Research papers
← vista completaPublished on April 27, 2017 | http://doi.org/10.5867/medwave.2017.03.6940
Risk factors for acute kidney injury in a pediatric intensive care unit: a retrospective cohort study
Factores de riesgo de lesión renal aguda en una unidad de cuidados intensivos pediátrica: cohorte retrospectiva
Abstract
BACKGROUND The incidence of acute kidney injury in the pediatric population and its associated risk factors are currently not clear.
OBJECTIVES The objective of the study was to assess the incidence of acute kidney injury in critically ill pediatric patients and to determine its associated risk factors.
METHODS We conducted a retrospective study of pediatric patients (<14 years old) admitted to a tertiary pediatric intensive care unit. Acute kidney injury (AKI) was classified using the Kidney Disease: Improving Global Outcomes definition KDIGO.
RESULTS A total number of 382 patients were assessed: acute kidney injury was found in 11.5% of them (incidence rate 0.99 persons-day). The following parameters analyzed with multivariate regression analysis were associated with acute kidney injury: low platelet count (R = 2.947; 95% CI= 1.276-6.805) and the need of vasopressor support (OR= 4.601; 95% CI= 1.665-12.710). Children with acute kidney injury had an increased length of stay in the hospital and an increased mortality compared with patients with no kidney injury (19 days vs. 5 days and 3.7/person-day vs. 0.32/person-day).
CONCLUSIONS Acute kidney injury is common among critically ill children and it is associated with adverse outcomes, including increased length of stay in the hospital and death. Low platelet count and vasopressor support were independently associated with the development of acute kidney injury in this population.
Introduction
Acute renal injury is an entity that may occur in hospitalized pediatric patients, especially in critically ill patients [1],[2],[3],[4],[5], a complication associated with longer hospital stay and increased risk of mortality [1],[3],[6],[7],[8]. The incidence and prevalence of acute renal injury in children is not known with certainty due to the lack of standardized definitions across different age groups [9]. In a study in neonates, the incidence of acute kidney injury ranged from 8% to 24%, according to the definition used and the severity of the disease [10]. Likewise, studies reported on this entity in Latin America are scarce [11]. This scenario seems similar in Colombia, where we only found a series of cases in Cali reporting a frequency of acute kidney injury of 0.38% and of 6.2% in patients hospitalized in general or intensive pediatric care units respectively [12].
Among the classifications proposed for acute kidney injury, the most commonly used and standardized for pediatric patients are pediatric Risk, Injury, Failure, Loss, End Stage Renal Disease (pRIFLE) [13], Acute Kidney Injury Network (AKI) [14] and Kidney Disease Improving Global Outcomes (KDIGO) [15]. In general, the parameters used for the definition are increased serum creatinine and decreased urinary output [16].
Early identification of risk factors for acute renal injury would allow establishing preventive strategies to decrease morbidity and mortality in these patients [17]. At present, risk factors associated with acute renal injury in children in pediatric intensive care units vary according to certain health and demographic characteristics. Age, anthropometry, blood pressure, basal glycaemia, lactate values, duration of mechanical ventilation, vasoactive therapy and the presence of infection, hypoxia and multiple organ dysfunction or coagulopathy are among the most mentioned [4]. Due to this variation in the risk factors for acute renal injury and the lack of local and regional data regarding their incidence and prevalence, it is necessary to evaluate them in order to detect patients that could benefit from an early treatment or a preventive intervention [18].
The primary objective of this study was to determine the incidence of acute renal injury in a critically ill pediatric population with no previous history of renal disease, who were treated at the Hospital Pablo Tobón Uribe, Medellin, Colombia during 2010-2014, and to identify risk factors for its occurrence.
Methods
Retrospective cohort where the medical records of patients younger than 14 years admitted to the pediatric intensive care unit or pediatric intermediate care unit (UCEP) were reviewed.
Location, performance period, and participants:
Hospital Pablo Tobón Uribe, is an institution with 85 pediatric beds and 18 intermediate and intensive pediatric care beds. It has an average of 600 admissions to intermediate and intensive pediatric services per year. Data collection was performed from January 2010 to December 2014. Patients aged 1-14 years who were transferred to intermediate and intensive pediatric care services due to deterioration of their clinical condition were considered eligible. Patients admitted for renal transplantation, with a diagnosis of cerebral death upon admission to intermediate and intensive pediatric care services, length of stay under 24 hours, previous diagnosis of acute renal injury at entering intermediate and intensive pediatric care services, and patients for whom no creatinine data were found during their stay in intermediate and intensive pediatric care services were excluded. Patients with a history of chronic kidney disease or malformations of the urinary tract were also excluded. The latter with the objective of evaluating risk factors other than previous renal injury for the presence of acute renal injury in a critically ill pediatric population.
Evaluated variables:
The main outcome was the appearance of acute renal injury during the stay period in the intermediate and intensive pediatric care services. Acute renal injury was defined, according to the Kidney Disease Improving Global Outcomes classification, as an elevation of serum creatinine values of 0.3 mg/dl with respect to baseline values [15],[19]; glomerular filtration rate was calculated using the Schwartz formula.
The following were considered as potential risk factors for the occurrence of acute renal injury: a diagnosis at the time of admission to intermediate and intensive pediatric care services of: respiratory failure, hypovolemic or hemorrhagic shock, cardiovascular disease, infections, postoperative trauma, non-renal transplant, presence of severe hypoxemia defined as PaO2/FiO2 (partial pressure of arterial oxygen/fraction of inspired oxygen) less than 200, presence of coagulopathy defined as International Normalized Ratio (INR) greater than 1.5, partial thromboplastin time (PTT) prolonged more than twice, thrombocytopenia defined as a count below 150,000 x mm3 and use of nephrotoxic agents (acyclovir, foscarnet, aminoglycosides, colistin, vancomycin, calcineurin inhibitors, nonsteroidal anti-inflammatory drugs). In addition, data on mortality over time in pediatric intensive and intermediate care services, need for renal replacement therapy and glomerular filtration rate at the end of follow-up were collected
Finally, acute renal injury was classified according to the Kidney Disease Improving Global Outcomes guidelines as: stage 1 when creatinine values increased above 0.3 mg/dl from baseline or an 1.5-to-1.9-fold elevation; stage 2 when the increase was 2 to 2.9 times; and stage 3 when it was ≥ 3 times, a creatinine with acute elevation above 4 mg/dl, or the need for renal replacement therapy [15],[20].
The database provided by the Hospital Pablo Tobón Uribe information management system between 2010 and 2014 was used for data collection. Afterwards, all the medical records of patients who met inclusion criteria were meticulously reviewed. Data were extracted from the institution's electronic medical records and were recorded in an Excel database for later statistical analysis with the SPSS and STATA programs.
Statistical analysis:
Statistical analyses were performed in five steps.
First: the incidence rate of acute renal injury was determined in the intermediate and intensive pediatric care services, for which it was calculated the number of patients with a diagnosis of acute renal injury out of the total patient days of stay in the intermediate and intensive pediatric care services from January 2010 to December 2014.
Second: descriptive statistics were performed; quantitative variables were presented with means and standard deviation, or medians and interquartile ranges, according to their distribution, which was checked by means of the Shapiro-Wilk test. Categorical variables were analyzed through proportions. Third: we searched for risk factors associated with acute renal injury in the critically ill pediatric population by means of a logistic regression model, with the presence or absence of acute renal injury as the dichotomous response variable. The independent variables were risk factors reported as such in the literature and variables that in the bivariate analysis showed a p value lower than 0.25. Wald statistic was used for assessing statistical significance of the regression coefficients.
Fourth: in an exploratory way, we evaluated the association of mortality in the clinically ill pediatric population, to the presence or absence of acute renal injury; for this, we compared the proportion of patients who died during the time of hospitalization in intensive and intermediate pediatric care services among those with acute renal injury with the proportion died among those without acute renal injury. Fifth: finally, the relationship between acute renal injury and the increase in the average length of hospital stay in intensive and intermediate pediatric care services, was evaluated.
Lost data were handled by multiple imputation; this process replaces lost data with plausible values, based on the observed data, thus allowing the statistical analysis with the complete data conserving the initial sample size. The variables used to perform multiple imputation were: oxygen arterial pressure/oxygen inspired fraction (PaO2/FiO2), partial thromboplastin time (PTT), potassium, lactate, platelets, use of vasopressors and use of nephrotoxic agents. Five imputations were calculated for each analyzed variable. The imputation method used was the fully conditional specification, and the maximum number of selected iterations was 1000. To verify the presence of potential important changes caused bay imputations we compared the obtained results before to those obtained after multiple imputation. To perform this procedure, we used statistical package SPSS version 20.
Ethical considerations:
This study was approved by the ethics and research committee of the Hospital Pablo Tobón Uribe, and it followed the norms on ethical aspects of the investigation in human beings contained in Resolution 008430 of 1993 of the Ministry of Health of Colombia. In addition, the confidentiality of the personal data of the patients included in the study was preserved.
Results
During the study period, 725 patients aged 1-14 years were admitted to the intensive and intermediate pediatric care services of Hospital Pablo Tobón Uribe. Of these, 343 patients were excluded because they had no renal function data, length of stay in intensive and intermediate pediatric care services less than 24 hours, a history of acute renal injury or urinary tract malformations, renal transplantation or diagnosis of brain death (Figure 1). Of the 382 evaluated patients, 11.5% (n = 44) presented acute renal injury after admission to intermediate and intensive pediatric care services, with an incidence rate of 0.99/person-days. When grouped according to the Kidney Disease Improving Global Outcomes (KDIGO) classification, 38.6% (n = 17) initially behaved as KDIGO-1; 29.6% (n = 13) as KDIGO-2; and 31.8% (n = 14) as KDIGO-3.
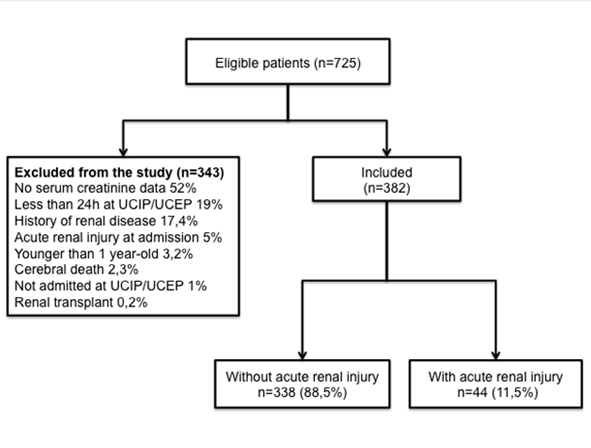 Full size
Full size The mean age was 6.1 years (SD=4.29); and 52.9% (n = 202) were males. Mean serum creatinine value prior to admission to the pediatric intensive care unit was 0.5 mg/dl (SD=0.134). The main causes of admission to intermediate and intensive pediatric care services were: infections, 31.2% (n = 119); postoperative, 21.2% (n = 81); and other, 23.6% (n = 95) (Table 1). No association was observed between age or gender of the patients, and presence of acute renal injury. On the contrary, the values of PaO2/FiO2 at admission, partial thromboplastin time, total bilirubin and serum potassium values at the time of diagnosis were different between both groups; as well as the need for mechanical ventilation, the use of vasopressors, nephrotoxic agents, and the use of vancomycin prior to the presence of acute renal injury (Table 1)
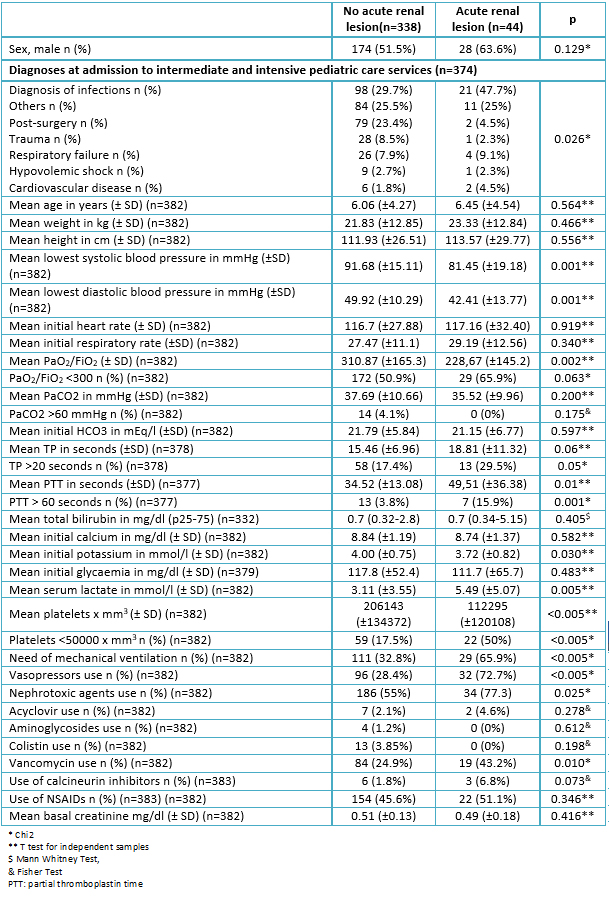 Full size
Full size Multivariate analysis:
Platelet values less than 50,000 x mm3 (OR = 2.947, 95% CI = 1.276 - 6.805) and vasopressors use (OR = 4.601, 95% CI = 1.665-12.710) were identified as risk factors for acute renal injury through multivariate logistic regression analysis (Table 2).
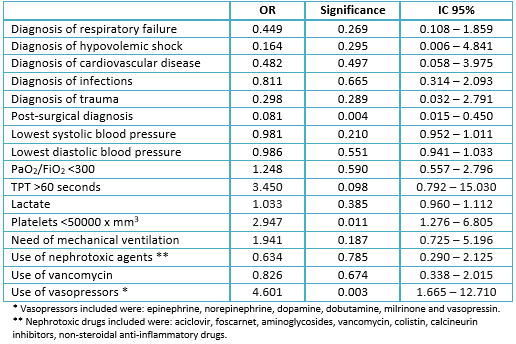 Full size
Full size Table 3 shows the univariate and multivariate analysis of the variables in which multiple imputation was performed; and the percentage of values imputed for each variable. As it can be observed, with the exception of the variable: PTT> 60 seconds, no significant differences were observed when comparing the previous and posterior results to multiple imputation.
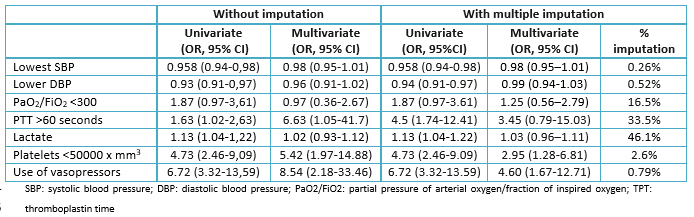 Full size
Full size Secondary outcomes:
Patients with acute kidney injury required longer hospitalization periods compared to those without acute renal injury (19 days vs. 5 days, p = 0.000). Mortality rate in patients with acute renal injury was also significantly higher (3.7/person-day vs. 0.32/person-day) (Table 4); hospital stay was higher in patients with acute renal injury KDIGO-2, and mortality was higher in patients with acute renal injury KDIGO-3 (50%) (Table 5).
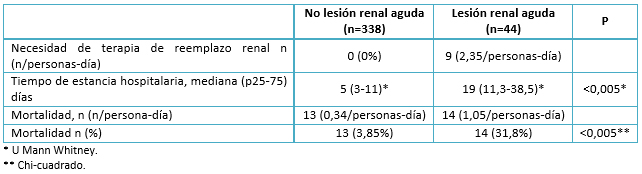 Full size
Full size 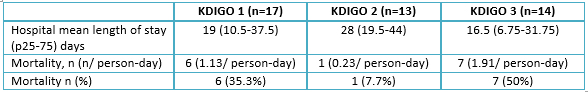 Full size
Full size Evolution of glomerular filtration rate:
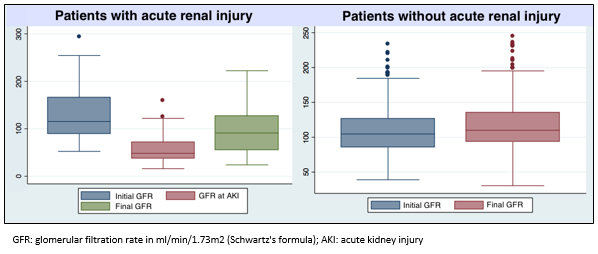
Glomerular filtration rate in patients with acute renal injury at discharge was lower than their baseline values; the initial glomerular filtration rate in these patients was 127.9 ml/min/1.73m2 (± 54.12); and at discharge, its mean decreased to 97.89 ml/min/1.73m2 (± 52.48) (p = 0.0003). In patients without acute renal injury, the initial glomerular filtration rate was 110.98 ml/min/1.73m2 (± 40.85); and at the time of discharge, it was 119.54 ml/min/1.73m2 (± 39. 80) (p = 0.0002) (Figure 2). In the group with acute renal injury, 45% of the patients had a final glomerular filtration rate value lower than 90ml/min/1.73m2; and in patients without acute renal injury, 19% had a glomerular filtration rate lower than 90ml/min/1.73m2.
 Full size
Full size Discussion
This study, which was conducted in a cohort of pediatric patients hospitalized in intermediate and intensive pediatric care services, aimed to assess the incidence of acute kidney injury and its associated risk factors. The incidence of acute renal injury was 11.5%, with a mortality observed in patients with acute renal injury of 31.8% vs 3.85% in those who did not present acute renal injury. Additionally, hospital length of stay was higher in patients with acute renal injury (19 days vs. 5 days), findings that support the importance of establishing preventive measures to avoid this complication, including the identification of risk factors associated with acute renal injury. In the evaluated cohort, a platelet value of less than 50,000 u/ml3 and the use of vasopressors were independent risk factors for acute renal injury.
Previous studies have reported incidences of acute renal injury greater than that found in our study. Cabral and colleagues reported an incidence of acute renal injury of 55% [3]; Safdar and colleagues reported 51.6% [8]; and Sutherland and colleagues 40.3% [21]. However, these studies included patients with a previous history of renal disease, and the severity profile of the pathologies and comorbidities was worse. In our cohort, we excluded patients with a history of hydronephrosis, renal transplantation, chronic kidney disease, vesicoureteral reflux and urinary infections prior to admission to intermediate and intensive pediatric care services, a fact which may explain the lower incidence of acute renal injury (11.5%). With regard to diagnosis, infectious diseases were significantly more frequent in the population with acute renal injury, similar to the findings of Duzova and colleagues who observed that ischemic injury (28%) and sepsis (18.2%) were the major causes of acute renal injury in 472 patients with acute kidney injury [22]. Esezobor and colleagues described sepsis as a cause of acute renal injury in 41.6% of 91 pediatric patients [23], a finding similar to that reported in the literature, where the main causes of acute kidney injury in developing countries are hemolytic uremic syndrome and systemic infections [24],[25].
There are many studies focusing on the risk factors for acute renal injury in the adult population, but few studies assess the pediatric population. Considering that the incidence of acute renal injury in critically ill patients is high, it is important the early identification of patients at risk for acute renal injury, in order to optimize resuscitation and support therapies, as well as to reduce preventable risks, such as the use of nephrotoxic drugs and contrast media for imaging studies [26]. In our cohort, after multivariate analysis, only platelet values below 50,000/mm3 and vasopressors use were independent risk factors for acute renal injury, a finding that has not been frequently reported in previous studies. Zhou and colleagues found out in a study of 205 pediatric patients with acute kidney injury that high values of urea nitrogen and low platelet values were independent risk factors for non-recovery of renal function [2].
Pol and colleagues conducted a multicenter prospective study in children younger than 16 years, hospitalized in intermediate and intensive pediatric care settings; in the logistic regression analysis, low platelet values were the major risk factor for the need for dialysis; for each 1000 platelets/mm3 lower, the risk of dialysis increased by 1.141 [18]. Baileys and colleagues in a study of 1,047 pediatric patients admitted to the pediatric intensive care unit found, in the multivariate analysis, that thrombocytopenia was a significant risk factor for acute renal injury (OR 6.4 95% CI 2.5-16, 2) [27]. One of the possible explanations for our findings is that platelet values and vasopressor use may be a marker of baseline disease severity, rather than a risk factor for acute renal injury [27]. In the evaluated cohort, patients with acute renal injury and need for vasopressors required mechanical ventilation more frequently, compared to patients who did not present acute renal injury nor vasopressors use (84.4% vs 65.5%, respectively). On the other hand, the group with acute renal injury and use of vasopressors, the most frequent diagnoses, reported at the time of admission to the critical care unit, were infections in 50% of cases, and respiratory failure in 12%. These findings suggest to take into account these two variables in the follow-up performed to critically ill pediatric patients. In patients with greater clinical deterioration, need for mechanical ventilation or with diagnosis of infections, it is suggested to frequently monitor renal function.
Surprisingly, the use of nephrotoxic agents in the multivariate analysis was not a risk factor for the presence of acute renal injury, although it was in the univariate analysis. However, this may be explained by previous knowledge of the following drugs as potential risk factors for acute renal injury: acyclovir, foscarnet, aminoglycosides, vancomycin, colistin, calcineurin inhibitors and nonsteroidal anti-inflammatory drugs. This is a reason to deliver these drugs only when necessary and with adequate dose control formulated to prevent the development of acute renal injury.
Another finding in our cohort was the higher in-hospital mortality in patients with acute renal injury, even in those with AKI-1 acute renal injury. This is consistent with the results reported by Touza Pol and colleagues who observed a 32.4% mortality rate in 136 children that entered the pediatric intensive care unit, and 15.1% of the survivors needed dialysis on discharge from the pediatric intensive care unit [18]. Sutherland and colleagues carried out an observational study in 1,479 patients under the age of 18 who were hospitalized, in which the mortality was higher in stages 1 and 3 of acute renal injury [21]. Other studies have reported a mortality ranging from 11% to 58.9% [2],[17]. However, it should be borne in mind that we evaluated only in-hospital mortality, which may partly explain the low percentage of patients with this outcome.
When assessing renal function at discharge, 45% of patients with acute kidney injury had a GFR of less than 90 mL/min/173m2 vs 19% in patients without acute renal injury, a finding similar to that reported by the Study of Askenazi and colleagues [28] and Hui-Stickle and colleagues [29], in which 34% to 50% of children who presented acute kidney damage evolved to chronic renal failure during follow-up. Ball and Kara [30] found that 40% of children who required dialysis for acute kidney damage had renal abnormalities at the time of hospital discharge. This finding consolidates the recommendation of long-term follow-up for children with acute kidney damage.
Goldstein has recently developed the empirical concept of renal angina, a scale that evaluates some risk factors for acute renal injury, which would allow its anticipation along with a strict monitoring of renal function for early clinical diagnosis and prevention [31]. This scale seems to have a higher predictive value than the Kidney Disease Improving Global Outcomes classification, especially in stage 1 of acute renal injury, but it is still not used for the diagnosis of acute renal injury, and it has not yet been validated in our population.
Among the limitations of our study is the fact that it was performed in a single hospital in the city, which does not allow the generalization of its results. In addition, it was a retrospective study, which limits the quality of the data and may explain the high percentage of missing data. Moreover, the definition of acute renal injury did not include any measurement of urinary output, which is a fundamental part in its definition and classification. Finally, the low number of children with the outcome of acute renal injury did not allow the analysis of all possible risk factors, and may decrease the statistical power of the results.
Conclusions
In summary, our results suggest that an important percentage of pediatric patients entering the intermediate and intensive pediatric care services present acute renal injury, especially those with a diagnosis of severe systemic infection. This fact increases hospital stay and mortality, even in the early stages of acute renal injury [6].
These findings support the importance of a strict monitoring of renal function, even in patients with no previous history of renal disease but with known risk factors for acute renal injury. In our cohort, platelet values below 50,000/ml and the use of vasopressors were risk markers for acute renal injury.
Notes
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Ethical aspects
The Journal is aware that the ethical scientific committee of the Pablo Tobón Uribe Hospital, Medellín, Colombia, was aware of this study and its possible publication in a biomedical dissemination journal.
Declaration of conflicts of interest
The authors have completed the ICMJE Declaration of Conflicts of Interest form and state that they have received funding from the Pablo Tobón Uribe Hospital for the report; not having financial relationships with any other organization that might have interests in the published article in the past three years; and not having other relationships or activities that could influence the published article. Forms can be requested by contacting the responsible author or the editorial board of the Journal.
Financing
The authors state that this manuscript received financial support from the Pablo Tobón Uribe Hospital in the city of Medellín, Colombia

