Estudios originales
← vista completaPublicado el 28 de diciembre de 2021 | http://doi.org/10.5867/medwave.2021.11.002068
Predictores de recurrencia de enfermedad tromboembólica venosa post suspensión de anticoagulación: estudio de cohorte prospectiva
Predictors of recurrence of venous thromboembolic disease after discontinuing of anticoagulation: a prospective cohort study
Abstract
Objective We aim to evaluate factors associated with the recurrence of thromboembolic episodes among patients with a first episode of venous thromboembolic disease during anticoagulation treatment and at least one year after treatment suspension.
Methods A prospective cohort of patients with a first episode of deep vein thrombosis confirmed by Doppler ultrasound and initiated anticoagulation treatment. Participants were registered in the Institutional Registry of Thromboembolic Disease between June 2015 and March 2019. Patients with cancer, with permanent inferior vena cava filter implant, and those who refused to participate or did not provide informed consent were excluded. All patients were evaluated within treatment at 30 days and at least one year after the suspension of anticoagulation with a D-dimer study and an ultrasound. All patients were evaluated for recurrence, bleeding (major and minor), and death.
Results A total of 304 patients were recruited during the study period. Seventy-three percent were female, and the median age was 80 years. The rate of recurrence rate during anticoagulation treatment was 5% (N = 16/303; 95% confidence interval: 3 to 8), and 5% during post-suspension follow-up (N = 11/202; 95%CI: 3 to 9). The overall bleeding rate was 13% (N = 39; 95%CI: 9 to 17), and 5% for major bleeding. Patients who recurred had higher basal D-dimer mean, higher neutrophils and monocytes, and a higher prevalence of age-adjusted D-dimer ratio greater than 0.5 before discontinuation. In addition, they more frequently had complete leg involvement by ultrasound and received a shorter treatment.
Conclusions Although some baseline and pre-suspension parameters had a higher recurrence incidence, statistical significance was not reached, probably due to small statistical power and a short-term follow-up.
|
Main messages
|
Introduction
Venous thromboembolic disease is the most frequent cause of preventable mortality in hospitalized patients [1]. Pulmonary embolism and deep vein thrombosis are the two most common manifestations of venous thromboembolic disease.
Deep vein thrombosis of the lower limb is classified according to its location into proximal (external iliac vein, femoral, popliteal) and distal (calf veins). Proximal deep vein thrombosis is of greater clinical importance, as it is more frequently associated with severe risk factors (e.g., active cancer, congestive heart failure, respiratory failure, age over 75). In contrast, distal deep vein thrombosis is more often associated with transient risk factors (recent knee surgery, immobility, prolonged travel, among others) [2],[3].
Anticoagulation is recommended as an initial treatment for venous thromboembolic diseases. It improves survival after a pulmonary embolism, reduces the extent of deep vein thrombosis and possibly the recurrence of venous thromboembolism at three months [4],[5]. While three months is the standard duration of anticoagulation therapy, there are situations where the treatment length is unclear (e.g., recurrent venous thromboembolism, idiopathic venous thromboembolism, and patients with a permanent risk factor such as active cancer, antiphospholipid syndrome) [6],[7].
Despite current standard anticoagulation treatments, clinical outcomes are far from been optimal. Patients with deep vein thrombosis have a 30% recurrence within five years and a 40% risk of developing post-thrombotic syndrome within two years [8].
Recurrent venous thromboembolic disease is severe [9] and can be fatal in 3.6 to 10% of patients. Patients with idiopathic venous thromboembolic disease have a higher risk of recurrence [10]. Currently, there are clinical factors associated with an increased risk of recurrence of venous thromboembolic disease. Patients with transient risk factors such as surgery, trauma, or pregnancy are at low risk of recurrence and do not benefit from a prolonged duration of anticoagulation [11].
Risk factors associated with increased recurrence are the absence of transient risk factors, more than two thrombotic events, male sex, residual deep vein thrombosis [12], vena cava filter [13], estrogen use, diabetes mellitus, neurological disease with a motor deficit, active cancer, inflammatory bowel disease, and chronic kidney disease [14]. Also, the site of the first episode of venous thromboembolic disease appears to influence the recurrence rate. Deep vein thrombosis, pulmonary embolism, and the two latter diseases combined are the ordered spectrum of venous thromboembolic disease from the lowest to the highest recurrence [10].
In addition to clinical factors, there are some signs detected by Doppler ultrasound that may be associated with a higher recurrence rate [15],[16],[17],[18].
The D-dimer is the most studied laboratory variable associated with recurrence. This parameter predicts the risk of recurrence of venous thromboembolic disease during treatment or even after a complete course of oral anticoagulants in a first episode [19],[20],[21],[22],[23].
Objectives
We aimed to evaluate factors associated with the recurrence of thromboembolic episodes among patients with a first episode of venous thromboembolic disease during anticoagulation treatment and at least one year after treatment discontinuation.
Methods
Study population
We designed a dynamic prospective cohort of patients with a first episode of deep vein thrombosis who initiated anticoagulation therapy and were included in the Institutional Thromboembolic Disease Registry from June 1, 2015, to March 30, 2019.
Enrollment was based on the request for a diagnostic study. We considered a case of deep vein thrombosis when the disease was confirmed through a Doppler ultrasound from lower-leg veins territory. Patients who refused to participate or refused to give informed consent and those who had active cancer, or a permanently implanted vena cava filter were excluded. The study protocol was approved by the Ethics Review Board of the 'Hospital Italiano de Buenos Aires'.
A full-time investigator examined all patients since the diagnosis and updated the database during follow-up visits. The registry contained baseline demographics, clinical history, comorbidities, physical examination, and laboratory data. We also collected information on patients' D-dimer by ELFA method (a combination of Enzyme-Linked ImmunoSorbent Assay, ELISA, with a final reading by fluorescence with D-Dimer exclusion II VIDAS, Biomerieux), and ultrasound imaging. Patients were followed until death unless they were lost to follow-up. The follow-up frequency was at the discretion of the treating physicians.
Follow-up and definitions
Thirty days before treatment suspension, all patients had a D-dimer and ultrasound assessment. When patients completed at least a year from treatment discontinuation, they were also studied through an ultrasound analysis and for thrombophilia if they were younger than 55 years or had no known risk factors for venous thromboembolic disease. All patients were evaluated pre-suspension and at least one year after treatment for recurrence, bleeding (major and minor), and death at 30 days. Recurrence was defined as progression or a new symptomatic episode during and after treatment discontinuation [24]. Patients were no longer followed if they withdrew, moved away, died after the last complementary study, or completed at least one year of follow-up (after treatment discontinuation).
Statistical considerations
Quantitative variables were presented as mean and standard deviation or as median and interquartile range according to the observed distribution. Categorical variables were presented as proportions. The 95% confidence intervals were calculated for each recurrence, bleeding, and death estimator. The association of each variable with venous thromboembolic disease recurrence was tested using the Kaplan Meier estimator and the Cox Mantel test to compare univariate survival curves. Candidate variables included epidemiological data, laboratory determinations, and imaging measures of residual thrombus (that may help predict recurrence in venous thromboembolic disease after treatment discontinuation). A Cox proportional hazard model was constructed with the significant dichotomic explanatory variables in the univariate analysis. Each variable was presented with crude and adjusted hazard ratios and a 95% confidence interval. A P <0.05 was considered statistically significant, and STATA version 13 software was used for the statistical analysis.
Results
Participants
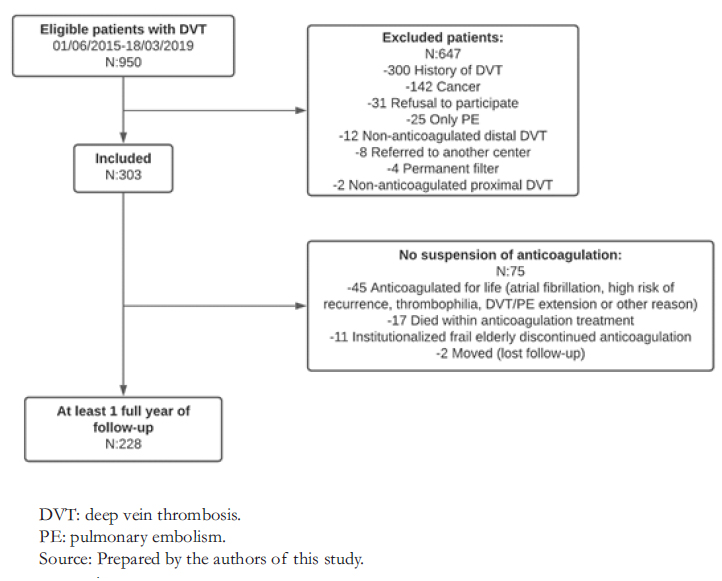
The institutional registry yielded 950 patients diagnosed with deep vein thrombosis between June 1 2015, and March 30 2019, of whom we excluded 647. The three leading causes of exclusion were patients with a previous venous thromboembolic disease (300, 46%), cancer (142, 22%), and patients with a health coverage different from the health plan of the 'Hospital Italiano de Buenos Aires'. Meanwhile, 303 patients met the selection criteria (Figure 1).
Table 1 shows the general characteristics of included patients.
 Full size
Full size 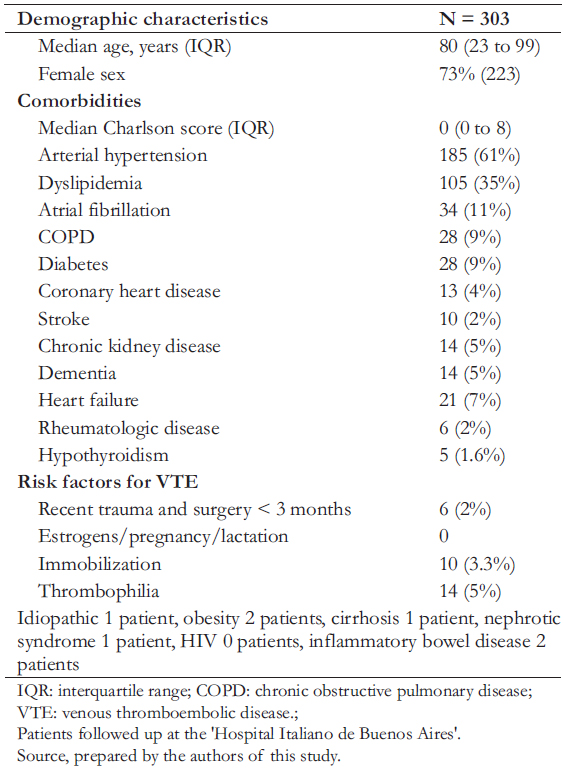 Full size
Full size Baseline and pre-suspension anticoagulation laboratory characteristics (N = 303)
The median baseline and pre-suspension D-dimer results were 5000 (interquartile range: 2600 to 5000) and 441 (253 to 657) nanograms per milliliter of fibrin equivalent units, respectively. The mean baseline hematocrit was 38% (interquartile range: 33% to 40%), the median leukocytes were 7838 (6622 to 9949), and neutrophils 69% (interquartile range: 60% to 77%). Regarding blood type and Rh factor, we only had information of 79 patients as follows: A 43% (34), AB 5.1% (4), B 16.5% (13), O 35.4% (28) and Rh-positive 92.4% (73).
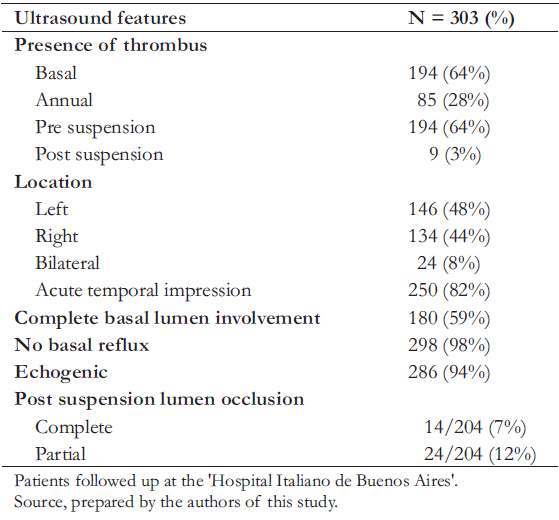
Ultrasound characteristics
At diagnosis, 13% (40) had whole leg involvement, and 11% (32) had proximal deep vein thrombosis. After treatment suspension, 19% of patients persisted with some degree of lumen occlusion. Table 2 shows the ultrasound characteristics.
 Full size
Full size Thrombophilia
The overall thrombophilia rate was 5% (N = 14, 95% confidence interval: 3 to 8), of which 36% (5) had factor V Leiden, 50% (7) antiphospholipid syndrome and 14% (2) prothrombin G20210A mutation. Among this group of patients, only one recurred within treatment (antiphospholipid syndrome), only six had their anticoagulation discontinued, and none recurred at one year.
Treatment
All patients received anticoagulation at the time of the thrombotic episode. The most frequent treatment drugs were acenocoumarol and enoxaparin. Table 3 shows the anticoagulants used to treat deep vein thrombosis. We found that 21% (64) of patients were still anticoagulated one year after the event. Some patients had to persist treatment due to atrial fibrillation (53%, 34), a high risk of recurrence (9%, 6), thrombophilia (8%, 5), and other unknown reasons. Among the 240 patients who discontinued anticoagulation, the median treatment was 6 months (interquartile range: 3 to 9 months). Table 4 shows the type of treatment given.
 Full size
Full size 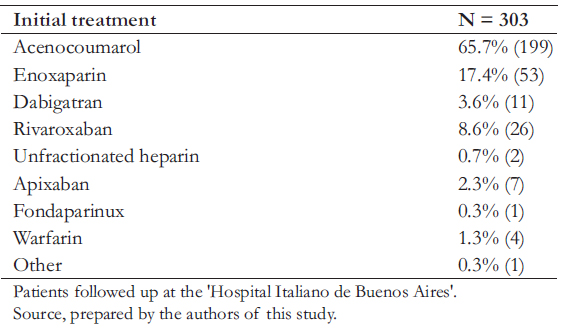 Full size
Full size Events
The recurrence rate during anticoagulation was 5% (N = 16/303, 95% confidence interval: 3 to 8), and during post-suspension follow-up was also 5% (N = 11/220, 95% confidence interval: 3 to 9). Of those who recurred, 40% (N = 6) were on treatment with acenocoumarol, 30% (N = 5) with enoxaparin and the remainder with unfractionated heparin, apixaban and rivaroxaban.
The overall bleeding rate was 13% (N = 39, 95% confidence interval: 9 to 17). We found that 5% (N = 16, 95% confidence interval: 3 to 8) had major bleeding and two patients died due to a hemorrhagic stroke. The rate of minor bleeding was 7% (N = 21, 95% confidence interval: 4 to 10).
Overall mortality was 17% (N = 53, 95% confidence interval: 13 to 22), of whom more than half died within the first three months (57%, 30/53).
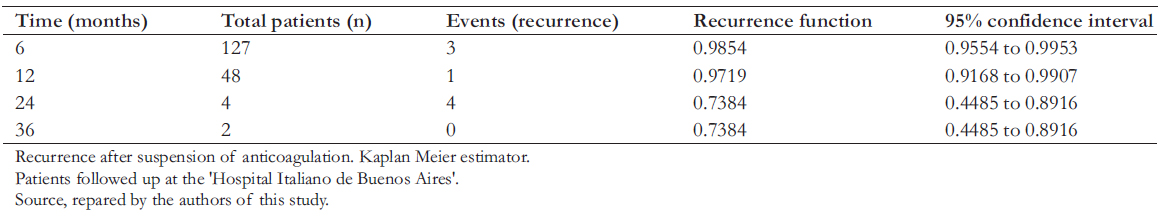
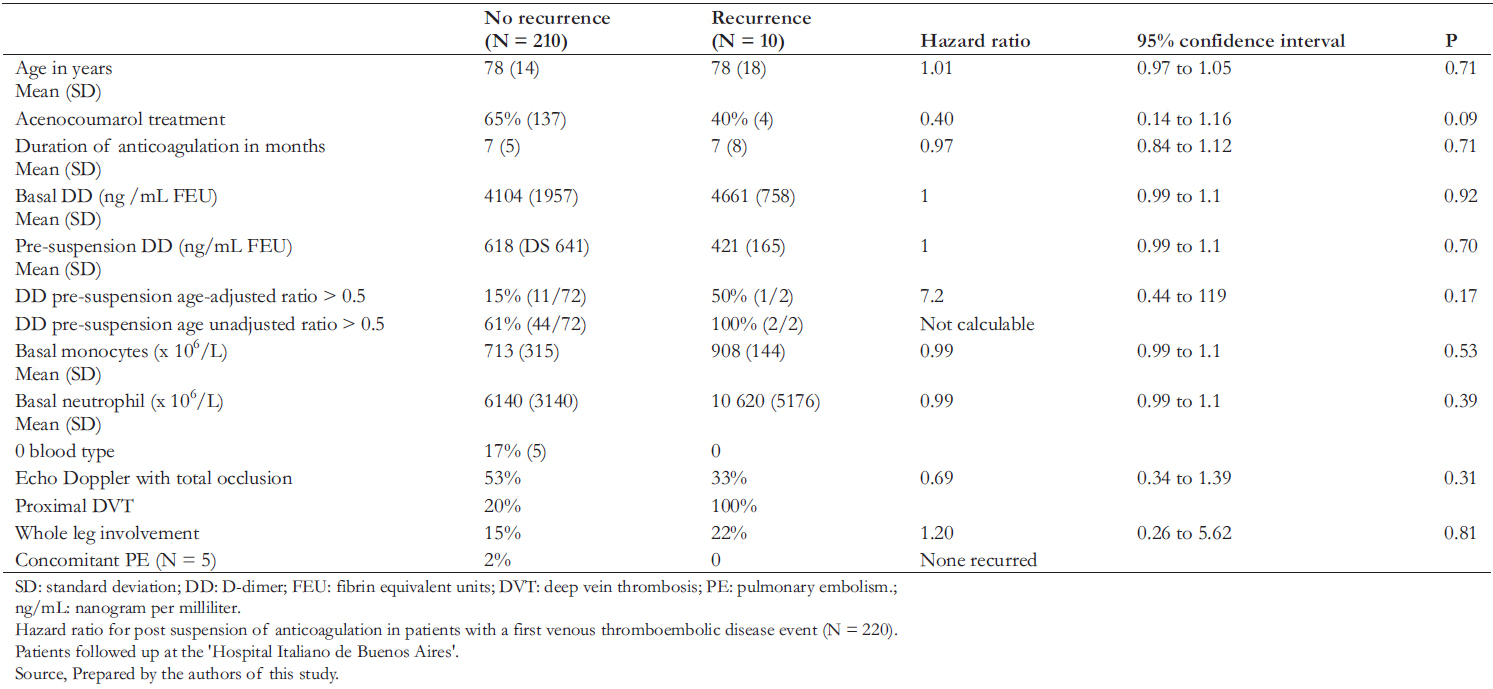
Recurrence after anticoagulation suspension
Patients with a post-suspension recurrence had a higher mean D-dimer and higher baseline neutrophil and monocyte counts. Patients who recurred after treatment suspension also had a higher frequency of complete leg involvement by ultrasound and received anticoagulation therapy for less time. However, no statistically significant differences were reached among the groups. Table 5 shows the crude hazard ratio for recurrence after suspension of anticoagulation.
 Full size
Full size Discussion
In this study, we evaluated factors associated with the recurrence of thromboembolic events in patients without cancer in the first episode of deep vein thrombosis. Recurrence was assessed within the anticoagulation treatment and one year after treatment suspension.
Low risk thrombophilias are associated risk factors for venous thromboembolic disease. Factor V Leiden and PT G20210A have a relative risk of five to seven and three to four for the first episode of venous thromboembolic disease, respectively. However, these characteristics do not significantly affect the risk of recurrence; they have been associated with an increased risk of recurrence of less than 1.5% [25],[26]. We found a very low prevalence of factor V Leiden and PTG20210A (1.8 and 0.7%, respectively), and therefore, an appropriate recurrence risk analysis associated with their presence could not be performed.
Concerning antiphospholipid syndrome, recurrence within treatment with vitamin K antagonists (with an international normalized range between two and three) was 3.7%. Prolonged anticoagulation is indicated in these high-risk patients [27]. We only found one patient with antiphospholipid syndrome recurring within the anticoagulation treatment. However, the prevalence of this disease in our population was 2.5%, which is lower than international literature reports (6 to 19%) [17].
Our study could not demonstrate that age, D-dimer, type or duration of anticoagulation, or a proximal location of the thrombus (those affecting the iliac-femoral axis with or without the involvement of the popliteal vein) were associated with recurrence. Very few patients presented recurrence in the time evaluated, and it is lower than other studies with longer follow-ups. The same limitation arose when we wanted to demonstrate that the extension of the thrombus and the presence of post-thrombotic sequelae are independent risk factors for recurrence [18],[28],[29].
We found that the overall bleeding rate in our study was relatively high (13%) and that incidence of major bleeding was 5%. In contrast, other studies found that an incidence of major bleeding between 1 and 4% [30].
This work has potential limitations. The post-suspension follow-up included at least the first year (some patients were followed up to 36 months, although it had a low N), so few events occurred. It is known that the recurrence rate increases over time [21],[28]. Therefore, the absence of association with factors known to increase the recurrence may be due to a short follow-up and a lack of statistical power (i.e., lack of sufficient N and few events, which is why cumulative frequencies are reported in outcomes).
As a strength, this dynamic cohort reflects real-world evidence, where patients are evaluated, treated, and followed differently than in clinical trials [22],[23]. The prospective follow-up of a cohort with closed characteristics ensures that the assessment of recurrence, bleeding, and death are accurate (patients are only seen at the 'Hospital Italiano de Buenos Aires', and all their consultation, studies, hospitalizations are recorded in the electronic medical record repository). Additionally, these data show real-world evidence in an elderly population (mean age 78 years).
Conclusion
In this work, we evaluated factors associated with recurrence of thromboembolic events in patients with a first non-cancer venous thromboembolic disease event, at least one year after treatment suspension, in a dynamic prospective cohort.
We found that patients who recurred had higher mean baseline D-dimer, higher neutrophils and monocytes, and more frequently had a whole-leg involvement by ultrasound and a shorter duration of anticoagulation therapy. However, these differences were not statistically significant, probably due to the small sample size and the low post-suspension recurrence rate associated with the short-term follow-up.
Notes
Contributor roles
MLPM, TGF, DG, FBQ: conceptualization, methodology, software, validation, formal analysis, research, resourcing, data curation, writing, first draft, review, revision, editing, visualization, oversight, project management, and obtaining funding. DM, NS, JR, FD, MM, FV: conceptualization and research.
Competing interests
The authors completed the ICMJE conflict of interest statement and declared that they received no funding for the completion of this article; have no financial relationships with organizations that may have an interest in the published article in the past three years; and have no other relationships or activities that may influence the publication of the article. Forms can be requested by contacting the responsible author or the Editorial Board of the Journal.
Ethics
The present study followed the considerations related to the care of clinical research participants included in the Declaration of Helsinki and the Guidelines for Research in Human Health (Resolution 1480/11) of the National Ministry of Health of Argentina. Moreover, this study was approved by the Ethics Committee for Research of the 'Hospital Italiano de Buenos Aires' (CEPI) for its development with protocol approval number 2151, dated November 7 2013.
Data availability statement
The database of this study is available upon request.
Funding
The work received funding from the 2011 Research Council Grant of the 'Hospital Italiano de Buenos Aires', Argentina.
Acknowledgments
Alejandra Romero, Juan Fornos, Akemi Zanella, Carolina Betancourth, Martina Aineseder.
Language of submission
Spanish.

