Epistemonikos summaries
← vista completaPublished on March 10, 2015 | http://doi.org/10.5867/medwave.2015.02.6082
Is iloprost effective in secondary Raynaud's phenomenon?
¿Es efectivo el iloprost en el fenómeno de Raynaud secundario?
Abstract
Patients with systemic sclerosis frequently have Raynaud's phenomenon and digital ischemic ulcers. Iloprost, a synthetic prostacyclin analogue, may be effective in these cases. Searching in Epistemonikos database, which is maintained by screening 20 databases, we identified three systematic reviews including seven randomized trials. We combined the evidence using meta-analysis and generated a summary of findings table following the GRADE approach. We concluded iloprost may lead to little or no difference in the frequency or severity of secondary Raynaud, and it is associated to adverse effects and important costs.
Problem
Systemic sclerosis is a connective tissue disease characterized by fibrosis and vascular phenomena that frequently affect the skin and other organs. About 90% of patients with systemic sclerosis suffer from secondary Raynaud’s phenomenon, which is usually more severe and it is accompanied by digital ischemic ulcers that carry the risk of infection, gangrene, osteomyelitis and amputation.
Iloprost, a synthetic prostacyclin analogue with vasodilatory effect, has been proposed as a treatment for Raynaud’s phenomenon associated to systemic sclerosis.
Methods
We used Epistemonikos database, which is maintained by screening more than 20 databases, to identify systematic reviews and their included primary studies.
With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
Acerca del conjunto de evidencia para esta pregunta
|
What is the evidence. See evidence matrix in Epistemonikos later |
We found three systematic reviews [1],[2],[3] including seven randomized controlled studies comparing iloprost vs placebo [4],[5],[6],[7],[8],[9],[10]. One of the studies did not report usable data for our analysis, so it is not considered in this table or in the summary of findings [5]. |
| What types of patients were included. |
All studies included patients with systemic sclerosis exclusively, except one that also included patients with severe primary Raynaud’s [6], but presented data in a way that allowed to separate the information of the systemic sclerosis group. Patients included in the studies presented a mean of 18 to 28 attacks per week [4],[7],[9],[10]. Two studies included patients with more than 12 episodes per week [6], but did not report average baseline frequency, and one study did not report any data on this regard [8]. |
|
What types of interventions were included. |
Two studies evaluated oral iloprost [4],[7], and the rest administered it intravenously. The duration of treatment was variable, from three days to six weeks in the different studies. |
|
What types of outcomes were measured. |
Frequency, severity and duration of attacks; global evaluation of the impact of Raynaud’s phenomenon made by patients or physicians; digital ulcer healing; Raynaud’s score, etc. |
Summary of findings
This information is based on six of seven randomized studies identified, including 595 patients. Five studies reported frequency [4],[6],[7],[9],[10], and four severity of attacks [4],[6],[8],[9]. Three studies measured digital ulcer healing [6],[8],[9], but only two reported data adequately [8],[9]. Adverse effects were reported in four studies [4],[7],[8],[9].
• Iloprost may lead to little or no difference in the frequency or severity of secondary Raynaud.
• It is not known if iloprost affects digital ulcer healing because the certainty of the evidence was estimated as very low.

Matrix of evidence: Iloprost vs placebo for secondary Raynaud’s phenomenon
Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
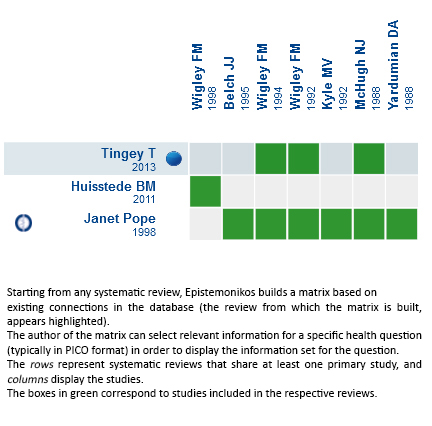 Full size
Full size Follow the link to access the interactive version Iloprost vs placebo for secondary Raynaud’s phenomenon

Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary.
Even though the project considers the periodical update of these summaries, users are invited to comment in the website of Medwave or to contact the authors through email if they realize there is new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce this summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organisation aiming to bring information closer to those making health decisions, through the use of technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.

