Comentarios
← vista completaPublicado el 15 de octubre de 2024 | http://doi.org/10.5867/medwave.2024.09.3008
Viruela símica: de la alerta a la práctica
Symic smallpox: From warning to practice
Background
Monkeypox, monkeypox, or MPox, is named after its initial detection in experimental monkeys in 1958. Following the eradication of human smallpox (1980), sporadic cases of monkeypox have been reported in some African countries, and an outbreak linked to imported animals in the United States (2003). On a larger scale, outbreaks were reported in the Democratic Republic of Congo (2005) and Nigeria (2017) [1]. In 2022, it spread via travelers to Europe and the Americas. Since then, more than 100 000 laboratory-confirmed cases have been reported, with more than 220 deaths worldwide [1]. On 14 August 2024, the Director-General of the World Health Organization (WHO) declared a public health emergency of international concern due to the increase in cases of smallpox in the Democratic Republic of Congo and its neighboring countries.
Disease origin and characteristics
Monkeypox is caused by a DNA-type virus of the genus Orthopoxiviridae. The virus has been genetically classified into two clades (I and II) and two subclades (a and b) each [2]. Both clades have different geographical, epidemiological, and clinical features. The West African clade (clade I) shows less than 1% fatality rates, and human-to-human transmission has never been documented. In comparison, the Congo Basin clade (also known as Central African clade or clade II) shows fatality rates of up to 11%, and documented human-to-human transmission of up to six sequential events has been observed [3].
The most common clinical manifestations are vesicle-like rashes on the skin, mucous membranes, or genitals, which may be itchy or painful and evolve into crusts, persisting for two to four weeks. The symptoms include fever above 38.5 degrees Celsius, lymphadenopathy, headache, myalgia, fatigue, and odynophagia. It is generally a self-limiting disease. However, its importance lies in the fact that there is no treatment, and some patients develop life-threatening complications [3]. The average incubation period is from 5 to 21 days [4], varying from 1.4 to 13 days [1].
It is transmitted by direct contact with an infected person, most commonly through sexual contact. Contact with vesicle secretions (skin and mucous membrane rashes) directly or through clothing, towels, or other fomites, as well as through saliva droplets, is also described as a potential source of interest. Cases of transmission to healthcare workers (through improper handling of personal protective equipment) and vertical transmission have been reported, with potentially fatal consequences for the fetus or newborn. Another transmission route is from infected animals to humans, either by handling the animal (dead or alive), contact with its secretions, or consuming its meat [2].
Those at most risk are immunocompromised patients, HIV carriers, and pregnant women. Severity and lethality are determined by complications such as bronchopneumonia, respiratory stress, dehydration, gastrointestinal disease, corneal infection with loss of vision, encephalitis, transverse myelitis, and myopericarditis, among others [3,5].
The clinical management of patients is based on the use of antivirals, symptomatic support, pain relief, and antibiotic treatment of bacterial complications [5]. However, antivirals have not yet been tested in clinical trials, making their availability difficult.
Epidemiological situation
Since January 2022, monkeypox cases have been reported in more than 120 countries, with over 100 000 confirmed cases and 223 deaths. Most of the cases reported in August 2024 are from African countries. In second place is the Americas region.
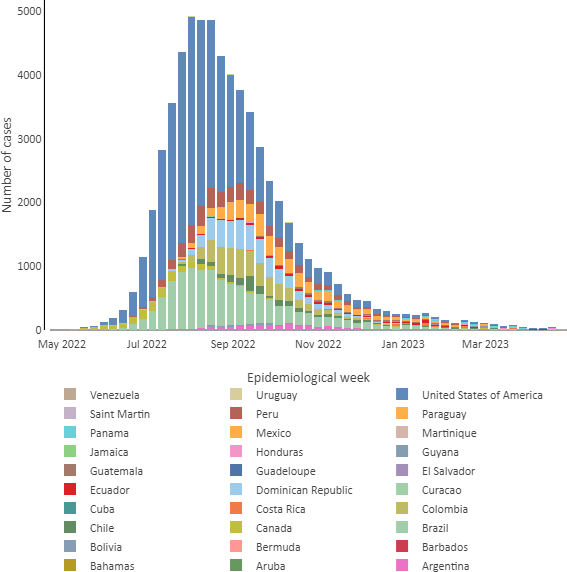
The ten most affected countries from 1st January 2022 to July 2024 are the United States, Brazil, Spain, the Democratic Republic of Congo, France, Colombia, Mexico, the United Kingdom, Peru, and Germany, accounting for 80% of the cases reported worldwide. Of these countries, half are in the Americas region [1]. Most of the reported cases in this region over the last two years have originated in healthcare services for patients living with HIV, sexual health checks, and primary or secondary healthcare services. The most frequent mode of transmission has been sexual contact between men who have sex with men [6]. Genomic surveillance most frequently identifies clade IIb of the virus [7]. Further details on the Latin American countries affected during the 2022 to 2023 outbreak are shown in Figure 1.
Confirmed cases of monkeypox by country/territory.
E14, 2022 to SE17, 2023. Pan American Health Organization. Mpox case board - Americas Region. Washington, D.C.: PAHO; 2024 [cited 2024 Sep 2].
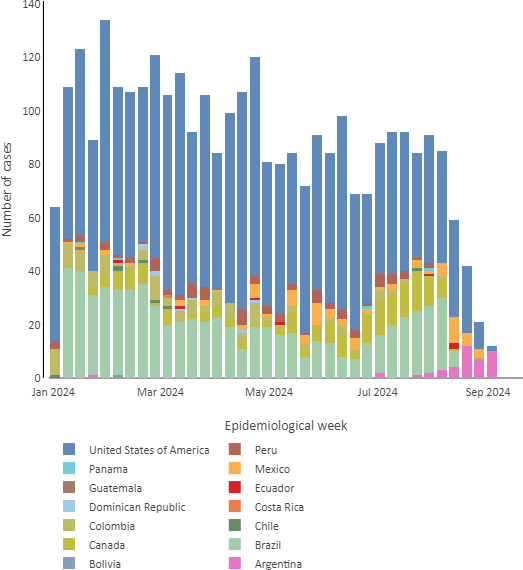
Between epidemiological weeks 1 and 38 of 2024, 13 countries reported new cases: Argentina (n = 8 cases), Bolivia (n = 1), Brazil (n = 702), Canada (n = 162), Chile (n = 7), Colombia (n = 111), Costa Rica (n = 1), Ecuador (n = 4), Guatemala (n = 1), Mexico (n = 53), Panama (n = 4), Peru (n = 77) and the United States (n = 1716 cases and one death). Figure 2 shows the current situation of confirmed cases of MPox in Latin America [7].
Confirmed cases of monkeypox by country/territory.
SE1, 2024 to SE38, 2024. Pan American Health Organization. Mpox case board - Americas Region. Washington, D.C.: PAHO; 2024 [cited 2024 Sep 2, 2024].
Control strategies
As with any infectious disease, epidemiological surveillance, early detection and diagnosis of cases, case isolation, and contact tracing are essential from a healthcare point of view to prevent its spread. Also, healthcare must be provided to cases while effectively protecting the healthcare team with preventive and biosecurity measures [7]. Given its side effects, the availability of an effective vaccine is limited and restricted to high-risk situations [4].
In terms of surveillance, healthcare teams must be aware of the regulations and their respective case definitions (suspected, probable, confirmed, re-infected) and have ready access to reporting systems. To this end, dissemination and training of healthcare professionals are recommended as part of sanitary alert activities [7].
Early detection includes laboratory diagnosis, performed by molecular techniques (PCR or polymerase chain reaction) on samples of vesicle secretions or skin lesions [2]. Molecular techniques are not usually part of the tests performed in clinical laboratories in primary healthcare facilities, although they are in some secondary healthcare facilities. It is likely that, following the SARS-CoV-2 pandemic, the techniques set up in these laboratories will allow rapid diagnosis at the local level. Authorities should take this situation into account. The WHO has called on laboratories and private companies to invest in manufacturing rapid test kits that facilitate diagnosis during a consultation or at the patient’s bedside without resorting to expensive molecular techniques [8]. Countries need to embrace genomic surveillance as a key part of their decision-making by making it possible to know which clades are circulating and where they come from.
Primary prevention with vaccination is another strategy used to prevent this disease. However, the vaccine is not recommended for large-scale use; rather, it is limited to specific situations of high risk of exposure. Side effects can be severe, ranging from fever, muscle aches, or headache to myocarditis, pericarditis, or encephalitis [4]. At least four types of vaccines are currently approved for use worldwide, summarized in Table 1.
WHO has called for efforts to focus on early detection, case diagnosis, contact tracing, and isolation to prevent the spread of the virus. This involves improving and disseminating knowledge of the disease among healthcare workers and the general population. Hence, risk communication is another fundamental pillar of control strategies, both for people to early identification of symptoms and consultation, as well as for them to apply appropriate infection prevention measures.
Risk communication guidelines should consider the disease’s epidemiology in each country. In Latin America, relevant information is available on the profile of cases reported during the 2022 to 2023 outbreak. The most frequent mode of transmission was sexual encounters (51%), 85% of whom were men who had sex with men, 48% were people living with HIV, and 84% had a prior history of travel [7]. In the case of Chile, cases were concentrated in young men (aged 30 to 39 years), among whom 53.5% self-reported having HIV infection, and 15% had another type of sexually transmitted infection [10].
From warning to action
While monkeypox had been considered rare and self-limiting, recent information suggests that complications can be life-threatening. On the other hand, the frequency of infection and its spread between countries and continents has also increased, and it is now considered a public health concern. Given this perspective, it is necessary to build the capacity of healthcare systems to act and prepare for an epidemic threat. To this end, immediate epidemiological surveillance is essential, as it provides valuable information that guides the development of appropriate control strategies.
The basic premise of epidemic control is blocking transmission, which means that once the transmission mechanism is known, it is interrupted to prevent transmission from one case to those around it. For monkeypox, this strategy translates into several actions. First, early case detection and isolation measures. For this, there must be good risk communication to make it easier for people with a history of risk factors to recognize the symptoms and seek medical advice. Secondly, healthcare workers must know how to recognize the disease, request confirmatory diagnostic tests, and provide preventive isolation measures and treatment for each patient. At this stage, healthcare workers are also responsible for initiating surveillance and notifying the competent healthcare authority of each case to continue with the next step. In turn, compliance with universal precautions standards by healthcare personnel will ensure that they remain free of contagion. Third, epidemiological teams initiate active surveillance, locating contacts of the case to record their history and isolate them. The isolation of contacts includes surveillance of their clinical status and counseling on prevention measures for the outbreak’s spread. Depending on the situation, vaccination may be considered. This can be done up to four days after contact with the sick person or up to 14 days if the person has no symptoms [2].
In addition, it is possible to envision other critical issues, such as early screening of groups at risk and rapid diagnosis. Establishing sentinel surveillance in healthcare services for patients with HIV or other sexually transmitted infections may be a good strategy for Latin America, given the profile of cases in the 2022 to 2023 outbreak. In such contexts, rapid testing would be helpful. Dissemination of transmission and prevention information at airports or to travelers is also advisable, given that most cases had a history of travel to places where the outbreak had already started. Vaccination of travelers in areas of virus circulation could also be considered a reasonable preventive measure. However, it should be considered that widespread transmission of the disease and the mass use of vaccines contribute to the likelihood of virus mutations that result in increased pathogenicity and eventually increase its pandemic potential [3,11].
Conclusions
In short, controlling monkeypox is more manageable than controlling an airborne disease such as SARS-CoV-2, which asymptomatic people also transmit.
Whether this alert does not turn into a sanitary emergency will depend on how countries prepare for the epidemic alert. To this end, the main pillars are risk communication (with an initial emphasis on travelers), passive and active epidemiological surveillance, and early detection. These, together with the updating of knowledge and awareness of health personnel regarding this disease, favor the timely control of contagions.

