Editorial
← vista completaPublished on October 1, 2015 | http://doi.org/10.5867/medwave.2015.08.6273
Clinical trials and study reporting - CONSORT guidelines at the forefront
Los ensayos clínicos y su publicación - las guías CONSORT en primer plano
Introduction
The so-called and known "randomized controlled clinical trial", is the leading type of research design in the arsenal of biomedical research, particularly epidemiological research. The reason is simple: it stands as the only research design considered truly experimental and the experiment represents the fastest and most effective way of development of scientific knowledge.
In the language of clinical and epidemiological research, the clinical randomized controlled trial is the research design with less risk of bias. Bias is the nightmare of all epidemiological research and has been and remains the subject of articles, reflections and essays on methodology of epidemiological studies [1],[2],[3]. Unfortunately, clinical randomized controlled trials are used only in research that assesses therapeutic or preventive procedures because these are the only objects of research that have overcome the strong barrier of ethics in research involving human beings. For ethical reasons, the experiment is banned except when it comes to conduct a clinical trial to evaluate a therapeutic or preventive action after being approved by the competent authorities, i.e. the ethics committees for research [4].
Designing randomized controlled trials
The purpose of the clinical trial design –as an experiment- is to isolate the study of all influence other than the objective of evaluating differences between treatments. The fundamental goal is to have equal groups in every way except for the therapeutic or preventive procedure assessed, so that whatever the outcome, can be attributed only to the procedure under consideration. On this basis we can formulate the so-called three golden rules of the design of a clinical trial which are aimed at confronting the most important biases in this type of research, since they directly threaten the chimerically desired similarity between groups [5].
- Randomization. Avoids susceptibility bias. Randomization is specifically aimed at achieving baseline comparability of groups since is responsible for achieving initially similar groups around, both in what is known as potential confounders, and in that which is unknown.
- Concurrent comparison. Avoids performance bias. Simultaneous (or concurrent) comparison implies that all treatment groups must be run in the same temporal and spatial context. It intends to avoid differences in external procedures (not directly assessed though necessary in health care) introduce unwanted dissimilarities between treatment groups that might lead to possibly confused results.
- Objective observation. Avoids detection and follow up biases. A measure intended to prevent differences arising from subjectivity -inevitably present in providers, patients and evaluators- miscarry the necessary similarity between the groups. It is the rule that requires the controversial use of placebos, unavoidable headaches of research ethics committees.
Figure 1 provides a schematic of the design of a clinical trial, illustrating the most important biases and the three rules above mentioned.
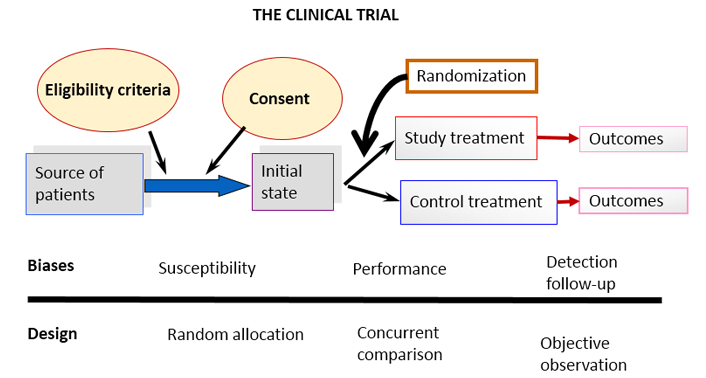
Figure 1. Schematic diagram of a basic clinical trial and potential sources of the most common biases.
All design elements, which have been introduced over time and shape modern clinical trials, are related to the effective implementation of these three golden rules. Consider, for example, intention to treat analysis [6] This rule forces researchers to include in the analysis of the results, paradoxically, those participants who were unable to complete the trial. The confusion generated in research-beginners (usually honest, so we think) is very high. The question is how to include in the results someone who withdrew or someone who had an accident and could not attend scheduled appointments. Well, the way to do it has already been conceived -that is what both the "last value carried forward, (LVCF)" and the “worst scenario” are for. The reason for doing it is related to possible "convenient" dissimilarities between groups, deliberately introduced by unscrupulous researchers prompted by the –yet more unscrupulous multinational pharmaceutical companies- as has already been reported in various scientific forums and in particular discussed in our journal [7].
More elaborate methodological elements of clinical trials in the narrow framework of an editorial in the Journal is impossible; methodological literature on clinical trials currently includes thousands or perhaps hundreds of thousands of articles, books, monographs and other scientific media.
The reporting of results of clinical trials
The cycle that links research with the application of its results in social practice inevitably passes by its publication (Figure 2).
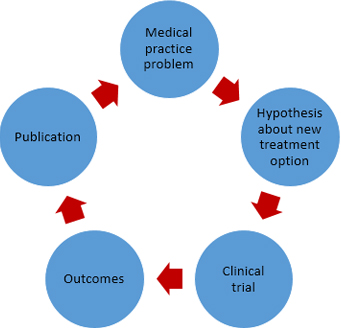
Figura 2. Simplified schematic of relationship between medical practice, therapeutic research and publishing results.
Publication of the results of a clinical trial is a requirement of good clinical practice (the name given to the "international ethical and scientific quality standard for designing, conducting, recording and reporting trials that involve the participation of human subjects" [8]). It is also a requirement for research ethics and researchers (see Articles 35 and 36 of the Declaration of Helsinki, the latest version, October 2013) [9] and a former editorial in Medwave [10]. Furthermore, it is undoubtedly a rule of common sense. How not to publish the results of a study that has consumed considerable human and material resources? How to deprive the scientific community of a research result on this scale? How to deprive society of such a result? Even more, why contribute to unnecessary repetition of studies already carried out, leaving results unpublished?
Strangely enough, the fact is that the non-publication of research results (particularly from clinical trials) is a relatively common problem that worries today all of us who advocate a research practice born of ethics and honesty- and results in a bias not mentioned before that, this time, is not linked to research design itself [11]. A bias that leaves us helpless to fight for a medical practice that stems from scientific evidence and against which the weapons we have today are not enough. This is the so-called publication bias, i.e. the distorted idea that may be generated in the scientific community (and in the nonprofessional public); because some research results (in this case of clinical trials), are not published.
Unfortunately, there is proof that non-publication occurs not by chance and the tendency is not to publish results unfavorable to the hypotheses. The consequence of this bias is a false magnification of the goodness of therapeutic or preventive measures that can undoubtedly have a negative impact on society. Publication bias is today under study and discussion in scientific fields of various kinds [12],[13],[14].
Let us go on with the reporting of clinical trials. The first is to emphasize that the report should reflect in detail the trial design, in short, how the three aforementioned golden rules were met and all other issues added to them: eligibility criteria, treatment details, definition and operationalization of primary and secondary variables and even the way in which data is processed and analyzed.
An introduction is also necessary, i.e. substantiate the clinical trial (which must be from the initial project of course). Regardless of the barrier of going through an ethics committee, the investigator must bear in mind that experiment on humans is permissible only if it is supported by a strong scientific rationale.
Without overwhelming the reader, the results of clinical trials should be clear and transparent; a synthesis that allows the corresponding generalization is necessary; and confidence intervals for the effects are essential. Without them, readers will not have an accurate picture of the magnitude of the effect achieved, whether or not significant differences arise. Much has already been discussed about the ineffectiveness of p values and the difference between statistical significance and clinical significance [15],[16],[17].
Discussion of results is the weakest point but also necessary in the report of an investigation, particularly a clinical trial. The reader not only has the right to identify the results but to participate in the authors´ reflections about them and distinguish their place in in what is already known.
Having outlined the above, we come to what is probably of most interest to our readers / authors / researchers. How you can definitely make a good report of the results of a clinical trial that allows a decent publication? The answer could be complicated because writing in summary, without avoiding important questions on the foundation, the method and the results of a study that has spent time, resources, and in particular, knowledge and skills, is not a simple task.
Some history about CONSORT
Fortunately, in 1994 –as a consequence of the repeated allusions to reports of poor quality of clinical trials in medical journals and various disquisitions about this topic that worried publishers, medical scientists and health authorities- two articles proposing a structured way to report clinical trials were published. One of these was a special communication of the Journal of the American Medical Association (JAMA) [17] and the other a position paper of the Annals of Internal Medicine [18]. Both articles reported the ideas of two groups that worked independently in the search for a systematic and structured way to publish results of clinical trials: the Standards of Reporting Trials Group and the Working Group on Recommendations for Reporting of Clinical Trials in the Biomedical Literature.
In 1995, an editorial in JAMA [19] made a call for the union of these two groups in order to achieve a properly combined proposal. Both groups were receptive to this call and in 1996 came out the first version of a guide for reporting the results of clinical trials which was the product of the conjoined work of the first two groups [20]. It was first published in JAMA and the BMJ reported almost immediately adherence to the newly published guides and basically reproduced their statements [21].
The new guide took the title of CONSORT, which is the acronym of its name in English: Consolidated Standards of Reporting Trials. In 2001, the first major revision of the initial guidelines was published simultaneously in three prestigious medical journals: Annals of Internal Medicine [22], JAMA [23] and Lancet [24].
CONSORT 2010 and Medwave
In 2010, a third revised CONSORT statement appeared. This time published by eight medical journals, some of them open access like PLoS Medicine [25], and BMC Medicine [26].
In addition to the initial guides and their two subsequent revisions directed to the basic design of a parallel trial, some extensions have been published for clinical trials with different specificities until today. We may distinguish CONSORT for non-inferiority studies [27]; CONSORT for cluster trials [28]; CONSORT for pragmatic trials [29]; and the one referred to studies of non-pharmacological treatments where trials for assessing surgical procedures, and rehabilitation therapies among others would be included [30].
The argument behind a good report of a clinical trial can be summarized in the words of Douglas G. Altman [21]:
Like all studies, randomised trials are open to bias if done badly. It is thus essential that randomised trials are done well and reported adequately. Readers should not have to infer what was probably done, they should be told explicitly. Proper methodology should be used and be seen to have been used.
The guide contains the basic CONSORT 2010 checklist with 25 items, some with sub-items, which actually gives 37 aspects that must be reported. The guide also suggests that the author include a patient flow diagram, which clearly displays the number of eligible participants, and the number that was lost in each subsequent stage; it contains a concrete proposal illustrated with a picture of how to do this flowchart. CONSORT is not limited to aspects of the method used to conduct the clinical trial but also includes elements of the introduction, the reporting of results and the discussion about them.
The author is thus committed not to forget the report of all aspects included in the guide or ultimately explain why some of the aspects, if any, was not completed. What we can call "good news" in this context is that researchers should identify and consider the CONSORT guide items not only when reporting their results, but also, since the planning of the trial.
As announced in the CONSORT website (http://www.consort-statement.org/about-consort/endorsers), over 600 biomedical journals and several publishers’ organizations such as the International Committee of Medical Journal Editors (ICMJE) and the World Association of Medical Editors (WAME), support CONSORT today. A systematic review published in 2012 suggested that the use of CONSORT effectively improves the reporting of clinical trials [31].
Our Journal supports the CONSORT initiative and promotes its use by including the CONSORT guidelines among the documents that authors of clinical trials reports should review before submitting a manuscript to the journal evaluation. There is also a strong recommendation in the instructions to authors to "follow the standards recommended by the international initiative known as the Equator Network (Enhancing the Quality and Transparency of Health Research)" where CONSORT appears.
Conclusion
Clinical trials are the most efficient and effective way to evaluate the adequacy of a new therapeutic or preventive measure. Their use for this purpose contributes decisively to provide society of new treatments that ultimately really improve the quality of life of human beings. For this reason, it is not enough to conduct a clinical trial with the utmost rigor but its results should be published in the spaces aimed for this purpose and at the right time. CONSORT guidelines in its different variants are today the best pattern or model to produce an optimal report on the foundation, the methods and the results of a clinical trial.
Notes
Conflicts of interest
The authors declare no conflicts of interest with the subject of this article.

