Reporte de caso
← vista completaPublicado el 15 de enero de 2025 | http://doi.org/10.5867/medwave.2025.01.2958
Infiltración vaginal para el alivio del dolor neuropático post histeropexia sacroespinosa: primer reporte exitoso a mediano plazo
Vaginal infiltration for relief of neuropathic pain after sacrospinous hysteropexy: First successful mid-term report
Abstract
Female genital prolapse, especially apical prolapse, significantly affects women’s health and quality of life. Sacrospinous hysteropexy is a widely used surgical procedure to address this condition, presenting few postoperative complications. However, one of the reported complications is neuropathic pain resulting from damage to the branches of the pudendal nerve. Despite the frequency of this complication, there are few standardized management alternatives. This article presents a clinical case of a 62-year-old patient who experienced persistent neuropathic pain after a sacrospinous hysteropexy, in whom traditional approaches such as physical therapy and medications were ineffective. Therefore, it was decided to perform a corticosteroid infiltration in the painful sites via the vaginal route with local anesthesia. The patient experienced immediate pain relief, which lasted for months without the need to repeat the infiltration. The available literature is scarce regarding the long-term success of this therapeutic technique, so this case highlights the potential mid-term efficacy of this alternative in managing postoperative neuropathic pain. This case contributes to the growing evidence that corticosteroid infiltration can be a viable option for the treatment of postoperative neuropathic pain, offering an improvement in the quality of life of affected patients. While this case shows an initial successful approach, further research is needed to validate and establish the applicability of vaginal corticosteroid infiltration in similar cases.
Main messages
- This study presents the case of a 62-year-old female patient who experienced persistent neuropathic pain after sacrospinous hysteropexy.
- Corticosteroid infiltration associated with analgesics via vaginal route with local anesthesia was used as treatment, resulting in immediate and long-lasting pain relief.
- This case highlights the potential medium-term efficacy of this therapeutic technique.
Introduction
Genital prolapse significantly impacts those affected’s well-being and quality of life, with apical prolapse being the second most prevalent condition after anterior wall defect [1]. Risk factors include childbirth, age, or history of hysterectomy. One of the techniques described to address this problem is the fixation of the vaginal vault to the sacrospinous ligament [2]. This surgical procedure is widely used. It is safe and effective in the treatment of apical prolapse, resulting in permanent attachment of the vaginal vault through fibrosis and healing of the sacrospinous ligament [3].
Although postoperative complications related to this surgical method are generally rare and of mild severity [2], neuropathic pain is the main one to keep in mind as a consequence of damage to the pudendal nerve branches. The pudendal nerve is both sensory and motor, originating from the sacral segments S2 to S4. It exits the pelvis through the greater sciatic foramen. It passes around the sciatic spine and back into the pelvis through the lesser sciatic foramen, passing through Alcock’s canal, also called the pudendal canal. This nerve innervates different structures of the perineum, including pelvic floor muscles and external genitalia. In the suspension of the vaginal vault to the sacrospinous ligament, there is a risk of injury to the pudendal nerve, given its proximity to the sacrospinous ligament near the sciatic spine, which can cause neuropathic pain or sensory dysfunction in the perineum [4]. Clinically, it can manifest as pain in the gluteal and posterior thigh region and can occur at variable rates between 6.1 and 15% [5]. Despite this complication, there is a lack of standardized management, with interventions ranging from physiotherapy to pharmacological approaches.
We present a case report of neuropathic pain after sacrospinous fixation. This case was successfully managed by vaginal infiltration of corticosteroids in painful sites identified on physical examination. The procedure was performed under local anesthesia, and the patient was discharged on an outpatient basis. The patient’s pain relief was immediate and was maintained during the following months of follow-up. This alternative was chosen due to the lack of improvement with the physical therapy and pharmacological approach.
Case report
Sixty-two-year-old patient with a history of four deliveries (three vaginal and one cesarean section) reported a one-year history of vaginal lump sensation associated with a feeling of heaviness. Physical examination revealed anterior genital prolapse stage 3 (Ba +2), posterior stage 2 (Bp 0), and apical stage 1 (C -3). The main demographic characteristics are detailed in Table 1.
After evaluation by the female pelvic floor team at the hospital, it was decided to perform an anterior repair with bilateral sacrospinous hysteropexy. The technique described for the Anchosure® kit was used and performed on December 28th, 2022. After surgery, the patient experienced left gluteal pain, with an intensity of 8/10 on the visual analog scale, which radiated to the anal region and the ipsilateral lower extremity.
Due to the characteristics of the pain, its location, and irradiation, and because it started after the surgical procedure, where there is a possibility of nerve injury, a neuropathic lesion of the pudendal nerve was suspected. Therefore, medical treatment was started with pregabalin at a dose of 75 milligrams per day. Along with pharmacological treatment, specialized pelvic floor physiotherapy was indicated to alleviate the symptoms, which was interrupted after five sessions due to persistent pain. At the end of therapy, the patient reported constant and persistent pain of 8/10 on the visual analog scale. Given the lack of response to the treatment, surgical infiltration of the painful points on physical examination and in the suture area with Anchosure® was decided, mainly over the left region.
The procedure took place in the outpatient procedure room, where direct vision under a speculum was used. Painful spots were identified on palpation with a cotton swab in the left lateral fornix and adnexal region (Figure 1). A sterile technique was applied, and infiltration was performed using a Perican® 18G - 1.3 x 80-millimeter spinal needle in the painful points. The solution contained physiological saline (3 milliliters), plus betamethasone acetate 3 milligrams per milliliter (3 milliliters), betamethasone disodium phosphate 3 milligrams per milliliter, lidocaine 2% (3 milliliters) and bupivacaine 0.5% (3 milliliters) (Figures 2 and 3).
Identification of painful spots in the posterior fornix.

Source: Photograph taken by the authors.
Infiltration set.
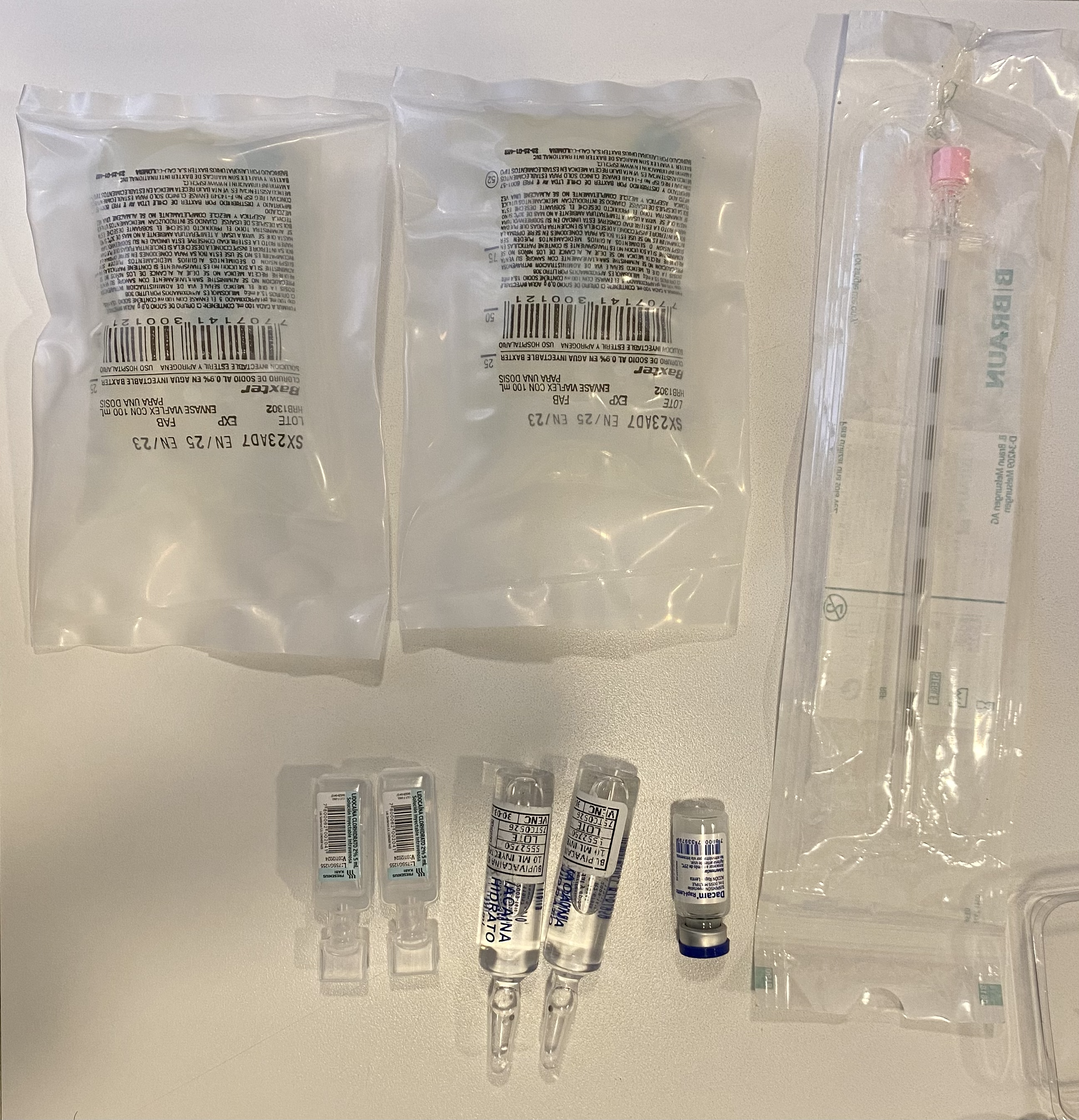
Source: Photograph taken by the authors.
Different infiltration sites after recognition of the painful points.
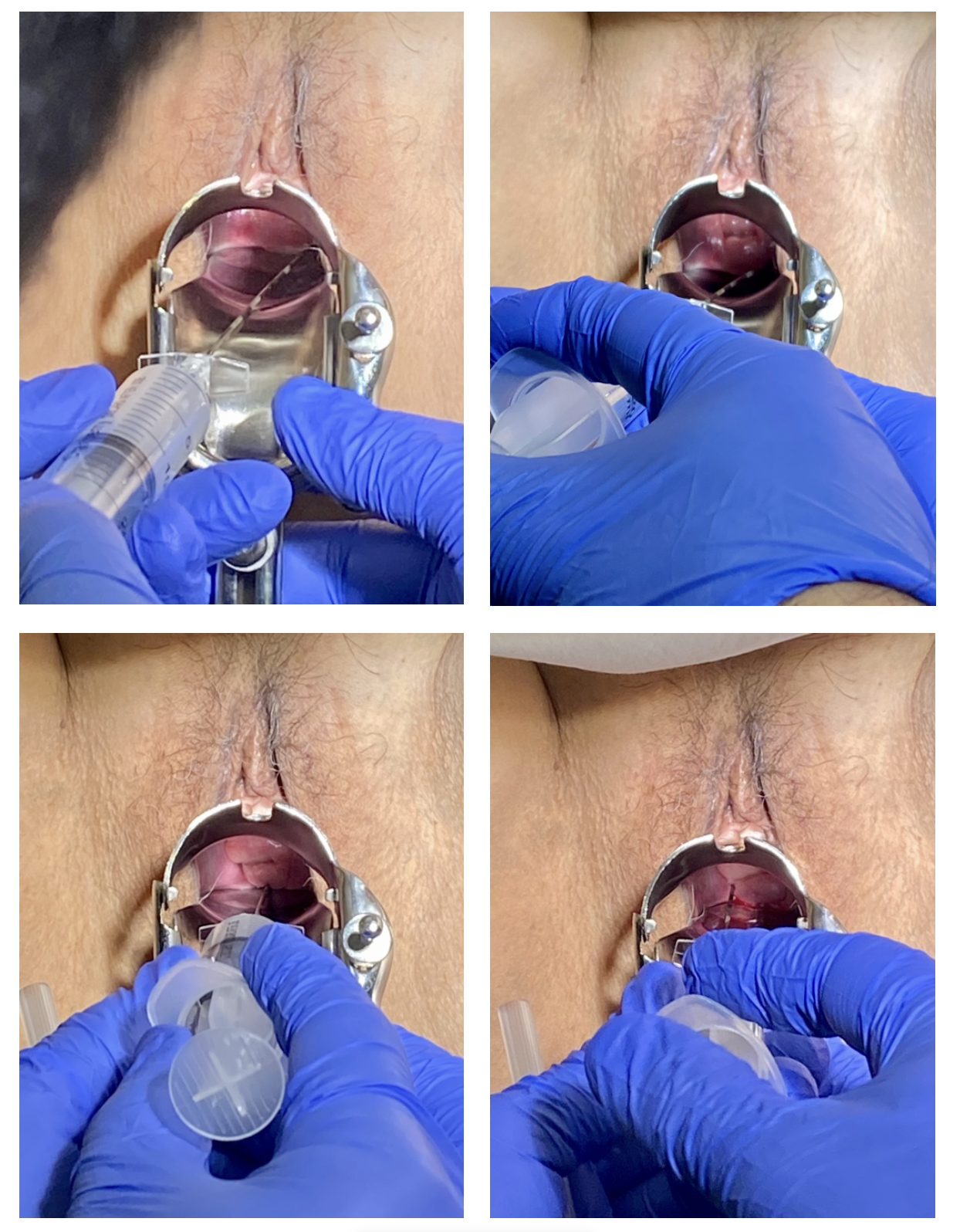
Source: Photograph taken by the authors.
The patient tolerated the procedure well. Minutes later, she manifested remission of symptoms, using a visual analog scale of 1/10. No complications were reported with this procedure. During the following two weeks, the visual analog scale score remained at 1/10, accompanied by an improvement in anal symptoms. After six months of follow-up, the patient maintained the same visual analog scale score of 1/10, reporting no gluteal or anal pain. The timeline is described in Table 2.
Discussion
Female genital prolapse significantly impacts patients' quality of life. Fixation of the vaginal apex or cervix to the sacrospinous ligament for the correction of apical prolapse, proposed by Richter in 1968, is a widely employed technique due to its efficacy, shorter surgical duration, faster recovery, and simplicity, especially in patients who are obese or medically contraindicated for laparotomy [6]. The sacrospinous ligament is a robust, supportive pelvic structure that extends from the sciatic spine to the sacral wall. It is closely associated with the pudendal neurovascular bundle and the inferior gluteal vessels, especially in its anterior portion.
The surgical procedure begins with a crescent-shaped incision in the posterior vaginal wall. This opens the pararectal space and allows access to the posterior pelvic cavity. The sacrospinous ligament is then located, identifying its insertion in the ischial spine and its course towards the S4 and S5 portions of the sacrum. The ligament is located medial to the obturator internus muscle and above the rectus. Once the ligament is identified, dissection of the surrounding soft tissues is performed to adequately expose it. Non-absorbable sutures are placed through the ligament, about two centimeters medial to the ischial spine, anchoring them to the vaginal apex. This allows the vaginal fornices to be suspended in the sacrospinous ligament. Subsequently, the sutures are tied and vaginal closure of the incision is performed [7,8,9,10,11].
It is crucial to take into account specific anatomical considerations during surgery, especially the relationship of the sacrospinous ligament to the pudendal nerve. The pudendal nerve exits the pelvis through the greater sciatic foramen, passes over the sacrospinous ligament, curves forward, and re-enters the pelvis through the lesser sciatic foramen, distributing into several branches that innervate the muscles and skin of the perineum. The area of greatest risk for pudendal nerve injury occurs during deep dissection to expose the sacrospinous ligament. If excessive dissection is performed or sutures are inappropriately installed in the area, the pudendal nerve can be damaged. The nerve’s proximity to the sacrospinous ligament places it in a vulnerable position during surgery. For this reason, careful planning and execution are required to avoid complications.
While this procedure is generally safe, neuropathic pain in the gluteus and posterior thigh has been observed, with an incidence of up to 15% postoperatively [5], as described in the case presented. Gluteal pain may result from nerve root injury (S3 to S5) within the sacrospinal ligament complex, where the suture is placed during vaginal apex fixation [12].
Pudendal neuropathy following sacrospinous hysteropexy is a rare but clinically significant complication. Classic symptoms include radiating pelvic, gluteal, and anal pain, with a strong indication of neuropathic injury in cases of persistence and specific location.
The first line of management for neuropathic pain after sacrospinous hysteropexy is medical management. Neuromodulatory drugs such as pregabalin and gabapentin are frequently used [1]. Pregabalin affects calcium channels in neurons, decreasing the release of excitatory neurotransmitters such as glutamate, which helps to reduce pain perception.
There is also evidence for the use of drugs such as amitriptyline, which acts on descending pain pathways [2].
In cases where patients do not respond to conventional medical management, infiltrations with corticosteroids and local anesthetics are considered, as was done in this case, in which a combination of betamethasone, lidocaine, and bupivacaine was used. Corticosteroids reduce local inflammation, while anesthetics temporarily decrease pain by blocking sodium channels in painful nerve fibers [3].
This case report highlights the efficacy of localized infiltration with steroids and anesthetics as a management strategy in patients refractory to conservative treatment. The permanent improvement of pain at six months highlights the effectiveness of this combined approach and the importance of early diagnosis to avoid chronic pain. Although there are reports of corticosteroid infiltration in suspected pudendal neuralgia, they are often with short-term follow-up and do not occur as a consequence of a surgical procedure. This is why this clinical case provides valuable information to the clinician who performs this type of intervention [13,14].
It is essential to consider the differential diagnoses of post-hysteropexy pain. Examples of these diagnoses are muscle or tendon injuries [4]; pudendal nerve entrapment syndrome, which can be suspected when the pain increases in the patient when sitting and is relieved when standing or lying down [5]; and myofascial pain, infection, or postoperative hematoma. The latter, although rare complications are causes of postoperative pain that should be ruled out by clinical examination and imaging to confirm or rule out suspicion [7].
In cases of persistent gluteal pain beyond six weeks, the primary recommendation is reintervention and suture removal at the level of the ligament, if feasible [15]. However, the Anchosure® kit complicates removal from the sacrospinous ligament, often making it inaccessible.
Posterior tibial nerve neuromodulation (Per-cutaneous Tibial Nerve Stimulation, or PTNS) is a therapeutic possibility. This technique is used in different types of pain related to the nervous system. It is based on the electrical stimulation of the posterior tibial nerve through an electrode near the ankle. A stimulation is produced that sends signals to the central nervous system, modulating neural activity and reducing pain perception. This technique is effective in certain types of pain, especially in pelvic pain and in cases of chronic neuropathic pain, as well as in overactive bladder. The simulations are usually applied in 12 sessions of about 30 minutes each, with the possibility of extending the treatment according to the response. The technique is minimally invasive and generally well tolerated. However, its effectiveness and safety may vary depending on the individual [16,17,18,19,20,21].
There is limited and scant evidence for outpatient management of neuropathic pain using pain point infiltration and pudendal nerve block [6]. There is also no evidence of this procedure’s success rate over time. In this case report, infiltration emerged as an alternative after medication and physiotherapy failed, achieving a significant 95% reduction in pain. The rapid improvement in the visual analog scale and the sustained reduction of pain at follow-up suggest its potential benefit in cases of postoperative neuropathic pain, which has not been present in previous studies. For this reason, further research and long-term data collection are essential to fully support the efficacy of this strategy in cases of postoperative neuropathic pain associated with sacrospinous fixation.
Conclusions
Local infiltration with anesthetics and corticosteroids in painful sites after sacrospinous fixation proves to be a safe and effective alternative for managing postoperative pain of neuropathic origin. However, studies with longer follow-ups are needed to make recommendations in this regard.

