Estudios originales
← vista completaPublicado el 18 de diciembre de 2020 | http://doi.org/10.5867/medwave.2020.11.8088
Mortalidad de los pacientes intervenidos de artroplastia de rodilla y cadera en Chile: análisis de sobrevida
Mortality after hip or knee arthroplasty for osteoarthritis in Chile: A survival analysis
Abstract
Background The purpose of this study is to determine if patients with osteoarthritis that undergo hip or knee arthroplasty jeopardize their life expectancy in Chile.
Methods A survival analysis study was designed and approved by our institutional ethics review board. Patients were included if they underwent surgery for hip or knee osteoarthritis and were 50 years or older at the time of surgery. Patients were excluded if arthroplasty was performed for fracture, hemophilia arthropathy, or tumor. A multiparametric Weibull regression was estimated, and the hazard ratio was reported. For internal validity, a bootstrap of 200 repetitions was performed.
Results A total of 4 094 arthroplasties were included. The Kaplan-Meier curve estimates a higher survival than the general population up to 12 years, after which the median survival is less than the general population. The bootstrap multiparametric Weibull regression estimated a hazard ratio of 1.53 (95% confidence interval: 1.27 to 1.84) for women, 1.09 (1.08 to 1.10) for every year older, and 1.29 (1.07 to 1.53) for hip arthroplasty patients.
Conclusion Mortality after hip and knee arthroplasty in Chile follows a bimodal behavior similar to reports from the United States and Europe. At first, mortality is lower than the general population but worsens after 12 to 15 years of surgery.
Main messages
|
Introduction
Osteoarthrosis is a frequent disease that causes pain, disability, and diminished quality of life. The most common compromised joint is the knee, followed by the hand and the hip[1]. Hip arthroplasty has been touted as the main surgery of the XXth century due to the impact it has had on patients' functionality and quality of life[2]. Knee arthroplasty indication has been increasing throughout this century, establishing it as a cost-effective treatment for knee osteoarthritis[3].
Implant survival has been widely studied. A recent systematic review has shown that the 25-year survival rate of hip prosthesis is 58%[4], and for knee prosthesis, the 20-year survival rate is above 80%[5]. Nevertheless, fewer studies have addressed the impact on patient’s survival compared to the general population; moreover, the results do not readily extrapolate to Chile or Latin-American reality due to many factors, among the most important might be the diversity of socioeconomic status[6]. A study carried out in the United States reported that survival after hip or knee arthroplasty had a bimodal behavior: initially greater survival than the general population and after 15 years, higher mortality than the general population[7]. A previous study performed in Sweden reported the same bimodal pattern, but the shift was at 12 years[8]. Similarly, a study performed in Denmark reported higher survival than the general population at a maximum follow-up of 12 years[9].
Patients before surgery commonly ask about mortality related to the procedure and their life expectancy after arthroplasty. The purpose of this study is to determine if patients with osteoarthritis that undergo hip or knee replacement jeopardize their life expectancy in Chile.
Methods
A survival analysis study was designed and approved by our institutional ethics review board. The patients were recruited from two general hospitals in Santiago, Chile: Hospital San Jose and Hospital Clínico Universidad de Chile. Both centers have access to the same type and brands of prostheses, and surgeons have a similar level of training; moreover, two of them work in both centers. The first hospital belongs to the public network of health centers, so all patients treated were affiliated to the public insurance, known as the National Health Fund. A public university owns the other center, and about half of the patients that received medical treatment were affiliated to the National Health Fund.
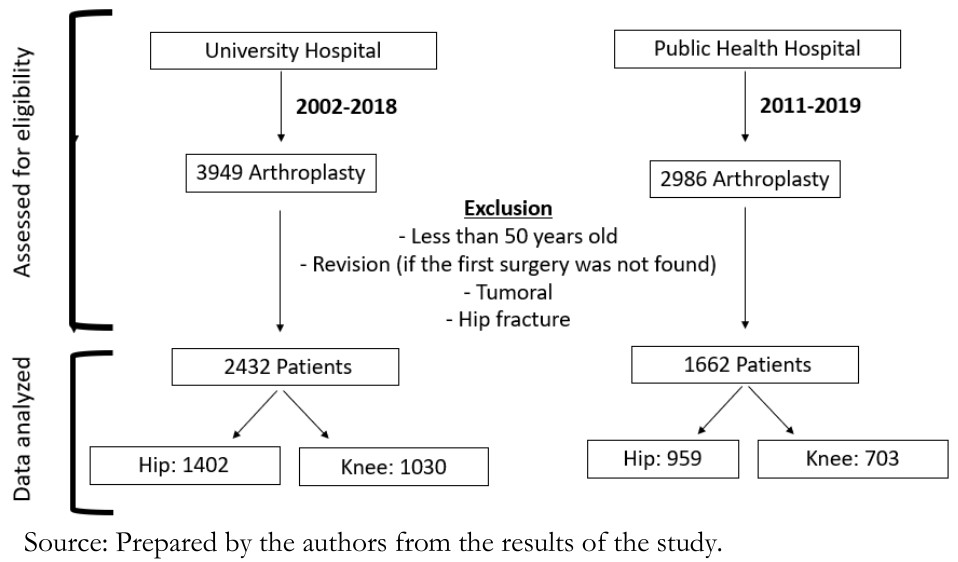
A search was conducted in both institutions using the National Health Fund code that identifies each procedure (2104129-11 for hip arthroplasty and 2104153-10 for knee arthroplasty). Patients were included if they underwent surgery for severe hip or knee osteoarthritis and were 50 years or older by the time of surgery. Patients were excluded if arthroplasty was performed for fracture, hemophilic arthropathy, or tumor. Also, revision arthroplasties were excluded. The review was done in the university hospital between January 1, 2002, to December 31, 2019, while the public hospital review was done from June 1, 2011, to February 29, 2020. Unfortunately, data before 2012 were not available. The flow chart of patient selection is shown in Figure 1. The patient’s full name, national ID number, gender, birth date, date of admission, date of discharge, surgery code, and surgery date were recorded. Patients with incomplete information were excluded. Then, by the National Transparency Act, we requested the National Civil Registry of Chile to inform whether the patients were alive by March 30, 2020; if deceased, they were asked to report the date of death.
 Full size
Full size Continuous variables were summarized in median, range, and interquartile range (IQR, p25–p75). Absolute frequency and percent were used to describe discrete variables. The unmatched nonparametric median test was used to compare continuous variables, and Fisher’s exact test was used to compare discrete variables. A p-value of < 0.05 was interpreted as significant.
For survival analyses, the initial time (t0) was the date of surgery. The final follow-up was March 30, 2020, and failure was defined as death by any cause. Total time at risk, the annual incidence of death and the percentile of survival time were reported for hip arthroplasty and knee arthroplasty. A multiparametric regression was estimated, Weibull exponential and log-normal distribution were tested. The distribution that had the best fit model was determined using log-likelihood, the relation between Cox-Snell residual and Nelson Aalen cumulative hazard, and the linear relation between the natural logarithm of the survival probability and the analyzed time. The hazard ratio is reported. For internal validity, a bootstrap of 200 repetitions was performed. The covariables were tested using the Wald test, and the power of each hazard ratio was calculated
The 2016 publication of the Statistics National Institute of Chile (INE)[10] was used to compare this estimation to the expectancy of life of the general Chilean population, reported in groups of five years. The age of the cohort included in the study was grouped forming four groups: 50 to 59, 60 to 69, 70 to 79, and 80 years or older. Each group was compared to the adjusted expectancy of life by age and gender for the general population, assuming an exponential distribution.
A significance of 5% was used, and a 95% confidence interval were estimated. The data were processed using Stata version 15 (StataCorp LP, College Station, Texas, USA).
Results
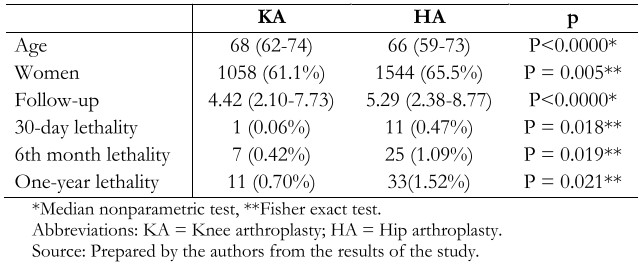
A total of 4 094 arthroplasties were included, of which 1 733 were knee arthroplasty replacements (42.3%), and 2 361 were hip replacements (57.7%). The median age was 67 years old (range, 50 to 97; interquartile range, 60 to 74), and 2 602 (63.6%) were female patients. Patients that underwent knee arthroplasty were significantly older than hip arthroplasty patients. Also, a significantly higher proportion of women was found in the hip arthroplasty group. During the period studied, a total of 462 patients died after arthroplasty (11.3%) (Table 1).
 Full size
Full size The median follow-up was 4.98 years (interquartile range, 2.25 to 8.43). Follow-up was significantly longer in the hip arthroplasty patients (Table 1). The lethality at 30 days, six months, and one year were higher in the hip arthroplasty group, reaching a statistical difference.
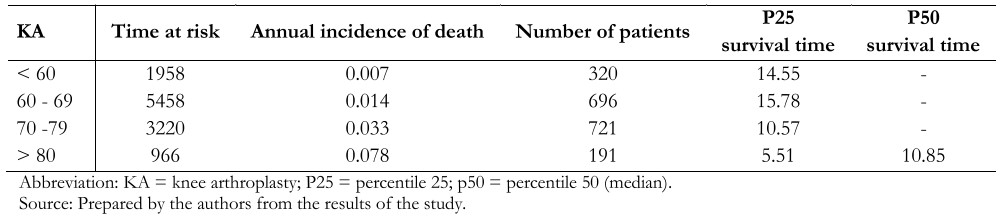
The total time at risk was 24 035 years, with an incidence rate of death by year of 0.019. The 25 percentile of survival time was 12.75 years. In the hip arthroplasty patients, the incidence of death by year was 0.021, and in the knee arthroplasty was 0.179. The 25 percentile of survival time was 12.90 years in hip arthroplasty patients and 11.89 years in knee arthroplasty patients. The total time at risk, the incidence of death and the median survival time percentile are summarized in Tables 2 and 3. The Kaplan-Meir survival curve was estimated knee arthroplasty and hip arthroplasty compared to the adjusted general population survival showing bimodal mortality. The Kaplan-Meier curve estimates a higher survival than the general population at up to 12 years, after which the median survival is less than that of the general population (Figure 2).
 Full size
Full size 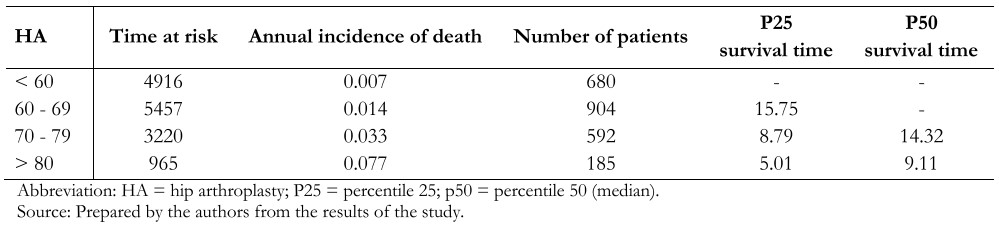 Full size
Full size 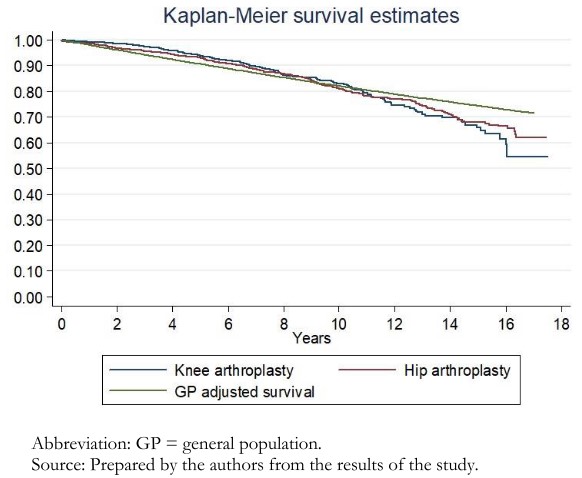 Full size
Full size The Weibull distribution was the best fit. The bootstrap multiparametric Weibull regression estimated a hazard ratio of 1.53 (95% confidence interval: 1.27 to 1.84) for women, a hazard ratio of 1.09 (95% confidence interval: 1.08 to 1.10) for every year older, a hazard ratio of 1.29 (95% confidence interval: 1.07 to 1.53) for hip arthroplasty. The parameter of the Weibull regression was 1.38 (95% confidence interval: 1.24 to 1.53), meaning a significant increase of risk of death by year after arthroplasty to a rate of 32% annually (95% confidence interval: 0.22 to 0.43), Wald test was significant p = 0.000, and the power for each hazard ratio was 0.99. The institution where the surgery was performed was not significant in long-term survival (hazard ratio 0.96; 95% confidence interval: 0.81 to 1.15).
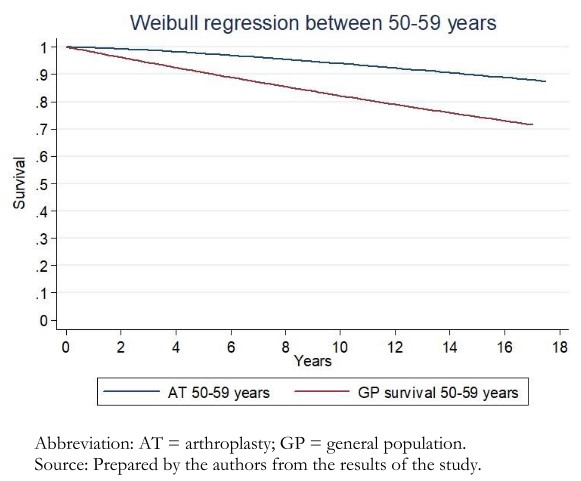
The Weibull estimation shows that knee arthroplasty and hip arthroplasty patients between 50 and 69 live at least 17 years longer than the general population (Figures 3 and 4). Meanwhile, patients over 70 years had a lower life expectancy 15 years after surgery (Figure 5). Also, patients above 80 years old had higher life expectancy than the general population until four years after surgery (Figure 6).
 Full size
Full size 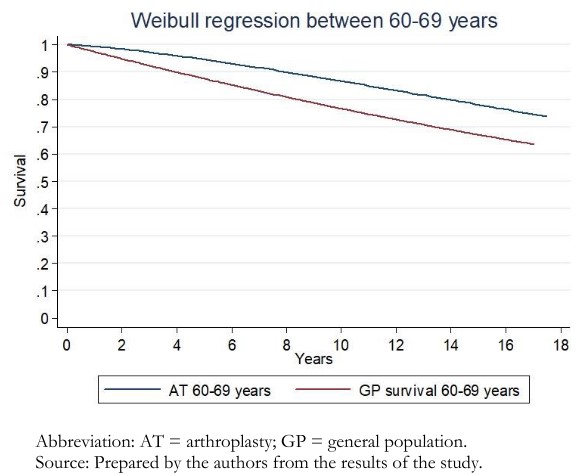 Full size
Full size 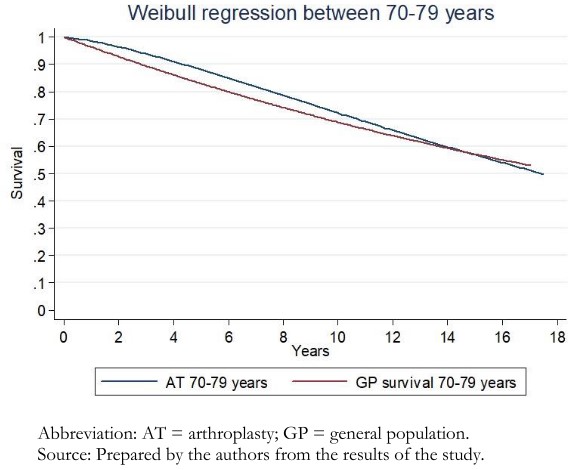 Full size
Full size 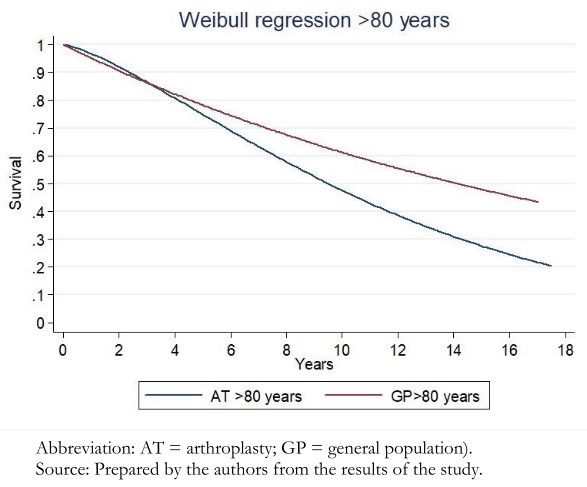 Full size
Full size Discussion
This study’s main finding shows that patients under 80 years old who undergo hip arthroplasty or knee arthroplasty do not compromise their life expectancy for the first 15 years after surgery, at least, which is consistent with the previous studies that report lower mortality than the general population during the first 12 to 15 years after surgery[7],[8],[9]. However, after this period of more prolonged survival, mortality was higher than the general population. This bimodal pattern was more abrupt in the population over 70 years. This bimodal pattern is similar to that reported in studies in the United States and Sweden, where the shift occurred between 12 and 15 years[7],[8].
The causes of this bimodal pattern are yet to be determined. The initial lower mortality is associated with patient selection, where patients that undergo arthroplasty must ascertain health status, and cardiovascular disease must be ruled out[7]. Moreover, patients that underwent successful arthroplasty achieved pain relief, which has been related to a higher life expectancy[11]. On the other hand, the increased mortality may be due to the increased risk of cardiovascular disease in patients with osteoarthritis compared to the general population. Patients with osteoarthritis have a 24% increased risk of developing cardiovascular disease, a relative risk of 2.80 (95% confidence interval: 2.25 to 3.49) to have heart failure, and a relative risk of 1.78 (95% confidence interval: 1.18 to 2.69) to have ischemic heart disease[12],[13]. This is supported by Swedish registry findings, where the leading cause of death in patients with osteoarthritis was cardiovascular disease[8]. Patients who have required a hip or knee prosthesis should be encouraged to follow routine controls for cardiovascular disease.
No difference in lethality after arthroplasty between the university and the public hospital was found in this study. Both centers were compared for lethality after hip fracture, and a higher lethality was found in the public center[14]. Therefore, socioeconomics and type of health insurance (public or private) play a minimum role in the bimodal behavior found in these patients, unlike hip fracture patients.
The time gap is shorter between the initial increase in survival and the later increase in mortality. Cardiovascular diseases are more prevalent as age increases, explaining the shorter gap of higher survival rates than the general population[15].
A significant hazard ratio in favor of knee replacement was found in this study. A patient undergoing hip replacement due to secondary osteoarthritis [hip dysplasia, inflammatory arthritis, and femoral head necrosis] does not achieve less mortality than the general population at any time[16]. Also, a significant proportion of knee procedures included in this study were done after 2012, so compared to an increased proportion of patients that underwent hip replacement before 2012, the comparison is uneven. An explosive increase in knee replacement procedures has been described in the last decades, and our cohort was not an exception[17],[18],[19]. Maradit-Kremers et al. demonstrate that comparing mortality rates between decades in patients that underwent arthroplasty is significantly different[7]. This could be explained by patients who underwent arthroplasty for femoral head necrosis or hip dysplasia, which were not an exclusion criterion in this study.
The findings in the over 80 years old cohort should encourage an interdisciplinary approach to diminish mortality after arthroplasty. Orthogeriatric should move forward from hip fracture to arthroplasty care[20]. Programs with good results have been reported in patients over 89 years old, reaching a better higher survival rate than the general population at four years follow up[21]. For knee osteoarthritis, unicompartmental arthroplasty is less invasive than total knee with similar functional and survival outcomes in patients over 75 years old[22],[23]. It could be that this less aggressive procedure tends to lower mortality rates in elderly patients.
This study has some limitations. The sample size is smaller and has a shorter follow up than the reports from the United States and Europe; nevertheless, the mortality trend is comparable. Also, the estimated regression model with good internal validity and high-power estimation of each hazard ratio minimizes the possible bias arising from the sample size.
Another limitation of this study is that the specific cause of mortality is unknown, so for example, a patient could have a hip arthroplasty performed but died because of lung cancer. Nevertheless, the number of patients studied minimizes this bias.
In addition, this study has a limitation in that the overall data were extracted from two hospitals and might differ in other regions of Chile or countries in Latin America. Nevertheless, the results obtained compared similarly to international reports, and there was no difference between public and private health institutions, making the results more generalizable.
Conclusion
Mortality after hip and knee arthroplasty in Chile follows a similar bimodal behavior over the years to reports from the United States and Europe. First, lower mortality than the general population is expected, but patients have increased mortality approximately after 12 to 15 years. The time gap is shorter in patients over 80 years, so this patient age-group must be carefully selected and adequately followed to optimize the results of this surgery; an interdisciplinary approach is mandatory. The risk of death after arthroplasty surgery is not constant and increases 0.32 by year. The survival rate after arthroplasty in this cohort of Chilean patients is similar to international reports.
Notes
Acknowledgments
The first author acknowledges the unconditional support of Leonel Barahona.
Roles and contributions of authorship
MB: Conceptualization, methodology, formal analysis, Investigation, data curation, writing (original draft preparation) and project administration. CB: Methodology, investigation, writing (review and editing), supervision and visualization. AM: Investigation, resources, writing (review and editing). JB: Investigation, resources, data curation, writing (original draft preparation). JPP: Data curation, investigation and writing (original draft preparation). JH: Validation, resources, investigation and writing (review and editing).
Conflict of interest
The authors declare that they have no competing interests.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was approved by the Hospital Clínico Universidad de Chile ethics research board, as stated in certificate number 32, issued on July 1, 2020.
Availability of data
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Language of original submission
Submitted and peer-reviewed in English.

