Epistemonikos summaries
← vista completaPublished on July 7, 2015 | http://doi.org/10.5867/medwave.2015.6177
Is there any difference between angiotensin converting enzyme inhibitors and angiotensin receptor blockers for heart failure?
¿Existe alguna diferencia entre los inhibidores de la enzima convertidora y los antagonistas del receptor de angiotensina para la insuficiencia cardiaca?
Abstract
Angiotensin receptor blockers are usually considered as equivalent to angiotensin converting enzyme inhibitors for patients with heart failure and low-ejection fraction. Some guidelines even recommend the former as first line treatment given their better adverse effects profile. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified four systematic reviews including eight pertinent randomized controlled trials. We combined the evidence using meta-analysis and generated a summary of findings following the GRADE approach. We concluded angiotensin receptor blockers and angiotensin converting enzyme inhibitors probably have a similar effect on mortality, and they might be equivalent in reducing hospitalization risk too. Treatment withdrawal due to adverse effects is probably lower with angiotensin receptor blockers than with angiotensin converting enzyme inhibitors.
Problem
Angiotensin converting enzyme inhibitors decrease morbidity and mortality in patients with heart failure and systolic dysfunction. It is generally accepted angiotensin receptor blockers have similar benefits, but recommendations vary in the different guidelines, ranging from using them as first-line treatment to reserve them to patients intolerant to angiotensin converting enzyme inhibitors.
Methods
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found four systematic reviews [1],[2],[3],[4] including eight randomized controlled trials [5],[6],[7],[8],[9],[10],[11],[12]. |
|
What types of patients were included |
The average age between studies ranged from 56 to 74 years. All studies included patients with heart failure of any etiology, and the most common cause was ischemic. No study included NYHA functional class I patients. All studies restricted inclusion to low ejection fraction patients; two studies required ejection fraction lower than 45% [8],[9], five < 40% [5],[6],[7],[10],[11] and one < 35% [12]. |
|
What types of interventions were included |
The angiotensin converting enzyme inhibitors used in the studies was enalapril in five [5],[6],[8],[9],[12], captopril in two [7],[11] and lisinopril in one [10]. The Angiotensin receptor blocker used as comparator was losartan in four studies [7],[9],[11],[12], valsartan in two [8],[10], telmisartan in one [6] and candesartan in one [5]. |
|
What types of outcomes were measured |
All-cause mortality or cardiovascular death, all-cause hospitalization, treatment withdrawal, quality of life, exercise tolerance, neurohumoral biomarkers and echocardiographic parameters. |
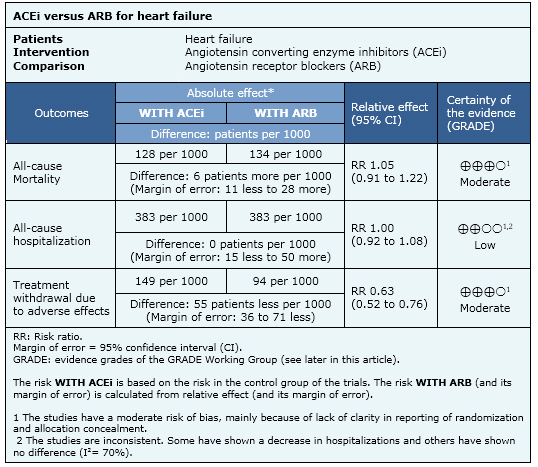
Summary of findings
The information on the effects of carvedilol is based on eight randomized controlled trials including 5201 patients. All studies reported mortality and three reported all-cause hospitalization, [5],[7],[11].
- Angiotensin receptor blockers and angiotensin converting enzyme inhibitors probably have a similar effect on mortality. The certainty of the evidence is moderate.
- Angiotensin receptor blockers and angiotensin converting enzyme inhibitors might be equivalent in reducing hospitalization. The certainty of the evidence is low.
- Treatment withdrawal due to adverse effects is probably lower with angiotensin receptor blockers than with angiotensin converting enzyme inhibitors. The certainty of the evidence is moderate.
Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
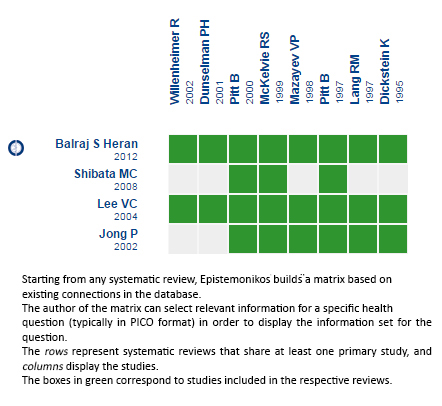 Full size
Full size Follow the link to access the interactive version Angiotensin-receptor blockers versus angiotensin converting enzyme inhibitors for heart failure
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.

