracted from electronic medical records using the EsSalud Intelligent Health System (ESSI, acronym in Spanish) platform. A comprehensive chart review was conducted to confirm eligibility and extract the variables of interest.
The primary outcome was prolonged hospital stay, defined as a stay of more than 10 days according to EsSalud standards [16]. Length of stay was calculated from admission to the Diabetic Foot Unit until hospital discharge. Independent variables considered as potential predictors included patient-related factors, wound-related factors, and the type of definitive treatment for diabetes-related foot infection.
Patient-related variables included age, sex, duration of diabetes mellitus, and comorbidities such as hypertension, chronic kidney disease (classified as non-end-stage or end-stage), established atherosclerotic cardiovascular disease (documented myocardial infarction, cerebrovascular disease, or peripheral artery disease), and previous major amputation due to diabetes-related foot infection.
Wound-related variables included duration of infection before admission, wound length, documented osteomyelitis, and wound severity according to the Wound, Ischemic, and Foot Infection (WIFI) classification as recorded in the medical charts. Given the heterogeneity of diagnostic methods for peripheral artery disease (ankle-brachial index, arterial Doppler ultrasound, computerized angiography, or arteriography) and incomplete data, the ischemia component of the WIFI classification was dichotomized as present or absent. We also documented the interval from emergency admission to initial wound debridement.
The type of definitive treatment for diabetes-related foot infection was determined by a multidisciplinary diabetic foot team led by endocrinologists and including vascular surgeons and orthopedic specialists, based on wound severity, comorbidities, and vascular status. All patients underwent initial bedside wound debridement. Definitive treatment was categorized into three mutually exclusive groups based on the most invasive intervention:
Bedside wound debridement only: Debridement of necrotic tissue using a scalpel, with or without adjunctive dressing therapy.
Bedside minor amputation: Amputation of one or more toes performed at the bedside, typically by the endocrinology team.
Surgical management: Any procedure performed in the operating room, including surgical debridement or major amputation (midfoot and below or above the knee).
Statistical analysis
Categorical variables were reported as absolute and relative frequencies. Continuous variables were summarized as medians with interquartile ranges. Missing data were minimal; therefore, no imputation procedures were applied, and analyses were conducted using available cases.
To explore baseline differences between patients with and without prolonged hospital stay, bivariate analyses were performed using Chi-square or Fisher’s exact test for categorical variables and the Kruskal-Wallis test for continuous variables. Results were reported with p values only.
For regression analysis, variables without predefined clinical cutoffs (age, duration of diabetes, duration of wounds, time of initial debridement, and wound length) were categorized into tertiles. Associations with prolonged hospital stay were examined using Poisson regression with robust variance, and results were presented as crude and adjusted relative risks with 95% confidence intervals. Variables with p < 0.2 in the bivariate analysis were included in the multivariable model. Because WIFI data were missing for four individuals, a complete-case approach was applied for multivariable analyses, and those participants were excluded from the corresponding models. Model fit was assessed using deviance and Pearson goodness-of-fit tests. Deviance and Pearson residuals were examined to detect outliers. Leverage values from the equivalent Poisson GLM without robust variance were used to identify influential observations.
Multivariable analyses were stratified into two models: one with patient-related factors and another with wound-related factors. This approach was adopted to reduce the risk of overfitting, given the sample size, and to allow for more straightforward interpretation of predictors at both the patient and wound levels. All statistical analyses were conducted using Stata v16.
Because the type of definitive treatment demonstrated the strongest association with prolonged hospital stay, it was included as part of an exploratory analysis of the patient-related model to assess its clinical influence (Supplementary Table S1). To maintain parsimony and avoid overfitting, the wound-related model was restricted to wound-specific factors and did not incorporate additional patient-related variables.
To assess the robustness of our findings, sensitivity analyses were performed using other definitions of prolonged hospital stay: ≥16 days (75th percentile of our cohort) and ≥21 days, consistent with the definition used in a previous study [18].
Ethics
This study was approved by the Ethics Committee of Hospital Nacional Alberto Sabogal Sologuren (MEMORANDO N°444-CIEI-OlyD-GRPS-ESSALUD-2022). Patient confidentiality was preserved by removing all personal identifiers after data collection.
Results
Between January 2020 and December 2021, a total of 278 patients were hospitalized with diabetes-related foot infections. Fifty patients were excluded (Figure 1), including two who died from sudden cardiac arrest during hospitalization; both had end-stage renal disease. Thus, data from 228 patients were included in the final analysis.
Flow of patients included in the study.
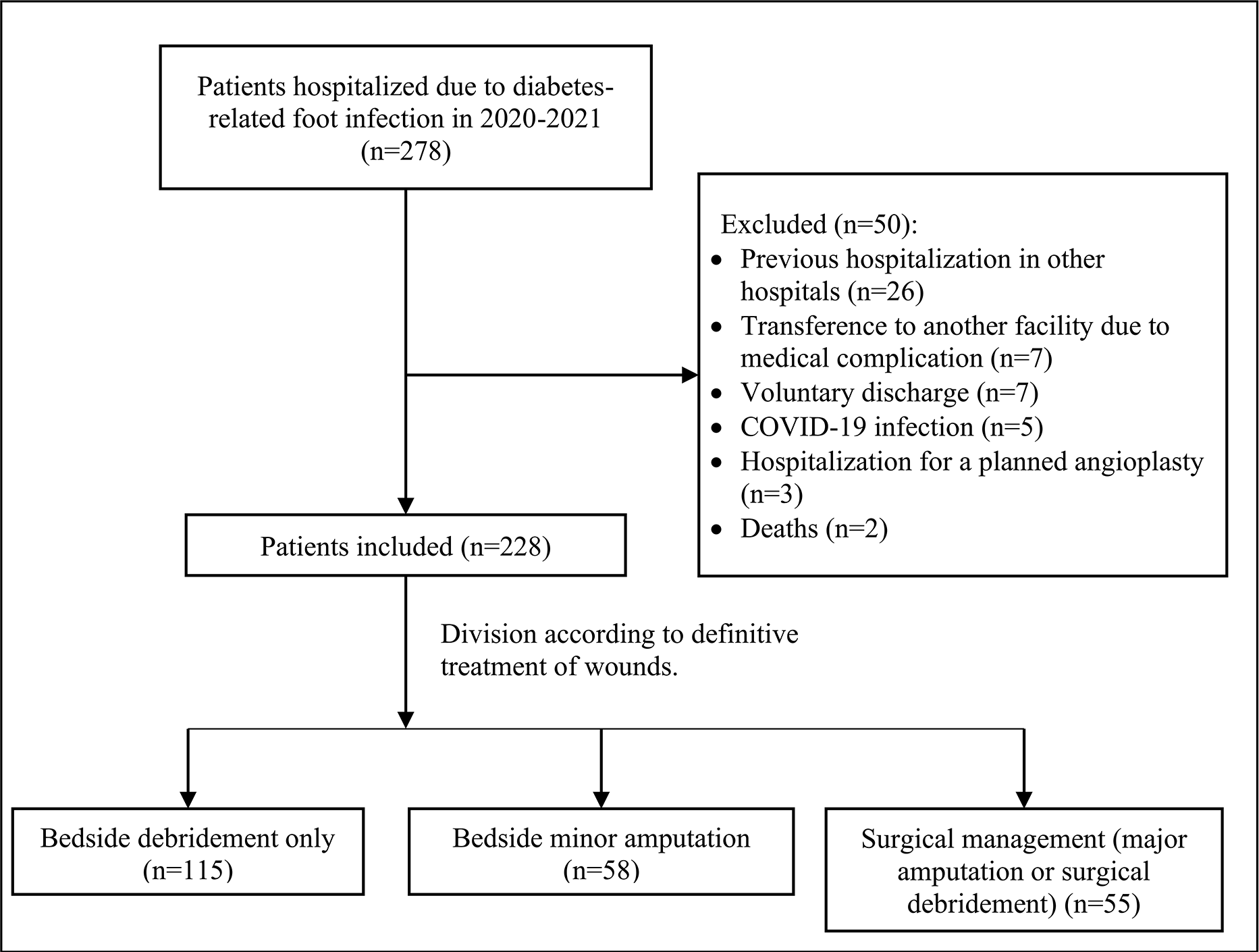
Among them, 76.3% were male, with a median age of 66 years (interquartile range: 57 to 73.5). Atherosclerotic cardiovascular disease was reported in 56.6% of patients, hypertension in 54.8%, chronic kidney disease in 42%, and a history of major amputation due to diabetes-related foot infection in 11.4% (Table 1).
Table 2 shows the characteristics of diabetes-related foot infections by hospital stay length. The median wound length was 3.5 cm (interquartile range: 2 to 6). Osteomyelitis was reported in 68% of patients, and peripheral artery disease in 59.8%. Regarding the type of definitive treatment, 50.5% were managed with bedside debridement only, 25.4% underwent minor amputation, and 24.1% required surgical interventions performed in the operating room, including major amputation (41 patients, 18%) or surgical debridement (14 patients, 6.1%). Eight patients (3.5%) underwent angioplasty during hospitalization, and none received surgical revascularization.
The median length of stay was 10 days (interquartile range: 6 to 16), with 49.6% of patients staying more than 10 days. Length of stay varied significantly by type of definitive treatment (p < 0.001; Figure 2).
Box and whisker plot of hospital stay by type of definitive treatment of diabetes-related foot infection.
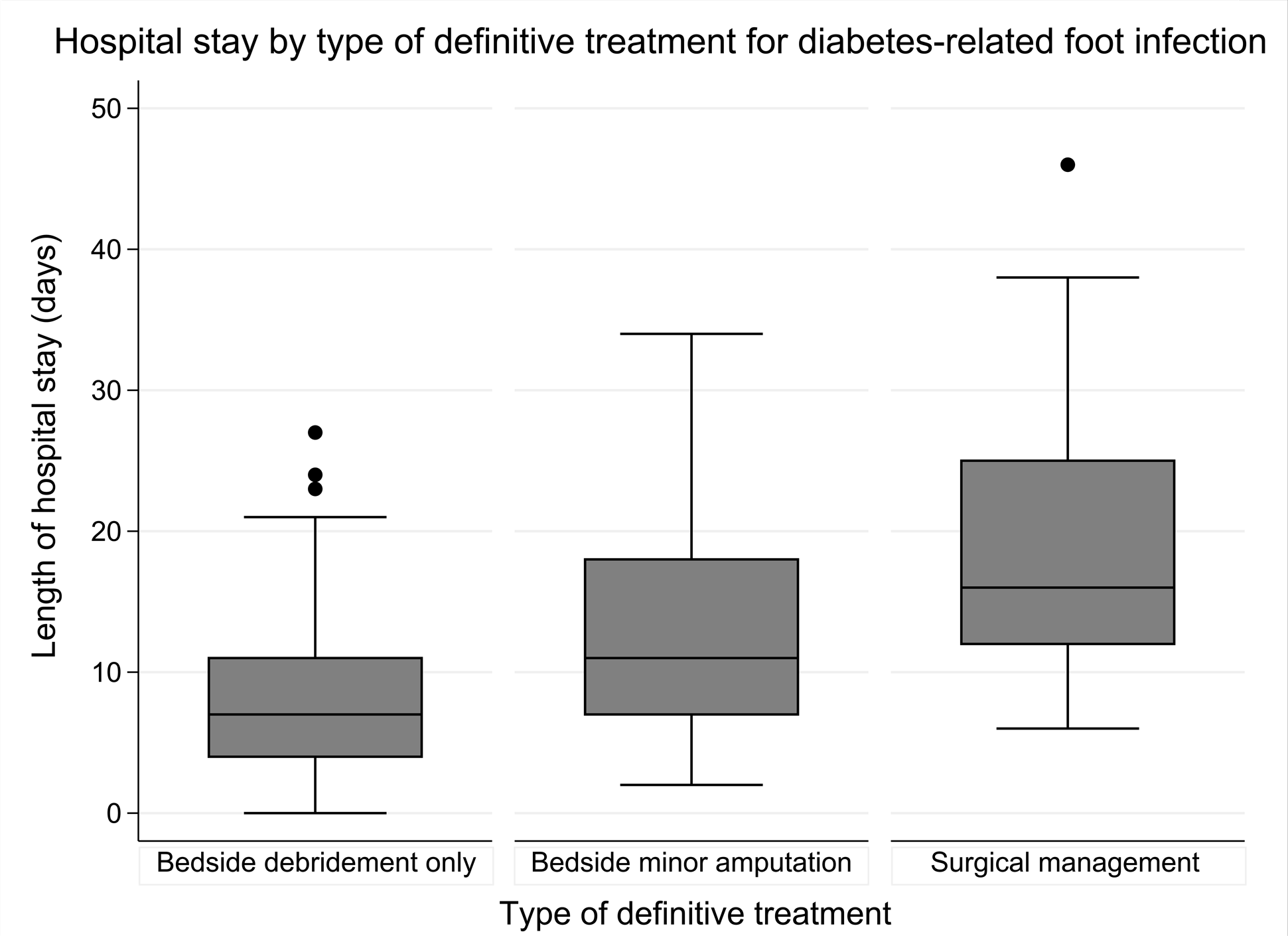
Patients who were managed with bedside debridement only had a median hospital stay of 7 days (IQR: 4 to 11); those who underwent bedside minor amputation had 11 days (IQR: 7 to 18), and patients who had major amputation or surgical debridement had 16 days (IQR: 12 to 25) (these data are not shown in the tables).
In the multivariate analysis (Table 3), a history of atherosclerotic cardiovascular disease was independently associated with prolonged hospital stay (adjusted relative risk: 1.4; 95% confidence interval: 1.08 to 1.84). Although younger patients (<60 years and 60 to 70 years) initially showed a higher risk of prolonged hospitalization, these associations lost statistical significance after adjusting for the type of definitive treatment, which was included as part of an exploratory analysis. Specifically, being younger than 60 years (ARR: 1.33; 95% CI: 0.97 to 1.81) or those aged 60 to 70 years (aRR: 1.25; 95% CI: 0.91 to 1.71) were not significantly associated with prolonged hospital stay compared to those older than 70 years (Supplementary Table S1).
Similarly, no significant associations were found between prolonged hospitalization and patient sex or prior major amputation.
Among wound-related variables (Table 4), a wound length greater than 5 cm was significantly associated with prolonged hospital stay (aRR: 1.63; 95% CI: 1.17 to 2.26). Patients who underwent bedside minor amputation (aRR: 1.79; 95% CI: 1.22 to 2.63) or surgical intervention (aRR: 2.04; 95% CI: 1.4 to 2.97) also had a higher risk of prolonged hospitalization compared to those managed with bedside debridement only.
In the bivariate analysis, patients classified as subgroup 3 in the "wound" category of the Wound, Ischemia, Foot infection (WIFI) classification (RR: 2.12; 95% CI: 1.06 to 4.24) and with a diagnosis of peripheral artery disease (RR: 1.51; 95% CI: 1.09 to 2.08) had an increased risk of prolonged hospital stay. However, these associations did not remain significant in the multivariate analysis.
Other variables, such as time to initial wound debridement, presence of osteomyelitis, and the “foot infection” category of the WIFI classification, were not independently associated with prolonged hospital stay in the adjusted models.
Both models (patient- and wound-related) showed excellent fit (patient-related model: deviance χ² (221) = 148.8, p = 0.999; wound-related model: χ² (140) = 76.96, p = 1.000). No extreme residuals were found, and leverage values were low (maximum ≈ 0.07). No influential observations were detected, supporting the stability of the risk ratio estimates.
The sensitivity analyses using alternative definitions of prolonged hospital stay yielded results consistent with the primary analysis regarding wound-related predictors. Wound length > 5 cm and the type of definitive treatment (minor amputation and surgical management) remained significantly associated with prolonged hospitalization when using the 16-day cutoff (p < 0.05). However, the association for wound length was weaker with the 21-day cutoff (p = 0.08) (Supplementary Tables S2 and S3).
On the other hand, none of the patient-related predictors were significantly associated with prolonged hospital stay under either definition (Supplementary Tables S4 and S5).
Discussion
Hospital length of stay is an indicator of healthcare efficiency and resource utilization [19] and directly contributes to healthcare costs [17]. Compared with patients hospitalized for other conditions, those hospitalized for diabetes-related foot infection can have up to twice the length of stay [20,21]. This study identified patient- and wound-related factors associated with prolonged length of stay among patients admitted to a tertiary-level diabetic foot care unit in Peru for diabetes-related foot infections. Nearly half of the patients exceeded the 10-day threshold established by the Peruvian Social Security system for inpatient care, highlighting the substantial impact of this infection on hospital resource utilization. Our findings show that documented atherosclerotic cardiovascular disease, wound length greater than 5 cm, and the type of definitive treatment were independently associated with prolonged hospitalization. The last two predictors remained associated with prolonged hospitalization in the sensitivity analyses using alternative definitions (≥16 days and ≥21 days).
Patient-related factors and prolonged hospital stay
In our cohort, nearly half of the patients had a prior history of atherosclerotic cardiovascular disease, which was independently associated with a 40% higher risk of prolonged hospital stay compared with those without this condition. Atherosclerotic cardiovascular disease is linked to impaired tissue perfusion and delayed wound healing [22,23] and may increase the complexity and duration of treatment. Similar results were reported by Kim et al. [15], and Loudon et al. demonstrated a comparable association in patients with acute coronary syndromes [24]. These findings highlight the potential impact of optimizing cardiovascular disease management during hospitalization to mitigate adverse outcomes, including prolonged hospital stay.
Although younger age (≤ 70 years) was initially associated with a longer hospital stay than older age (> 70 years), this association lost statistical significance after adjustment for treatment type. In a Spanish cohort, Nieto-Gil et al. similarly reported that older patients had shorter hospital stays [11]. These results may suggest different therapeutic strategies or treatment intensity between younger and older patients that could influence length of stay [18]. In contrast, other studies have found that advanced age is more strongly associated with amputation rather than prolonged hospitalization [25].
We did not find a significant association between prolonged hospital stay and sex, hypertension, chronic kidney disease, or osteomyelitis. These findings are consistent with other studies [26,27], though some studies, such as Tabur et al. [28], observed longer hospital stay among male patients (p = 0.04).
Wound-related factors and prolonged hospital stay
Wounds exceeding 5 cm were associated with a 63% higher risk of prolonged hospitalization compared to those <3 cm, and this association remained significant using the 16-day cutoff. These findings suggest that larger wounds demand more complex and extended hospital care. To our knowledge, no previous studies have specifically examined wound length in relation to hospital stay; however, greater wound depth [29] has been linked to prolonged hospitalization. Prospective studies are needed to validate wound length as a predictor of hospital outcomes in patients with diabetes-related foot infections.
In our cohort, higher scores in the “wound” and “foot infection” domains of the WIFI classification were associated with prolonged hospital stay in bivariate analysis, but lost significance in the multivariate model, possibly due to limited statistical power or residual confounding. Prior studies using the Wagner classification showed similar results, where higher grades have been consistently linked to longer hospital stay [28,30]; for example, Eren et al. reported an average length of stay of 15 days in patients with Wagner grade 3 or 4 lesions compared to 7.9 days in those with grade 2 (p = 0.009) [31]. These results support the plausibility that more severe wounds may require more complex management, underscoring the need for larger studies to validate wound classification systems for hospital outcomes, including length of stay.
Type of treatment and prolonged hospital stay
The type of definitive treatment of diabetes-related foot infection showed the strongest association with prolonged hospital stay. Patients undergoing bedside minor amputation had a 79% higher risk of prolonged hospital stay. In contrast, those requiring surgical debridement or major amputation had twice the risk compared with patients managed solely with bedside debridement. This association remained robust and statistically significant using both 16- and 21-day thresholds for defining prolonged hospital stay.
These findings are consistent with previous reports [21,28,30], including a study by Tan et al. in Singapore that reported a sixfold higher risk of prolonged hospitalization following major amputation. It is important to note that surgical interventions are typically reserved for severe cases and require perioperative work-ups, multidisciplinary decision-making, and longer recovery periods, which may increase the overall hospital stay [30]. In contrast, a recent report showed that limb-preserving strategies can lengthen hospital stay as a part of attempts to avoid major amputation [32].
In resource-limited settings such as our institution, where vascular interventions were rarely performed (3.5% angioplasty, no surgical revascularization), early and effective wound care is critical. Our analysis identified key predictors of prolonged hospitalization, such as large wounds, atherosclerotic cardiovascular disease, and minor amputation or surgical management, which should be addressed during the inpatient management of diabetes-related foot infections.
In addition, previous studies [12,33] suggest that implementing diabetic foot coordinators or skilled care facilities may help reduce length of stay and improve clinical outcomes; however, additional studies are required to confirm their effectiveness.
Limitations and strengths
This study was conducted in a single tertiary hospital, which may limit generalizability. Some important variables, such as glycemic control, microbiological data, and antibiotic resistance, were not analyzed due to limited access to data. Furthermore, peripheral artery disease was diagnosed by heterogeneous methods, potentially masking the effect of severe stages on healing time and amputation risk. Other outcomes, including remission, wound recurrence, and complications, were not assessed, highlighting the need for additional studies in the context of resource-limited settings.
Nonetheless, our study included a sizable patient cohort managed within a dedicated diabetic foot care unit, but with limitations that reflect real-world challenges such as limited access to revascularization. Sensitivity analyses using alternative definitions of prolonged hospitalization confirmed the robustness of wound-related predictors. Our findings may contribute to improving clinical decision-making by enabling early identification of predictors for prolonged hospital stay and guiding the design of future prospective studies in similar contexts.
Conclusions
In this Peruvian cohort of patients hospitalized for diabetes-related foot infection, nearly half experienced a prolonged hospital stay, based on local standards. Independent predictors of prolonged hospital stay included wound length greater than 5 cm, history of atherosclerotic cardiovascular disease, bedside minor amputation, and surgical management (major amputation or debridement).
Identifying clinical and wound-related predictors of prolonged hospital stay may support earlier intervention, reduce hospital burden, and improve outcomes for patients hospitalized with diabetes-related foot infection, particularly in resource-limited settings.

