Reporte de caso
← vista completaPublicado el 6 de diciembre de 2024 | http://doi.org/10.5867/medwave.2024.11.2975
Presentación tomográfica con aspecto miliar en paciente inmunocomprometido con candidiasis pulmonar: reporte de caso
Tomographic presentation with miliary appearance in an immunocompromised patient with pulmonary candidiasis: A case report
Abstract
Introduction Candida albicans infection shows a wide range of patterns on chest computed tomography, including ground glass opacities and consolidation, with the miliary pattern being the least frequent. The miliary pattern is not exclusive to tuberculosis. Fungal lung infections are rare and potentially fatal. Colonization by Candida albicans, associated with impaired immunity, requires early empirical antifungal therapy to improve survival.
Case report 48-year-old male patient with persistent productive cough, mucopurulent expectoration, dyspnea on moderate exertion, night sweats, elevated temperature, and weight loss. Chest tomography revealed miliary interstitial lung disease, and he was prescribed antituberculosis treatment. The pathologic result of the biopsy concluded the presence of moderately differentiated keratinized infiltrating squamous cell carcinoma. The patient died.
Dicussion The miliary tomographic pattern requires a broader approach for accurate diagnosis. The reported case presented with oral candidiasis and impaired immunity. Previous colonization associated with impaired immunity is the most important factor found for disseminated candidiasis.
Conclusion The miliary radiological pattern is not exclusive to tuberculosis, warranting a more precise diagnostic approach. It is important to diagnose disseminated candidiasis in order to initiate early antifungal therapy and thus improve survival.
Main messages
- The miliary tomographic pattern has diverse differential diagnoses and specific cultures; histological studies are necessary to determine its etiology.
- Pulmonary fungal infections are infrequent, potentially lethal, with high morbimortality.
- This work presents a rare case of pulmonary candidiasis from the tomographic point of view to be considered among the differential diagnoses in immunocompromised patients. Diagnostic video bronchoscopy showed two tumors in the right main bronchus. Studies of the samples revealed the presence of Candida albicans in the pulmonary parenchyma. A new contrasted chest tomographic study reported a heterogeneous lesion in the esophagus. The pathologic result of the biopsy concluded the presence of moderately differentiated keratinized infiltrating squamous cell carcinoma. The patient died.
Introduction
Pulmonary fungal infections are infrequent and potentially lethal, with high morbidity and mortality rates [1]. Updated estimates suggest an annual incidence of 6.5 million invasive fungal infections and 3.8 million deaths, of which about 2.5 million (68%; range 35 to 90) were directly attributable. About 1 565 000 people have a Candida albicans bloodstream infection or invasive candidiasis each year, with 995 000 deaths (63.6%) [2].
Most patients with pulmonary candidiasis often have generalized systemic involvement, and invasive candidiasis (candidemia) occurs more frequently in patients with some factor of immune impairment [3,4]. Chest computed tomography findings are nonspecific. A high index of suspicion based on clinical data can guide the diagnosis of pulmonary Candida albicans infection. Miliary nodule images are the least frequent forms [3,5,6]. This pattern is representative of a lymphohematogenous dissemination of the disease [7]. For accurate diagnosis, bronchoscopy with bronchoalveolar lavage, plus transbronchial biopsy with histological studies with hematoxylin-eosin staining and Schiff’s periodic acid-Schiff technique should be performed [8].
Case report
A 48-year-old male patient from Otuzco, La Libertad, Peru. He was a farmer and had a history of exposure to wood smoke since childhood and chronic alcoholism. He denied close contact with people with tuberculosis and co-morbidities. He attended the emergency department of the Hospital Regional Docente de Trujillo on May 8th, 2023, with a period of illness of approximately six months. He had a cough with mucopurulent expectoration, solid foods dysphagia, hypoxia, and weight loss of approximately 13 kilograms (22%). In addition, he reported feeling general malaise, night sweats, and unquantified thermal rises. Seven days before admission, nausea, vomiting, oral intolerance, and increased dyspnea on slight exertion were added.
He was admitted to the emergency department with the following vital signs:
-
Oxygen saturation (pulse oximetry): 84%.
-
Inspired oxygen fraction: 21%.
-
Arterial pressure: 80/60 millimeters of mercury.
-
Heart rate: 130 per minute.
-
Respiratory rate: 20 per minute.
Oxygen support, intravenous hydration, and vasopressors were indicated.
The patient appeared to be in poor general condition, with poor hydration and nutrition. Physical examination revealed skin pallor +/+++ and a capillary refill of three seconds. Oral mucosa was dry, and the tongue had whitish plaques suggestive of oral candidiasis. Chest auscultation showed decreased vesicular murmur and crackles in both bases.
Cardiovascular examination reported tachycardic heart sounds of low intensity, without murmurs. Peripheral pulses were symmetrical with tachysysphygmia. The abdomen was soft and depressible, with pain on deep palpation in the mesogastrium and present hydro-aerial sounds. The nervous system was oriented in terms of time, space, and person. There were no motor or sensory deficits or meningeal signs (Glasgow scale 15).
Initial blood tests showed leukocytosis without left deviation with relative lymphopenia (21 860 per cubic millimeter, 2% basophils, 91% segmented, 5% lymphocytes); increased C-reactive protein (89.1 milligrams per liter), serum creatinine at the upper limit of the normal range (1.3 milligrams per deciliter), increased serum urea level (117 milligrams per deciliter). Two sputum smears were reported as negative and with good-quality samples. Postero-anterior chest radiograph reported diffuse micronodular images in the lower two-thirds of both lung fields. The electrocardiogram reported sinus tachycardia.
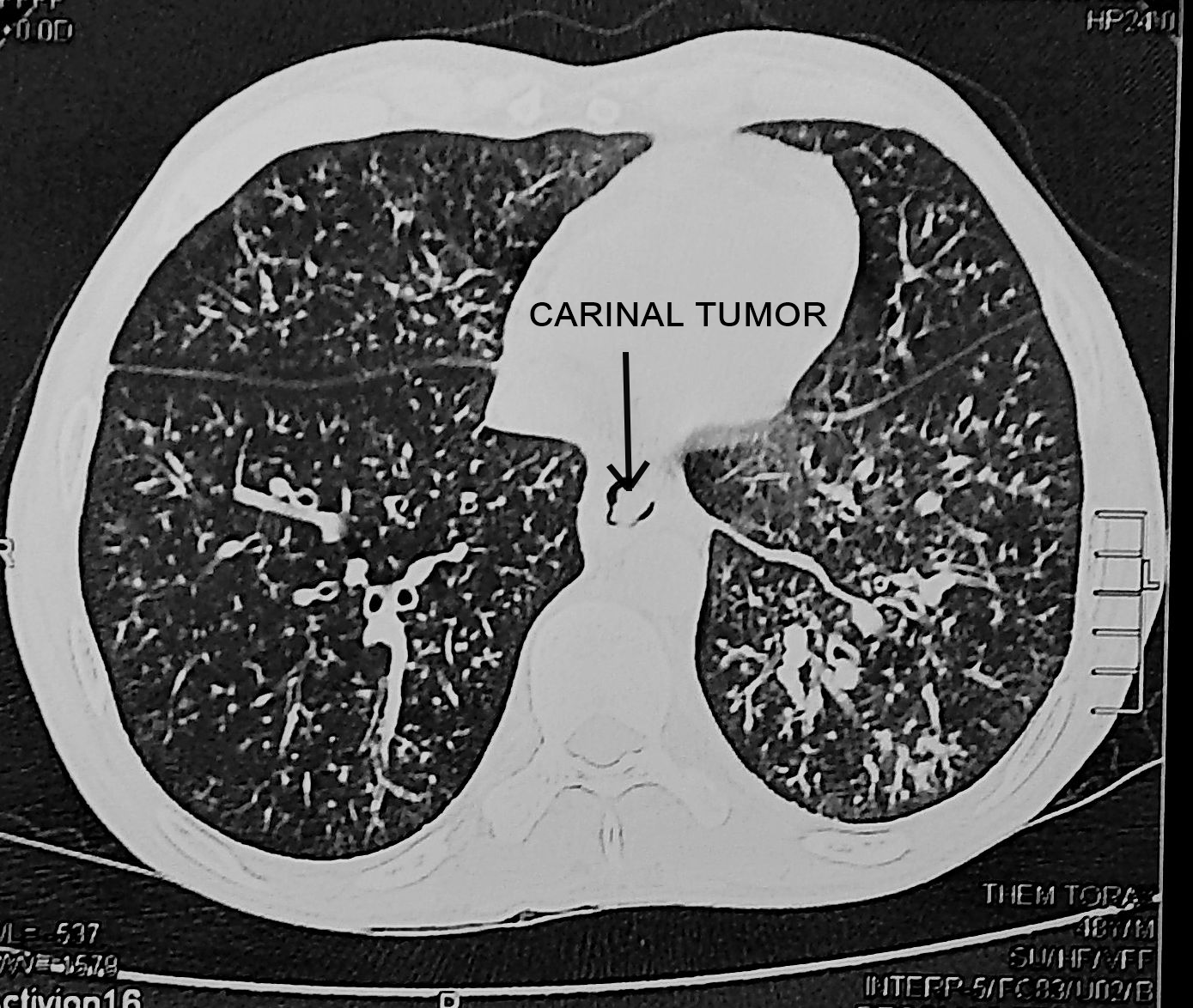
During the two-day stay in the emergency department, a non-contrast computed axial tomography of the chest was also requested. This showed the presence of “tree in bud” images, compatible with nonspecific “miliary” pulmonary interstitiopathy in both lung fields, in addition to esophageal dilatation suggestive of achalasia (Figures 1 and 2).
Chest computed axial tomography: revealing “tree-in-bud” images compatible with non-specific milia-type pulmonary interstitiopathy in both lung fields (coronal slice).
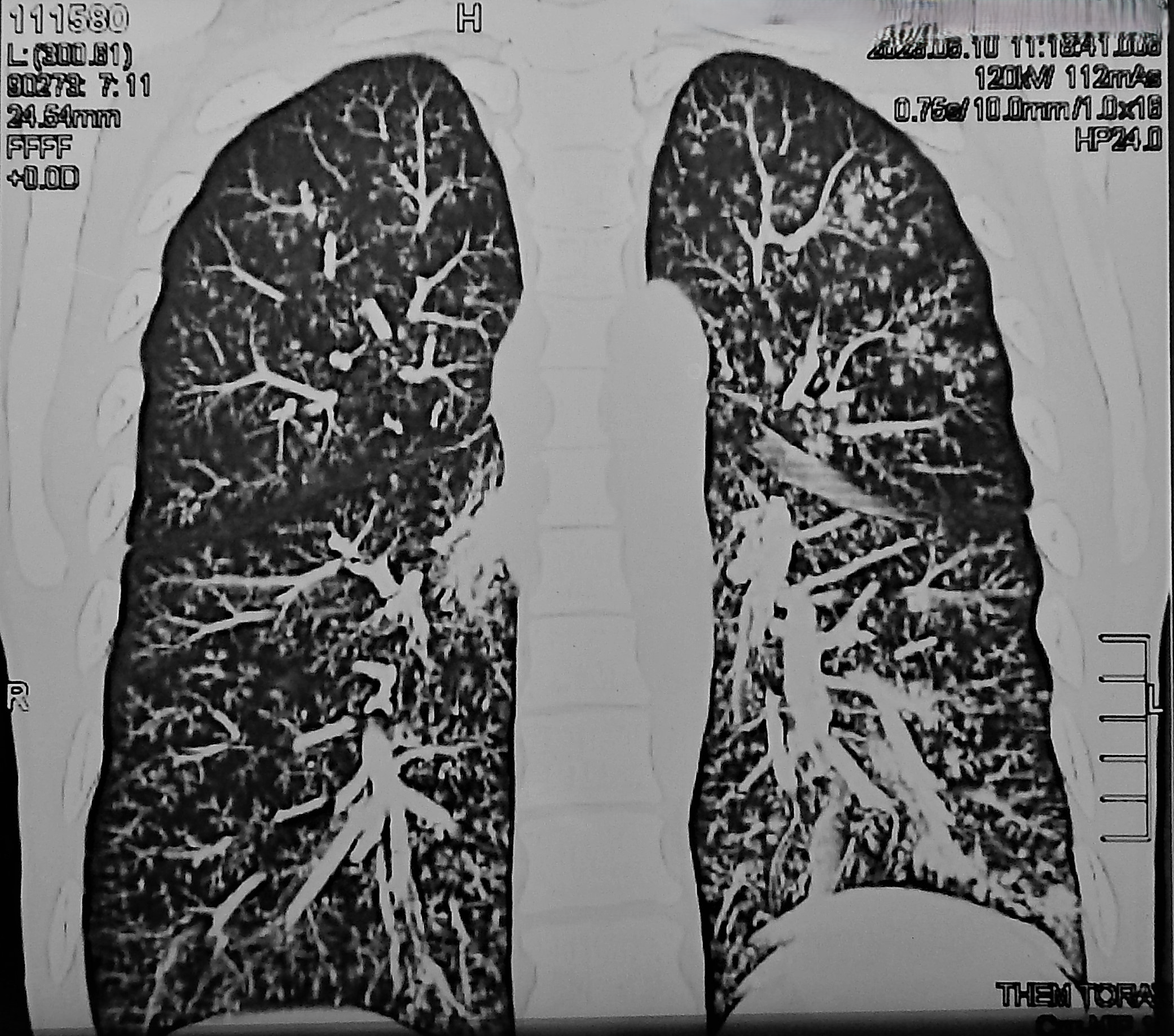
Chest computed axial tomography: revealing “tree-in-bud” images compatible with nonspecific “milia” type pulmonary interstitiopathy in both lung fields (axial slice).
Due to the clinical situation and epidemiological criteria, the medical team of the emergency department proposed miliary tuberculosis plus chronic alcoholism as a diagnostic hypothesis. For this reason, they decided to initiate treatment for miliary tuberculosis with isoniazid (H), rifampicin (R), ethambutol (E), and pyrazinamide (Z) in the presentation of combined fixed doses, adjusted to body weight, in addition to prednisone at a dose of 40 milligrams per day.
The patient was hospitalized in the pneumology department. On May 15th, he underwent abdominal and chest ultrasound. The study revealed the presence of residual hepatic calcification of 3 millimeters in the right lobe, in addition to right pleural effusion (428 milliliters) and left pleural effusion (290 milliliters), with signs of consolidation and bilateral passive atelectasis. A new serum total protein and serum albumin dosage showed severe hypoalbuminemia (2.2 grams per deciliter).
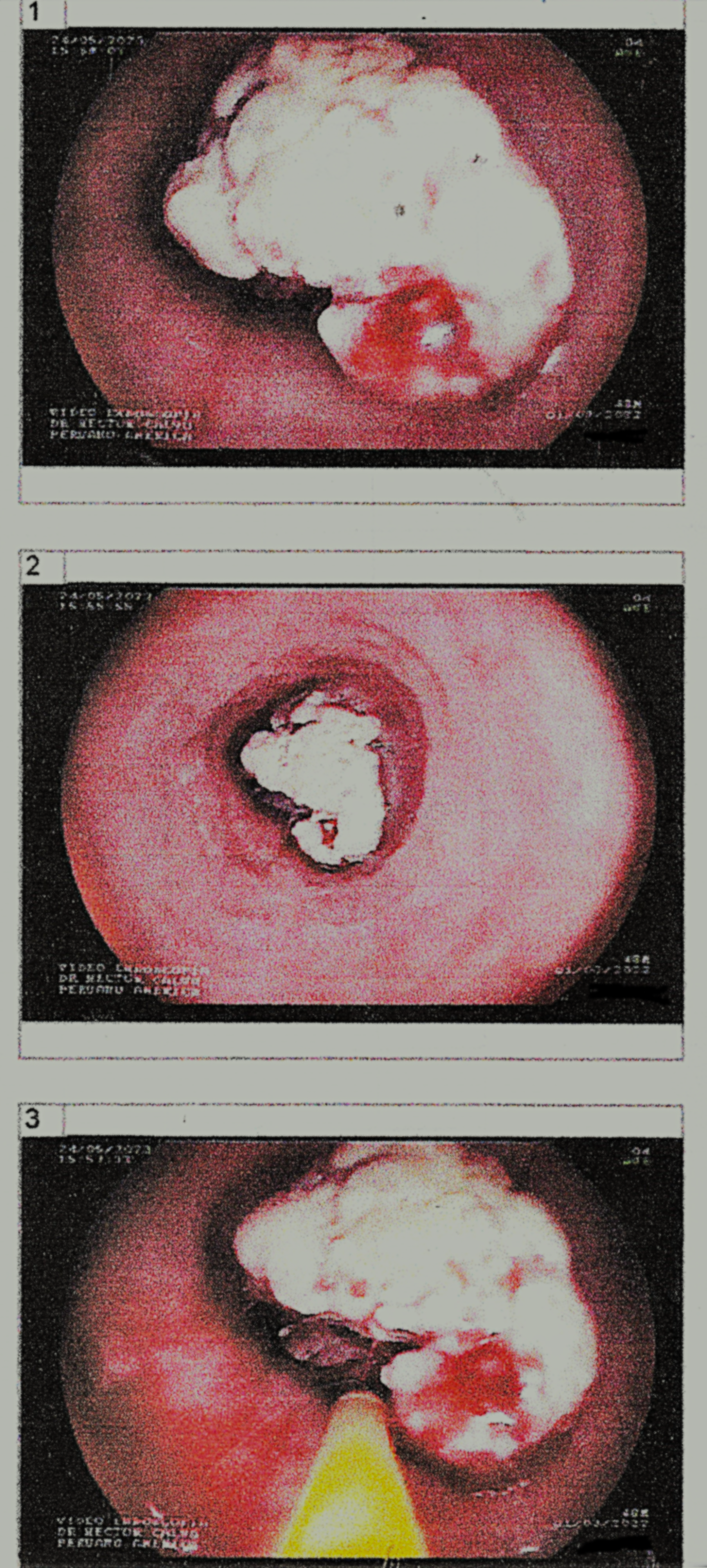
The following day, a diagnostic bronchoscopy video was performed. The findings in the right bronchial branch showed abundant mucopurulent secretion. In addition, in the main bronchus, there was an irregular surface tumor with vascularized areas that partially involved the main carina. Adjacent to it was a prominent, rounded, exophytic lesion with signs suggestive of necrosis. Both lesions were biopsied. The samples were sent for bacteriological and anatomopathological studies. Only purulent secretion was evidenced in the exploration of the left bronchial branch. The secretions were aspirated, and the samples were sent for bacteriological study of acid-fast bacilli, common germs, and fungi.
Intravenous antibiotic treatment was indicated (ceftriaxone 2 grams every 24 hours, clindamycin 600 milligrams every 8 hours) for 14 days, and oral azithromycin 500 milligrams every 24 hours for five days.
On May 20th, the tuberculin test (purified protein derivative) was applied to the forearm, and at 72 hours, the reading was 0 millimeters.
Ophthalmology evaluation was requested for fundus study due to suspected disseminated tuberculosis with non-contributory results.
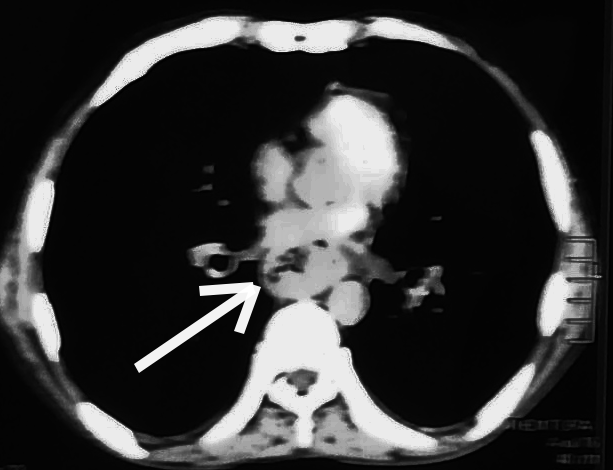
On May 22nd, a contrast-enhanced chest CT scan reported the presence of a heterogeneous lesion in the mediastinum behind the trachea at the level of the esophagus (Figures 3 and 4).
Computed axial tomography (mediastinal view) reveals a heterogeneous lesion in the mediastinum behind the trachea at the level of the esophagus (coronal section).

Computed axial tomography (mediastinal view) reveals a heterogeneous lesion in the mediastinum behind the trachea at the esophagus level (axial section).
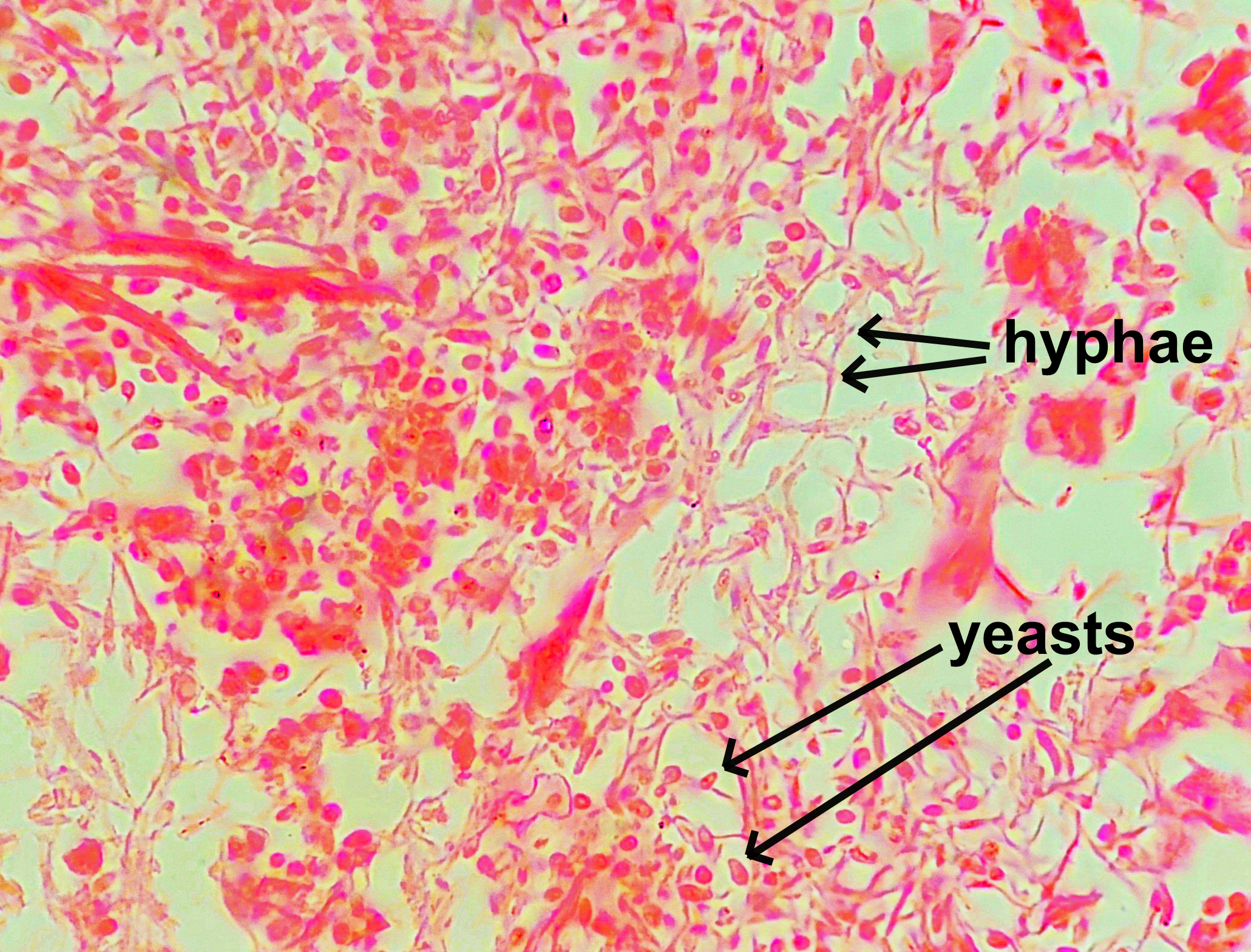
The results of the bronchoscopy samples reported that there was no presence of neoplastic cells in the bronchial aspirate cell block technique. In addition, Candida albicans were observed in the bronchial aspirate secretion (97% probability). The cytological and histological study of the bronchial biopsy reported respiratory epithelium with inflammatory infiltrate and fungal foci compatible with Candida albicans (Figures 5 and 6). On May 24th, antituberculosis treatment was suspended, and fluconazole 800 milligrams with loading dose and 400 milligrams every 24 hours by nasogastric tube was indicated (18 days after hospital admission).
Histology result of bronchial biopsy sample (hematoxylin-eosin stain) reveals the presence of pulmonary epithelium and Candida albicans hyphae.
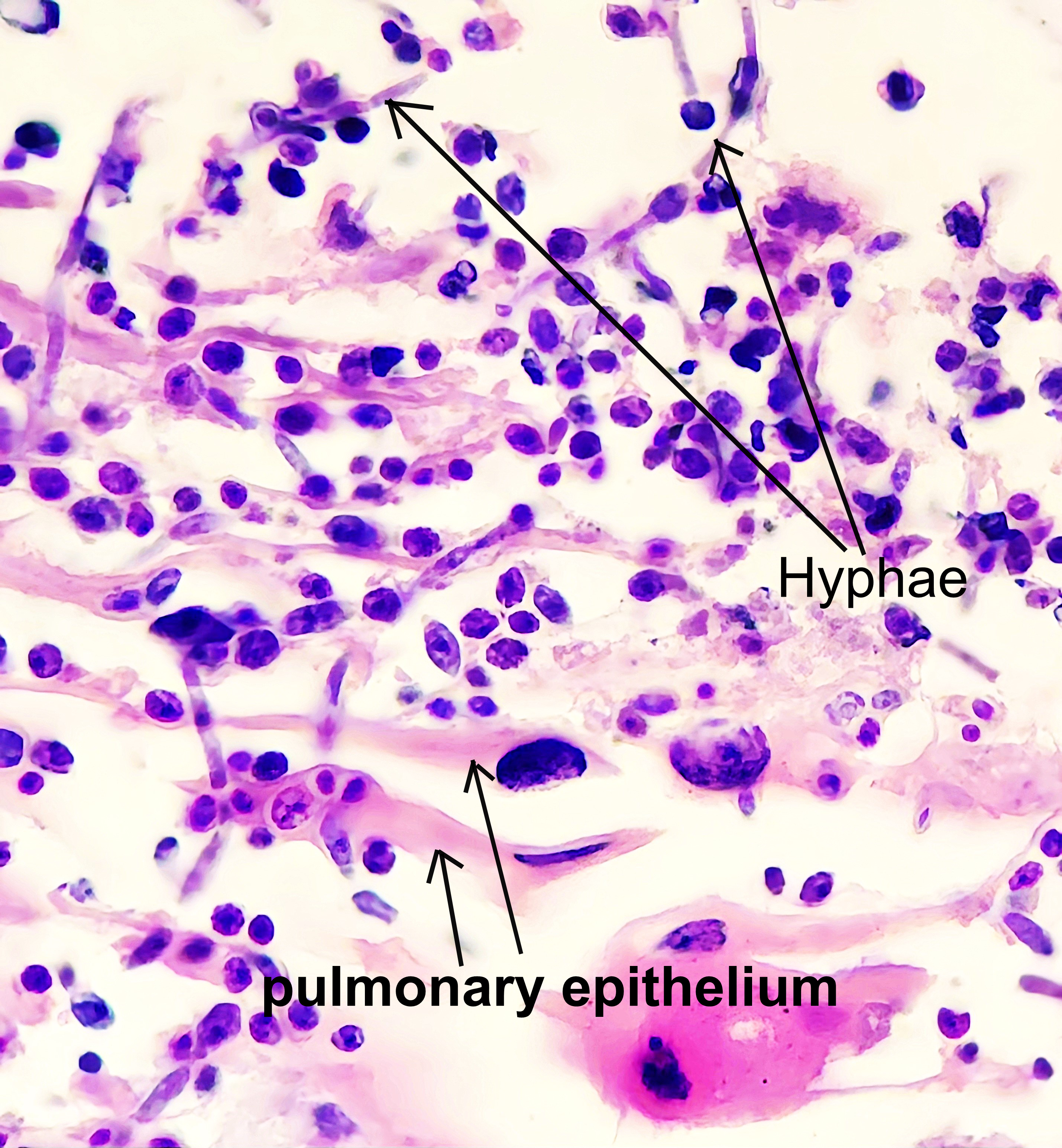
Cytology result of bronchial biopsy sample (hematoxylin-eosin stain) shows Candida albicans hyphae and yeasts.
On May 29th, an evaluation by gastroenterology was requested to perform an upper endoscopy study of the gastrointestinal tract. This showed an irregular proliferative lesion 22 centimeters from the dental arch, which produced stenosis of the esophageal lumen and prevented the probe from advancing (Figure 7). A gastrostomy was performed for enteral nutrition, and he remained clinically stable for the following 72 hours.
Endoscopy of the esophagus. Irregular proliferative lesion, partially covered with fibrin-producing stenosis of the esophageal lumen.
On June 2, a histopathological report of a biopsy of the esophageal tumor was received. It reported keratinized infiltrating squamous cell carcinoma and intermediate differentiation. That same day, the patient presented respiratory exacerbation and hemodynamic instability. The use of vasopressors through a central catheter was indicated without response. The patient passed away.
Table 1 shows the results of the ancillary tests performed.
Discussion
When a miliary pattern is observed in a tomographic study, the initial approach is correctly classifying its location regarding the secondary lung lobe and correlating its incidence with widely described pathologies. For example, random presentation often represents the hematogenous spread of disease, including tuberculosis, disseminated fungal infections, and metastases from neoplasms that have a preference for the lower and posterior zones of the lung [9,10], as is the case in the present report.
Miliary tuberculosis is a severe and disseminated form of tuberculosis. It occurs when the bacterium spreads through the bloodstream and affects multiple organs throughout the body. The term “miliary” is derived from the Latin word miliarius, which means resembling millet seeds. It describes the characteristic appearance of small tuberculous lesions in the affected organs. Regardless of the causative infectious agent, this finding indicates significant systemic involvement that warrants prompt therapeutic management [11].
Due to the poor general condition and severe respiratory compromise associated with the miliary pattern in the chest radiological studies, in addition to negative sputum smears and residing in a region with a high prevalence of tuberculosis [12], the medical team in the emergency department proposed the diagnosis of miliary tuberculosis. For these reasons, they immediately initiated antituberculosis treatment plus oral corticosteroids, which coincides with the recommended therapeutic approach for these cases [11].
As part of the study of miliary tuberculosis, smear microscopy of stool and urine samples was requested, and no evidence of alcohol-resistant bacilli was found. An eye fundus examination was also performed, showing no lesions compatible with tuberculous involvement. The macular lesion described was not attributed to tuberculous pathology.
The miliary pattern has several differential diagnoses. It is highly suggestive but not exclusive to infectious etiology, such as tuberculosis or histoplasmosis. Miliary images in radiological studies may be present in sarcoidosis, pneumoconiosis, secondary lung metastasis of primary thyroid, kidney, and trophoblast cancers, as well as sarcoma [13,14]. In this context, we expanded the studies using diagnostic video bronchoscopy and obtained bacteriological, cytological, and histological samples. These resulted in the presence of Candida albicans in the pulmonary parenchyma.
Candida albicans, a saprophytic fungi, causes infection and disease when previous colonization and factors associated with impaired immunity exist. After invading the mucosa, Candida albicans proliferates, adheres, develops plaques, and subsequently spreads through the vascular system, causing candidemia [15,16]. Candidemia causes decreased T-cell response and can infect any organ, leading to invasive candidiasis [17]. About 80% of Candida albicans infections are associated with biofilm development, favoring systemic invasion and greater inflammatory response and resistance to antifungals [16,17,18]. Infections by saprophytic fungi such as Candida albicans present a wide spectrum of patterns on chest computed tomography. These mainly include ground-glass opacities, consolidation, cysts, and cavitations. They rarely present nodule or micro-nodular patterns (miliary pattern) [19,20].
The fine nodular pattern seen in the tomographic study would represent candidemia due to the bronchogenic spread of Candida albicans from a primary pulmonary source. This may also happen in patients with gastrointestinal or genitourinary candidiasis, which is present before hematogenous spread to the lungs. Therefore, early detection of Candida albicans in non-pulmonary sites is recommended for early antifungal therapy [21].
As part of the comprehensive evaluation, due to solids dysphagia, the patient was referred to the gastroenterology department for evaluation and endoscopic study of the upper gastrointestinal tract. The endoscopic inspection revealed the presence of a tumor mass in the esophagus in its middle thoracic portion. On the other hand, the anatomopathological study of the respective biopsy showed a moderately differentiated keratinized infiltrating squamous cell carcinoma. This would explain the patient’s severe immunosuppressed state.
Esophageal cancer originates in the esophageal mucosa and spreads into the muscular and adventitial layers. Depending on the type of cell where it originates, epidermoid carcinoma starts in squamous cells. Generally, it is located in the middle and upper part, unlike adenocarcinoma, which involves glandular cells and is located in the lower part of the esophagogastric junction. Both forms are very aggressive, making esophageal neoplasia one with the lowest survival. If diagnosed in an advanced stage, survival rates are between five and seven months [22]. In the present case, with a disease time of six months, the esophageal cancer was in advanced stage. It was a late diagnosis. Among the risk factors associated with the development of esophageal squamous cell carcinoma are alcohol consumption, low social status, and achalasia, among others [23]. These factors coincide with those reported by the patient and described in this report.
The case of our patient had oral cavity plaques compatible with oral candidiasis, in addition to risk factors for impaired immunity, such as malnutrition, chronic alcoholism, lymphopenia, and esophageal carcinoma.
The most important factors found for disseminated candidiasis are previous colonization and impaired immunity. These factors are determinants for initiating early empirical antifungal therapy to improve survival in these patients [24,25,26].
Conclusions
The miliary-type radiological pattern is highly suggestive but not exclusive of tuberculosis, warranting a more precise diagnostic approach.
Candida albicans is a saprophytic fungus that causes disease when there is previous colonization and impaired immunity.
Candida albicans infection has a wide spectrum of chest computed axial tomography patterns, the miliary pattern being the least frequent.
The diagnosis of esophageal carcinoma was made at an advanced stage; therefore, it had a grim prognosis.
According to this case report, it is important to diagnose disseminated candidiasis to initiate early antifungal therapy and thus improve survival in immunocompromised patients.

