Resúmenes Epistemonikos
← vista completaPublicado el 30 de septiembre de 2022 | http://doi.org/10.5867/medwave.2022.08.2568
Adición de melatonina a terapia con hipotermia para encefalopatía hipóxico-isquémica neonatal
Addition of melatonin to hypothermia therapy for neonatal hypoxic-ischemic encephalopathy
Abstract
Introduction Neonatal hypoxic-ischemic encephalopathy is caused by perinatal asphyxia, resulting in an acute neurological dysfunction of variable severity. It occurs in one to six of every 1000 full-term newborns and is associated with high neonatal morbimortality and adverse neurological outcomes. The use of hypothermia is considered the standard therapy for this condition. However, different adjuvant therapeutic options have been proposed due to limited clinical efficacy, including drugs like melatonin. There is controversy about whether combined therapy with melatonin is superior to monotherapy with hypothermia.
Methods We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, and Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of the findings table using the GRADE approach.
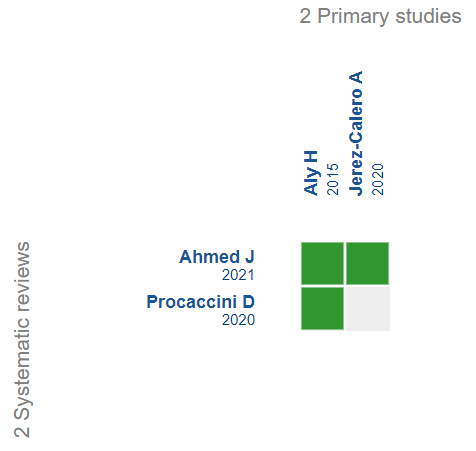
Results We identified two systematic reviews that included two primary studies, both randomized trials. The two randomized trials were included in the analysis of the present work.
Conclusion It is not possible to establish whether the addition of melatonin decreases mortality or the probability of alterations in brain magnetic resonance imaging because the certainty of the existing evidence has been assessed as very low. On the other hand, the addition of melatonin to hypothermia therapy, compared to hypothermia monotherapy, may increase the probability of normal neurological examination at six months and the probability of normal cognition at 18 months. Finally, adding melatonin to hypothermia therapy likely reduces the probability of seizures.
Main messages
- It is not possible to establish whether the addition of melatonin decreases mortality or the probability of presenting alterations reflected in brain magnetic resonance imaging because the certainty of the existing evidence has been evaluated as very low.
- Adding melatonin to hypothermia compared to hypothermia monotherapy may increase the likelihood of normal neurologic examination at six months and normal cognition at 18 months (low certainty of the evidence).
- Adding melatonin to hypothermia compared to hypothermia monotherapy may likely decrease the likelihood of seizures (moderate certainty of the evidence).
Problem
Hypoxic-ischemic neonatal encephalopathy is characterized by acute neurological dysfunction of variable severity caused by perinatal asphyxia [1]. In these episodes, hypoxia generates excitotoxicity and the accumulation of free radicals, nitric oxide, cytokines, and intracellular calcium, resulting in neural necrosis [2]. Clinically, it is possible to classify this pathology into three stages according to the modified Sarnat Classification to assess prognosis [3].
Hypoxic-ischemic neonatal encephalopathy incidence is estimated to be one to six per 1000 term newborns [4] and is associated with high neonatal mortality. Mortality rates are close to 10% in patients with moderate disease and up to 60% in cases of severe neonatal disease [5]. Moreover, about 30% of surviving patients with moderate and virtually all patients with severe neonatal hypoxic-ischemic encephalopathy have severe neurological sequelae, including cerebral palsy [5]
Currently, the standard therapy for neonatal hypoxic-ischemic encephalopathy is based on hypothermia treatment, consisting of the controlled reduction of body temperature by two to four degrees Celsius during the first six hours of life. Multiple studies have validated this therapy due to its neuroprotective capacity [6]. However, it has been shown that approximately half of the cases do not obtain significant clinical benefits from hypothermia as monotherapy [7].
In this context, new adjuvant treatments have been studied, highlighting the therapeutic potential of using melatonin – a neurohormone with antioxidant and anti-inflammatory properties – and its ability to cross the blood-brain barrier [8]. Other therapeutic options currently under study include erythropoietin, magnesium, allopurinol, and xenon [1].
Although the therapeutic addition of melatonin could decrease mortality and improve neurological outcomes [9], there is currently no consensus on whether hypothermia monotherapy or combination therapy with the addition of melatonin should be used [9-12]. For this reason, it is essential to provide a summary of the evidence that allows a comparison of both treatments.
Methods
We searched Epistemonikos, the largest database of systematic reviews in health, which is maintained by searching multiple information sources, including MEDLINE, EMBASE, and Cochrane, among others. We extracted and analyzed the data from the primary studies of the identified reviews and generated a structured summary called FRISBEE (Friendly Summaries of Body of Evidence using Epistemonikos). We followed a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), a meta-analysis of all studies when possible, a summary table of results with the GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) method, and a section of other considerations for decision-making.
About the body of evidence for this question
|
What is the evidence? See the evidence matrix in Epistemonikos below. |
We found two systematic reviews [9-10], which included two primary studies [13],[14], both randomized trials. This table and the summary are based on both trials. |
|
What type of patients did the studies include? * |
One trial [13] included 30 term infants diagnosed with neonatal hypoxic-ischemic encephalopathy. The other study [14] included 25 preterm or term infants diagnosed with neonatal hypoxic-ischemic encephalopathy. Exclusion criteria were not reported in either trial [13],[14]. |
|
What type of interventions did the studies include? * |
Both trials [13],[14] compared melatonin and hypothermia therapy versus hypothermia monotherapy. The doses of melatonin used in one trial [13] were 10 milligrams per kilogram of body weight per day by orogastric tube, completing five doses in total. The doses of melatonin used in the other trial [14] were five milligrams per kilogram of body weight per day by the intravenous route, completing three doses in total. Both trials [13],[14] used manual hypothermia controlled with ice packs for three days for both the intervention and control groups. |
|
What type of outcomes were measured? |
The trials reported multiple outcomes, which were grouped by the systematic reviews as follows:
The follow-up of one trial [13] was six months, while the follow-up of the other study [13] was 18 months. |
*Information on primary studies is extracted from the identified systematic reviews and not directly from the studies unless otherwise specified.
Summary of results
Information on the effects of adding melatonin to hypothermia therapy for neonatal hypoxic-ischemic encephalopathy is based on two trials [13],[14] involving 55 patients. Both trials [13],[14] measured mortality, the presence of seizures, and brain magnetic resonance imaging alterations. One trial [13] measured neurological examinations at six months, while the other trial [14] assessed neurodevelopment at six and 18 months. None of the trials reported the presence of clinical adverse effects.
The summary of the results is as follows:
- It is not possible to establish whether adding melatonin to hypothermia therapy compared to hypothermia monotherapy decreases mortality because the certainty of the existing evidence has been assessed as very low.
- It is not possible to establish whether adding melatonin to hypothermia therapy compared to hypothermia monotherapy decreases the likelihood of having brain magnetic resonance imaging alterations because the certainty of the existing evidence has been assessed as very low.
- Adding melatonin to hypothermia compared to hypothermia monotherapy may increase the likelihood of a normal neurologic examination at six months (low certainty of the evidence).
- Adding melatonin to hypothermia compared to hypothermia monotherapy could increase the likelihood of normal cognition at 18 months (low certainty of the evidence).
- Adding melatonin to hypothermia use compared to hypothermia monotherapy is likely to decrease the likelihood of seizures (moderate certainty of the evidence).
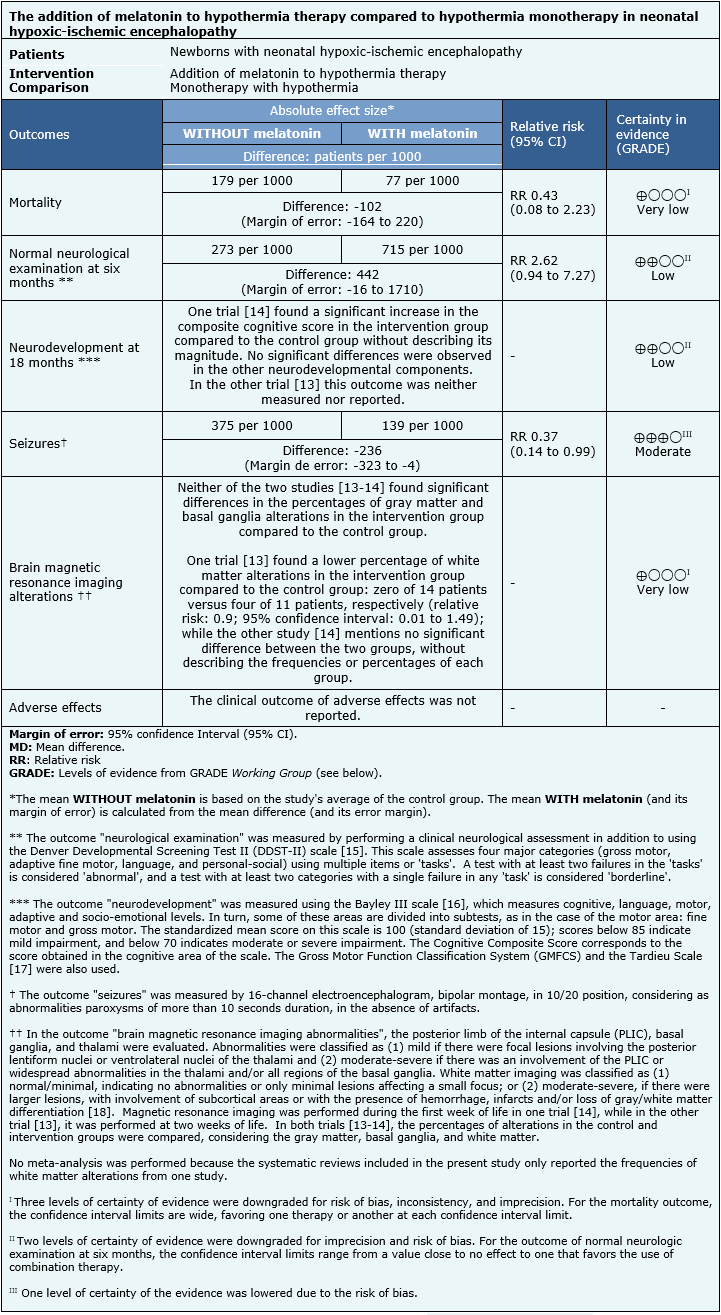 Full size
Full size Follow the link to access the interactive version of this table (Interactive Summary of Findings - iSoF)
|
About the levels of evidence (GRADE)* ⊕⊕⊕⊕ ⊕⊕⊕◯ ⊕⊕◯◯ ⊕◯◯◯ *This is also called 'quality of evidence' or 'confidence in the effect estimate'. |
Other considerations for decision-making
|
To whom this evidence applies and to whom it does not apply |
|
|
About the outcomes included in this summary |
|
|
Harm/benefit balance and certainty in evidence |
|
|
Costs |
|
|
What do patients and their caregivers think |
|
|
Differences between this summary and other sources |
|
|
Could this information change in the future? |
|
How we made this summary
Using automated and collaborative methods, we compile all the evidence relevant to the question of interest and present it in an evidence matrix.
Notes
If new systematic reviews on this topic are published after the publication of this abstract, a "new evidence" notice will be displayed at the top of the matrix. While the project envisages regular updating of these abstracts, users are invited to comment on the Medwave website or contact the authors by e-mail if they believe there are evidence that warrants an earlier update.
After creating an Epistemonikos account, by saving the matrices, you will receive automatic notifications whenever there is new evidence that potentially answers this question.
This article is part of the Epistemonikos evidence synthesis project. It is elaborated with a pre-established methodology, rigorous methodological standards, and an internal peer review process. Each of these articles corresponds to a summary called FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence of a specific question in a friendly format for clinicians. Its main resources are based on the Epistemonikos evidence matrix and analysis of results using the GRADE methodology. Further details of the methods to elaborate this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997).
The Epistemonikos Foundation is an organization that seeks to bring information closer to health decision-makers through the use of technologies. Its main development is the Epistemonikos database (www.epistemonikos.org).

