Comentarios
← vista completaPublicado el 16 de junio de 2020 | http://doi.org/10.5867/medwave.2020.05.7935
Asignación ética de recursos sanitarios escasos en el contexto de crisis por COVID-19
Ethical allocation of scarce health care resources in the context of the COVID-19 crisis
Abstract
The current COVID-19 pandemic has the potential to overwhelm the capacity of hospitals and Intensive Care Units in Chile and Latin America. Thus local authorities have an ethical obligation to be prepared by implementing pertinent measures to prevent a situation of rationing of scarce healthcare resources, and by defining ethically acceptable and socially legitimate criteria for the allocation of these resources. This paper responds to recent ethical guidelines issued by a Chilean academic institution and discusses the main moral principles for the ethical foundations of criteria for rationing during the present crisis. It argues that under exceptional circumstances such as the current pandemic, the traditional patient-centered morality of medicine needs to be balanced with ethical principles formulated from a public health perspective, including the principles of social utility, social justice and equity, among others. The paper concludes with some recommendations regarding how to reach an agreement about rationing criteria and about their implementation in clinical practice.
Hopefully, the containment procedures adopted in Chile and other countries in the region manage to flatten the epidemic curve enough so that the collapse of health-care systems can be avoided. However, given the uncertain effectiveness of these measures, the experiences seen in other countries and warnings of experts, local authorities have an ethical obligation to be prepared, first, by taking all the appropriate measures to prevent the country from reaching a situation where we have to ration ICU admission among patients who need it. To achieve this goal, it is necessary, among other measures, to set up protocols, coordinate action, increase the number of ICU beds with access to mechanical ventilators, and to give adequate training to health-care teams.
Second, given a situation of extreme rationing, it is paramount to identify ethically acceptable and socially legitimate criteria for the distribution of limited health-care resources. The criteria must be ethically acceptable in the sense of having a solid foundation of recognized moral values and principles. As I argue later, the incorporation of principles of public health ethics is crucial and necessary to prevent negative consequences to both health-care professionals and the community at large. Social legitimacy, meanwhile, requires the participation of civil society in generating these criteria, including the definition of which principles and values are morally relevant.
Likewise, the academic community is called upon to actively participate in this debate, supporting the government and civil society in making decisions in times of crisis. At the time of writing this article, the main contribution in Chile has been given by the Center for Bioethics of the Pontifical Catholic University through two separate documents (in Spanish) entitled “Ethical Guidelines for Medical Decisions in the Context of the Pandemic in Chile" and "Ethical Guidelines for the so-called ‘problem of the last bed’” (hereafter, PCU Ethical Guidelines) [1],[2]. In what follows, I will make a brief analysis of these important documents, then discuss moral principles relevant to the ethical foundation of appropriate criteria for rationing during the COVID-19 pandemic. My goal will be to provide an ethical framework for deliberation and to offer some recommendations. The definition of specific criteria for rationing goes beyond the scope of the present paper.
The PCU Ethical Guidelines take as a starting point the “centrality of the person in the clinical relationship and care” and then develop recommendations focused on the wellbeing of the patient and the protection of the doctor-patient relationship. Procuring the good of the individual patient makes up the basis of traditional clinical ethics, dates back to Hippocrates, and prevails in contemporary bioethics through the principles of beneficence and respect for persons[3],[4]. The PCU Ethical Guidelines are timely in highlighting these principles and reminding us that “despite the shortage of resources, one cannot give up taking care of every patient.” Nevertheless, it is important to keep in mind that in a pandemic, there can be severe constraints on the ability to deliver the care that patients need.
Facing this challenge, the PCU Ethical Guidelines recommend “doing what is proportionate to the clinical condition of the patient” and “in patients for whom access to an ICU is considered disproportionate, [making] the decision to adapt the therapeutic effort.” ICU doctors are familiar with the principles of proportionality and adequacy of therapeutic effort. These are applied in cases where medical interventions, especially those of critical care, are unlikely to result in a net benefit to the patient[5],[6]. Nevertheless, given the present context, these recommendations have the limitation of focusing ethically on the individual patient. They answer the question: is it ethically correct to decide to admit this patient into the ICU, instead of not doing so? Yet, the question that summons us is another: is it ethically correct to decide to admit this patient into the ICU, instead of this other patient?
The extent to which physicians have duties beyond those determined by the interests of the present patient, such as duties to other members of society, remains controversial[7]. But few would dispute that under exceptional circumstances, such as war and national emergencies, doctors do have to take into account the interests of society[8]. In these cases, the traditional patient-centered morality of medicine needs to be balanced with ethical principles and values formulated from a public health perspective[9],[10],[11],[12]. This is not to deny that health-care professionals, especially those working with scarce resources, sometimes do incorporate a social perspective into their decision-making[13]. My claim is that in a public health emergency, health-care decisions should integrate public health ethical principles explicitly, systematically, and transparently. What are those principles? A good starting point is to consider three principles commonly used to justify the rationing of health-care resources: social utility, social justice, and equity, broadly accepted principles in the specialized literature, although sometimes used under different denominations [14],[15],[16],[17],[18]. I will now briefly present how these principles can be applied to the current COVID-19 pandemic.
The principle of social utility refers to maximizing net benefits but transferred to the field of public health. In situations of crisis, this principle usually translates into saving the most number of lives, which is consistent with the inherent value universally placed on each human life[19]. To this end, priority should be given to patients who most need and are most likely to benefit from critical care interventions, a decision that can be aided by clinical assessment scales[20],[21]. In order to estimate social utility, it is also appropriate to consider the years of lives saved[18]. It is difficult to question that in a situation of extreme rationing, a patient with a good prognosis and long life expectancy, should have priority for the last bed in an ICU over another patient with short life expectancy (e.g., due to cancer). The complexity of making these estimates should not be an excuse to undermine their importance. To reduce the mortality and morbidity caused by COVID-19 should be a priority both from a clinical and a public health point of view.
In broad terms, the principle of justice refers to a fair, equitable, and appropriate distribution of benefits and burdens in society[3]. This principle can be defined in many ways. For the present purposes, I refer to social justice as the widely accepted view that a just allocation of resources should give priority to those who are worse off or in greater need[4],[14],[22]. In other words, it is not enough to maximize the benefit of society if this generates or exacerbates social injustices. For example, maybe the most efficient way of distributing health-care resources in Chile is to concentrate ICU beds in the central region of the country, where most of the population lives. Even if this allowed maximizing social utility, it would not be fair to implement this measure if it hampers access to resources to people living in the extreme and historically disadvantaged regions of the country. In practice, applying the principle of social justice is challenging because there are many dimensions in which people can be disadvantaged, e.g., due to sickness, low resources, or because they have not yet had the opportunity to enjoy the different stages of life[18]. This highlights the need for input from different disciplines when it comes to applying this principle, especially at the macro-level of resource allocation.
According to the principle of equity (which can also be considered a requirement of justice), everyone who needs health-care resources should have an equal opportunity to access them, however when resources are allocated one has to weight relevant moral considerations such as those deriving from the two previous principles. Under normal conditions, access to the ICU and general medical attention is established, in part, on a first-come, first-served basis. This system is equal for all and is not problematic as long as those who arrive late will not be left unattended. But in a public health emergency, this may not be enough. While patients with a poor prognosis are connected to mechanical ventilation, others with better prognosis or greater need, due to arriving late, can be left without access to this resource. Even if the principles of social utility and social justice, are not taken into account, limiting access on a first-come, first-served basis ends up being inequitable and can result in fewer lives saved. The most ethically appropriate formula perhaps is that among patients who are roughly equivalent according to the previous principles, randomly select those who will be admitted[9],[19]. In practice, however, some instances of first-come, first-served to health care may be hard to avoid[23].
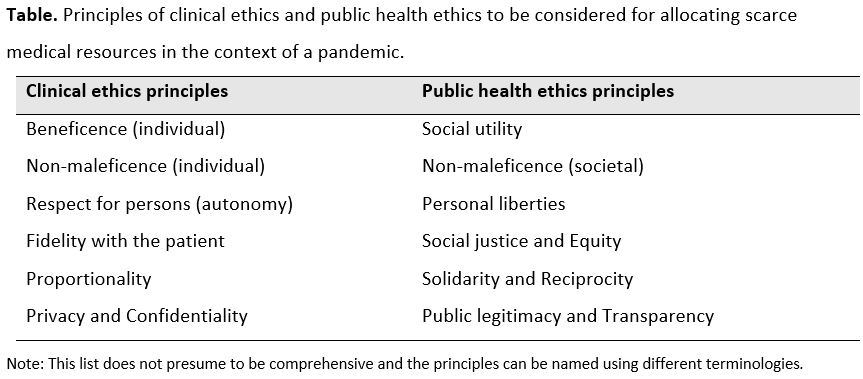
The PCU Ethical Guidelines briefly discuss several of the criteria just mentioned. However, they describe them as unfair and discriminatory on the basis that “they do not focus on the central point of medical care: the patient, including his or her objective condition and context,” creating a false dilemma between clinical ethics and public health ethics. Although a situation of extreme rationing calls for a shift from an individualist to a public health approach, that does not mean that we should overlook clinical ethics. Duties such as not abandoning the patient, or respecting prior wishes or advanced directives, acquire particular relevance in this context. However, as with most ethical controversies, we need to find the right balance between competing principles, which, in this case, stems both from clinical and public health ethics [Table]. It is true that, when viewed individually, none of the mentioned principles of public health ethics are likely to be sufficient or entirely satisfactory. But the controversy does not lie here. In the present scenario, where public health principles are inescapable, the challenge is to combine them with other ethically relevant principles in the best possible way[19],[24]. Indeed, this approach is consistent with most international ethical guidelines, including those published by medical societies in Spain and Italy during this present pandemic[25],[26].
The principles of social utility, social justice, and equity are essential, but they are not exclusive of other principles of public health ethics relevant in the present context [Table]. For reasons of space, I will only comment on some additional principles that I consider especially relevant. The principle of solidarity refers to the unity and cooperation between communities based on the common interest in fighting the pandemic[27]. Health institutions in areas with more resources or otherwise less affected by the crisis must be willing to support those most affected. The principle of reciprocity, for its part, requires that those who put their health at risk by helping to combat the pandemic receive adequate compensation, such as is the case of health workers who must assume a high physical and emotional cost. There is a consensus that this group should have some priority to access health care in extreme rationing circumstances[14],[19]. The principle of social utility also supports the need for this particular treatment since health workers play a critical and instrumental role in fighting the pandemic[28]. Finally, it is worth stressing that the process for defining criteria for rationing scarce health-care resources should satisfy the principles of public legitimacy and transparency. In addition to being based on recognized moral principles, the chosen criteria must be transparent and understandable to the public, as well as being available for discussion and review[29].
 Full size
Full size The COVID-19 pandemic confronts us with the duty and the ethical challenge of formulating ethically acceptable criteria for potential rationing of health-care resources that should apply to both patients with and without COVID-19. The grounds of these criteria cannot be reduced exclusively to clinical or public health ethical principles, but result from an adequate balancing of both normative dimensions. When it comes to agreeing on allocation criteria, the contributions of experts from all the relevant areas (including physicians) are as significant as including the participation of civil society. There are procedural issues regarding what is the fairest and most legitimate way to reach such an agreement that cannot be addressed here[30], but it is worth noting that the social committee created by the Chilean government to deal with the current pandemic can provide a useful platform. What is clear, though, is that without well-defined rationing criteria, health-care professionals will be forced to make life and death decisions without the necessary tools, and might be deemed as arbitrary and unfair. This situation, in addition to saving fewer lives, would cause an enormous emotional cost and risk of moral distress in health care professionals [31]. For all of these reasons, there should be predefined criteria applied consistently by professionals in roles outside direct patient care, for example, through triage committees (or similar entities) set up in the relevant health-care facilities [10],[19],[24],[32].

