Nota técnica
← vista completaPublicado el 20 de diciembre de 2016 | http://doi.org/10.5867/medwave.2016.11.6805
Carcinoma de células basales pigmentado simulando un melanoma de extensión superficial
Pigmented basal cell carcinoma mimicking a superficial spreading melanoma
Abstract
Basal cell carcinoma is the most common form of skin cancer, especially in elderly people. Pigmented basal cell carcinoma is a rare subtype and has been described in the literature as a nodular and hyperpigmented lesion; rarely, it can appear as an extensive pigmented plate, which may be clinically indistinguishable from superficial spreading melanoma and Bowen disease. Dermatoscopy has a high sensitivity in the diagnosis of basal cell carcinoma. When Menzies criteria are used; however, the final diagnosis is made by histopathology. The objective of the present report is to analyze the case of a patient with pigmented basal cell carcinoma simulating a superficial spreading melanoma.
Introduction
Basal cell carcinoma is the most frequent of skin cancers. This carcinoma usually appears on skin areas that are most frequently affected by sun exposure, specially on those individuals with skin types I and II, and on elderly population. However, it should be noted that in the last few years there has been a surprisingly rising rate of new cases, specially on people under 50 years of age [1]. Its clinical presentation is mainly characterized by slow growth and low metastatic potential. Nonetheless, without proper treatment it may result in poor outcome, generally driven by its local invasion.
There are five different types of basal cell carcinoma described in the literature:
- Nodular.
- Superficial.
- Pigmented.
- Morpheaform.
- Pinkus fibroepithelioma.
The pigmented form is an infrequent subtype of basal cell carcinoma that shows melanin pigments in its histopathology and is generally described in common literature as a nodular hyperpigmented translucent lesion [1],[2]. The pigmented basal cell carcinoma can also appear as a rare clinical presentation showing the shape of a broad superficial plaque, appearing in few cases report in literature [3].
Given its low frequency, we will now present one of these clinical cases, and briefly analyze its main differential diagnoses, including malignant melanoma of superficial extension considering its importance for prognosis.
Clinical case
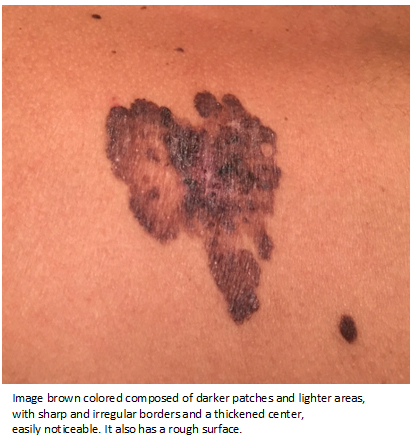
A 51 year-old woman, previously healthy, consulted to a physician for the newly appearance of a skin lesion on her back, with a progressively fast growth, associated with occasional pruritus, but unable to determine its exact progression time. On physical examination, there was a brown colored plaque at the lower lumbar zone, with 7 to 5 cm diameter, sharply and irregular borders, and a hard consistence when touched through standard palpation procedure (Figure 1).
 Full size
Full size A contact dermatoscopic image of moderate quality showed a heterogeneous lesion with an asymmetric pattern and several different structures, which resembled a melanocytic lesion (Figure 2).
 Full size
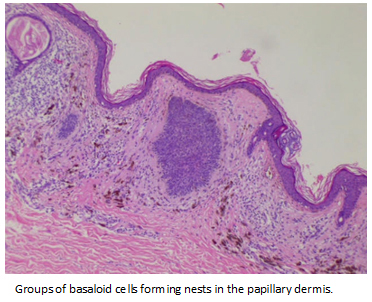
Full size The incisional biopsy showed a group of basaloid cells forming nests, with a peripheral palisade on the papillary dermis, and the presence of melanin (Figure 3). After removing the whole lesion, histopathology revealed the same results described previously. Additional zoom revealed the presence of melanin and melanophages through the dermis (Figure 4). The patient showed complete recovery, at least during the first year follow up.
 Full size
Full size 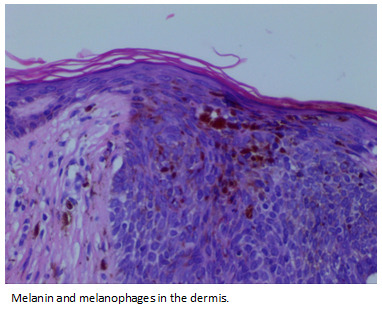 Full size
Full size Discussion
Clinically, pigmented basal cell carcinoma as an extensive irregular plaque is to be differentiated from a superficial spreading melanoma, which is usually a palpable plaque with irregular borders, generally containing more than one color tone, and sometimes with areas of tumor regression. Another differential diagnosis to consider is pigmented Bowen’s disease mainly due to the well-delimited edges of the lesion [4].
Dermatoscopy is a noninvasive diagnostic technique, which uses optical magnification for the visualization of certain skin areas, which cannot be seen at naked eye [5]. Its main use is found in the differential diagnosis of pigmented skin lesions. Dermatoscopy is useful as a complementary tool when its polarized light and contact functions are combined, in order to see a greater spectrum of structures as possible. In our case, where only contact dermatoscopy was used, probably we could not identify all the possible structures needed to determine the type of lesion we were studying, making its use questionable in this context. Nonetheless, today dermatoscopy is considered a clue tool in the diagnosis of basal cell carcinoma, because it allows an early detection and diagnosis, and contributes to the differential diagnosis with other skin tumors, both pigmented and non-pigmented [6].
Basal cell carcinoma’s dermatoscopic diagnosis based on Menzies et al criteria [7], requires the absence of pigmented reticulum and the presence of at least one of the following criteria:
- Ulcerations.
- Big blue-grey ovoid nests.
- Leaf-like areas.
- Spoke-wheel areas.
- Arborizing vessels.
- Multiple blue-grey globules and dots.
It has been determined that around 96.5% of basal cell carcinomas show at least one of these criteria, so this method is a very useful diagnostic tool [6].
There are other structures that may be present in pigmented basal cell carcinoma, such as brown globules/dots or blue whitish veil and irregular blood vessels. The frequency of this findings increases with the lesions degree of pigmentation, acquiring morphological resemblance with the melanoma when the concentration of pigments is greater [6]. However, Menzies criteria allow recognizing a basal cell carcinoma even in the presence of great intensity of pigment [6]. According to the author, the first criterion may not be present in the pigmented basal cell carcinoma (absence of pigmented reticulum), but one of the six criteria proposed must be present. This method would have a 97% sensitivity in the diagnosis of pigmented basal cell carcinoma [7].
In our case, although the technique was not the most accurate, you can see an intensively pigmented lesion, with structures that may suggest melanoma, like the blue-grey veil, brown dots and hyperpigmented spots. There are also multiple blue-grey globules distributed all throughout the lesion. Considering the final diagnose, we corroborated the diagnostic power of Menzies criteria. In this case, the dermatoscopic key was the presence of blue-grey globules.
Regarding pigmented Bowen`s disease as a differential diagnosis, it should be noted this is a rare disease, prevailing in black skin type men, aged between 60 and 70 years. It is clinically characterized by a very well demarcated pigmented plaque, just as in our case, but unlike basal cell carcinoma, Bowen´s pigmented disease has been reported in areas of the skin with no sun exposure. [8].
The dermatoscopic findings on Bowen`s disease are not characteristic; one usually finds a disorganized pattern, without structure, of a brownish color. You may identify less structured and hypopigmented areas, grey dots, areas of grey-brown pigment and blood vessels [9].
Even with Menzies criteria, the definite diagnosis is given by the biopsy. In the histopathology, the pigmented basal cell carcinoma has common features with its nodular variant. It shows basal cells grouped on the papillary and reticular dermis, forming nests of different sizes with a palisade of basaloid cells on the periphery, surrounded by retraction spaces [10]. In the case of pigmented basal cell carcinoma, besides the mentioned findings there are melanin pigments and melanophages.
Asymmetric histopathologic features characterize superficial spreading melanoma, which shows great amounts of isolated melanocytes, badly circumscribed, with random distribution, and with the tendency to form discohesive nests. Additionally, melanocytes are present on the basal layer (pagetoid dissemination) [11].
Histopathology of pigmented Bowen`s disease shows hyperkeratosis, parakeratosis and epidermal dysplasia, with abundant cells rich in melanin, located in the basal layer. Additionally, it is possible to find an infiltrate of lymphocytes or histiocytes in the dermis [4].
Conclusion
In a patient with a broad pigmented plaque, with well-demarcated borders, the first differential diagnoses to think about should be a pigmented basal cell carcinoma, a superficial spreading melanoma and a pigmented Bowen’s disease. Clinically, these three diseases may be indistinguishable.
Dermatoscopy is a useful tool because it increases sensitivity for basal cell carcinoma diagnosis when one or more Menzies criteria are present. Nevertheless, the final diagnosis needs the histopathological study of the lesions.
Notes
From the editor
The author originally submitted this article in Spanish and English. The Journal has not copyedited the English version.
Ethical aspects
The patient has signed the informed consent form requested by Medwave. A copy was sent to the editorial board of the magazine.
Declaration of conflicts of interest
The authors have completed the ICMJE conflict declaration form translated into Spanish by Medwave, and declare that they have not received funding for the report; Not having financial relationships with organizations that might have interests in the published article in the past three years; And not having other relationships or activities that could influence the published article. Forms can be requested by contacting the responsible author or the editorial board of the Journal.
Financing
The authors state that there were no external sources of funding.

