Epistemonikos summaries
← vista completaPublished on June 5, 2015 | http://doi.org/10.5867/medwave.2015.05.6148
Urethroplasty with buccal mucosa graft or penile skin graft for anterior urethral stricture?
¿Uretroplastía con injerto de mucosa oral o piel prepucioescrotal para el tratamiento de la estrechez de uretra anterior?
Abstract
Currently the treatment for urethral stricture considers various techniques, including augmentation urethroplasty using tissue from different parts of the body. The more used are the buccal mucosa and penile skin, but are there any differences in success between both tissues? Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified one systematic review including 18 primary studies addressing this question, six of them prospective. We combined the evidence using meta-analysis and generated a summary of findings table following the GRADE approach. We concluded there is uncertainty about the superiority of one technique over another because the certainty of the evidence is very low. A new systematic review is urgently needed on this topic as randomized studies have been published after the most recent review, which could provide greater certainty.
Problem
The urethral stricture is a condition that leads a significant deterioration in the quality of life and is associated to high costs [1]. Its frequency is increasing due to the increase in life expectancy [2],[3], which determines a higher probability of manipulation of the urinary tract and infections, in addition to the loss in the scarring potential of the urinary tract, among other factors .
The vast majority of urethral strictures are treated by internal urethrotomy dilation under direct vision, which is not a curative procedure and has a high rate of recurrence [4]. Among the alternative curative treatments is urethral augmentation, which employs various tissue transfer techniques in order to restore complete functionality. Choosing the right treatment depends on the etiology, location, length of the narrow urethra, among other factors. There is still controversy about the effectiveness of different types of tissues used to achieve an optimal result, being penile skin and buccal mucosa the most frequently used.
Methods
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found one systematic review [5] including 18 primary studies [6-23],six of them prospective [10],[11],[14],[17],[19],[23] and the rest retrospective [6-9],[12],[13],[15],[16],[18],[20-22]. |
|
What types of patients were included |
All studies included male patients over 18 years. Most studies included patients with different causes of urethra stricture, except in five studies which included post- traumatic causes [15], previously transplanted kidney - pancreas [11], neurogenic bladder related to urethral pathology [14], previously instrumented [10] and primary treatment of failed hypospadias [19].The extent of urethral stricture ranged from 1.5 cm to eight centimeters in the different studies. It is important to notice there were differences in the extent between groups, being on average 6.2 cm in patients using penile skin versus 4.6 cm in those using buccal mucosa. The location of the stricture was the anterior urethra (includes penile and bulbar urethra ) in four studies [13],[14],[21],[23], only penile urethra in four [8],[10],[11],[19], only bulbar urethra in seven [6],[7],[9],[17],[18],[20],[22] and three studies considered all segments of the urethra [12],[15],[16]. |
|
What types of interventions were included |
The surgical techniques used in the primary studies were: increased anastomosis , combined urethroplasty, dorsal onlay , lateral onlay , urethroplasty in one stage, two-stage urethroplasty and ventral onlay. |
|
What types of outcomes were measured |
Success was defined in all studies as the absence of need for manipulation of the urethra (urethrotomy , dilatation , cystoscopy , urethrocystography, etc.) after urethroplasty Only one study measured quality of life , lower urinary tract symptoms and Qmax post urethroplasty [17]. The follow-up time was 64.1 months for patients who used penile skin versus 42.1 months for those who used buccal mucosa. |
Summary of findings
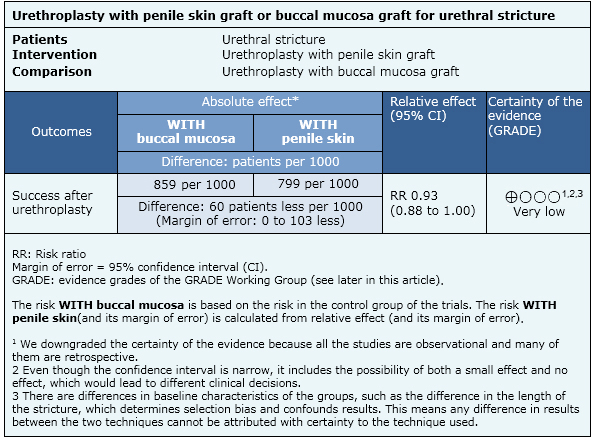
The information about the differential effect of urethroplasty using buccal mucosa graft or penile skin graft for urethral stricture is based on 18 studies comprising 911 patients.
- There is uncertainty about whether urethroplasty with buccal mucosa tissue or penile skin lead to greater success because the certainty of the evidence is very low.
Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
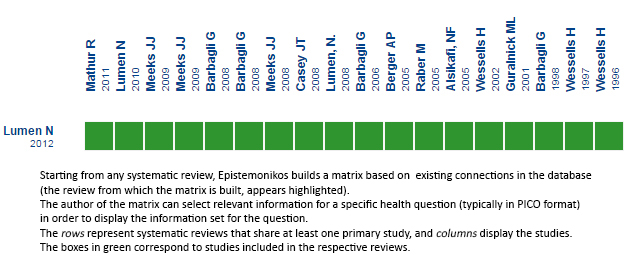 Full size
Full size Follow the link to access the interactive version Buccal mucosa graft vs penile skin graft for urethroplasty in anterior urethral stricture

Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.

