Resúmenes Epistemonikos
← vista completaPublicado el 8 de enero de 2016 | http://doi.org/10.5867/medwave.2015.6357
¿Es necesaria la profilaxis antibiótica para el taponamiento nasal en epistaxis anterior?
Is antibiotic prophylaxis in nasal packing for anterior epistaxis needed?
Abstract
Epistaxis is an extremely common problem that sometimes requires anterior nasal packing. Antibiotics are frequently indicated to prevent infectious complications, although the role of this measure is controversial. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified one systematic review including three primary studies, none of them randomized. We combined the evidence using meta-analysis and generated a summary of findings table following the GRADE approach. We concluded it is not clear whether prophylactic antibiotics reduce infectious complications in patients with nasal packing for anterior epistaxis because the certainty of the evidence is very low.
Problem
Epistaxis is a common problem that usually resolves spontaneously. However, in some cases it requires hospital care and interventions of different complexity. Among these, one of the most common is anterior nasal packing, after which antibiotics are commonly indicated in order to prevent infectious complications.
Methods
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found only one systematic review [1] including three non-randomized studies, two of them retrospective and one prospective [2],[3],[4]. |
|
What types of patients were included |
All of the studies included patients treated in emergency rooms for spontaneous anterior epistaxis requiring nasal packing and/or other intervention. |
|
What types of interventions were included |
All studies compared use of prophylactic antibiotics against no antibiotics. Amoxicillin-clavulanic acid was used in all of the studies, although others as clarithromycin and piperacillin/tazobactam were also used [3],[4]. |
|
What types of outcomes |
The outcome measured by the studies was "infectious complications". This term refers to bacterial sinusitis, acute otitis media and staphylococcal toxic shock. It was measured through questionnaires and/or laboratory or radiological examinations when needed. |
Summary of findings
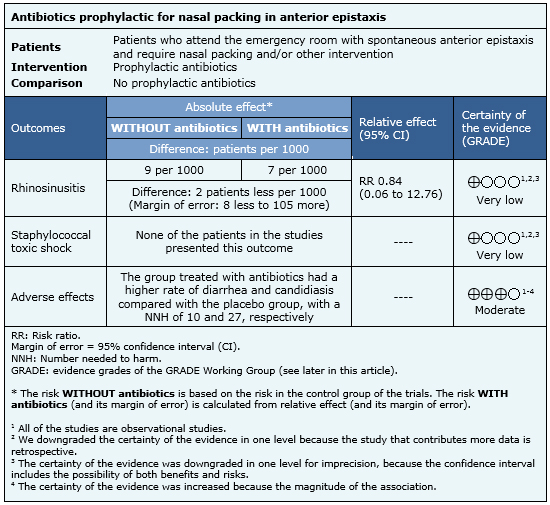
Information on the effects of antibiotics in patients with nasal packing for epistaxis is based on three non-randomized studies involving 234 patients. All studies measured bacterial rhinosinusitis and staphylococcal toxic shock. The information on the adverse effects comes from a systematic review including 45 randomized controlled studies [5].
- It is not clear whether antibiotic prophylaxis decreases the risk of sinusitis in patients with nasal packing for anterior epistaxis. The certainty of the evidence is very low.
- It is not clear whether antibiotic prophylaxis reduces the risk of staphylococcal toxic shock in patients with nasal packing for anterior epistaxis. The certainty of the evidence is very low.

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
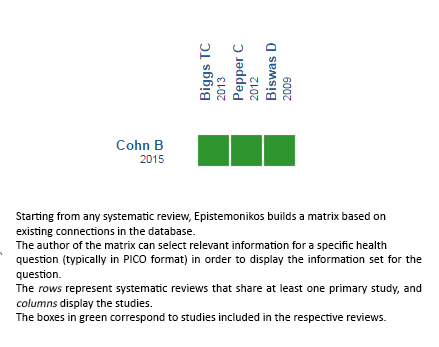
Follow the link to access the interactive version: Prophylactic antibiotics for anterior nasal packing in epistaxis
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.

