Epistemonikos summaries
← vista completaPublished on March 22, 2016 | http://doi.org/10.5867/medwave.2016.6385
Laparoscopy or open surgery for the treatment of hydatid cyst?
¿Cirugía laparoscópica o abierta para el tratamiento del quiste hidatídico?
Abstract
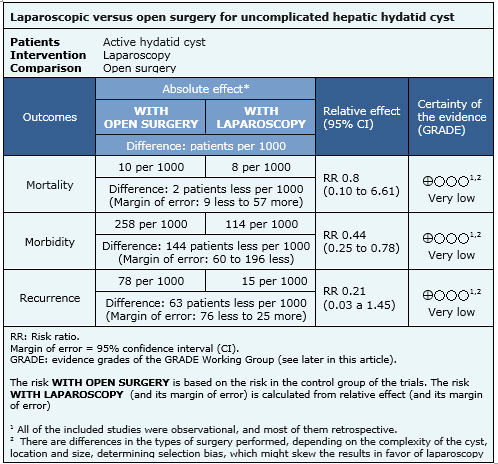
The laparoscopic approach has taken a prominent role in the last decades for various surgical conditions, including liver hydatid cyst. However there is controversy about whether it can replace open surgery. Using Epistemonikos database, which is maintained by screening 30 databases, we identified three systematic reviews which together include four relevant studies, all nonrandomized. We combined the evidence using meta-analysis and generated a summary of findings table following the GRADE approach. We concluded it is unclear whether laparoscopy for hepatic hydatid cyst reduces mortality, morbidity or recurrence compared with open surgery because the certainty of the evidence is very low.
Problem
Hydatid cyst or hydatid disease is a zoonosis caused by Echinococcus granulosus. It is widely spread throughout the world, with endemic areas in the Mediterranean, South America, New Zealand, Australia, among others [1]. It may compromise multiple organs, but the most commonly affected is the liver. There are various treatments, from medical management with anthelmintics to more aggressive treatments such as surgery, which is currently considered as standard of treatment [2]. This can be done by radical surgery (hepatectomy or pericystectomy) or conservative (cystectomy, deroofing, omentoplasty, among others). Radical surgery has shown the lowest long-term risk of recurrence [2].
With the development of minimally invasive techniques, laparoscopic approach has taken a prominent role in various surgical conditions, including hepatic hydatid disease.
Methods
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found three systematic reviews [2],[3],[4], which include four studies relevant to our question, none of them randomized. Three were retrospective [6],[7],[8] and one prospective [5]. |
|
What types of patients were included |
The studies included patients older than 10 years with active liver hydatid cyst (cysts type I to IV or CE1 to CE4). One study [8] excluded patients with cysts located in segment 1 and 7 and with evidence of intrabiliary rupture. None of the studies included emergency surgery for complicated cyst. |
|
What types of interventions were included |
All studies compared laparoscopy versus open surgery [5],[6],[7],[8]. Regarding the different types of surgery, studies divided it into conservative surgery where only the membrane was removed and pericystic parasite remained in the liver, and radical procedures including pericystectomy and liver resection. Two studies [6],[8] included only conservative laparoscopic management in the laparoscopy group, and one study [8] did not include radical surgery in the open surgery group. |
|
What types of outcomes |
Perioperative mortality and morbidity, relapse and hospital stay were compared across studies included in the summary. They also measured general complications such as fever of unknown origin, subcutaneous hematoma, pleural effusion or empyema, pneumonia, atelectasis, drug induced fever and hyperosmolar coma. |
|
We found three systematic reviews [5], [6], [7], including 14 studies reported in 21 references [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28]. Eight studies correspond to randomized controlled trials (15 references [9], [10], [11], [12], [13], [14], [16], [17], [19], [21], [22], [23], [24], [26], [27]). This table and the summary in general are based on the latter. One study [15] did not contribute data to any of the outcomes of interest. |
Summary of findings
The information on the effects of laparoscopic hepatic hydatid disease management is based on one prospective and three retrospectives studies including 486 patients. All studies reported the outcomes mortality, perioperative morbidity and recurrence.
- It is unclear whether the management of hepatic hydatid cyst by laparoscopy reduces mortality compared with open surgery because the certainty of the evidence is very low.
- It is unclear whether the management of hepatic hydatid cyst by laparoscopy reduces morbidity compared with open surgery because the certainty of the evidence is very low.
- It is unclear whether the management of hepatic hydatid cyst by laparoscopy reduces recurrences compared with open surgery because the certainty of the evidence is very low.

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
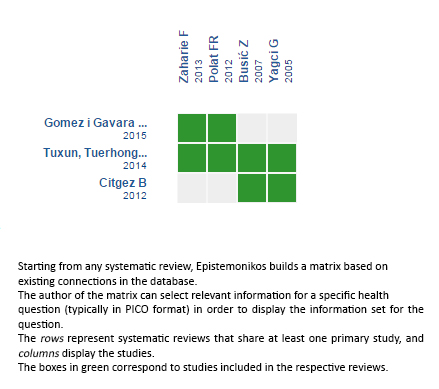
Follow the link to access the interactive version: Laparoscopic versus open surgery for liver cystic echinococcosis
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.

