Epistemonikos summaries
← vista completaPublished on August 3, 2016 | http://doi.org/10.5867/medwave.2016.6496
Should prophylactic measures to prevent postpolypectomy bleeding after resection of large colorectal polyps be used?
¿Deben realizarse medidas profilácticas para evitar el sangrado postpolipectomía luego de resecar pólipos colorrectales grandes?
Abstract
Post-polypectomy bleeding after colonoscopy with resection of large colorectal polyps can cause significant morbidity (readmission for monitoring, transfusion, repeat endoscopy and therapy) and a significant cost to hospitals and insurers. Nevertheless prophylactic endoscopic measures could reduce risk of post-polypectomy bleeding. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified two systematic reviews including 10 randomized trials. We combined the evidence using meta-analysis and generated a summary of findings table following the GRADE approach. We concluded prophylactic endoscopic measures could be effective in reducing post-polypectomy bleeding after resection of large colorectal polyps.
Problem
Colorectal cancer is the third leading cause of cancer death in Western populations [1],[2]. Colonoscopy has become the most widely accepted method for colon cancer screening because it reduces mortality and the incidence of cancer by identification and removal of precancerous lesions [3],[4],[5],[6],[7],[8].
Bleeding is the most frequently observed complication after polypectomy that can occur early (during and within 24 hours of the procedure) or delayed (usually in the first few days until four weeks after colonoscopy). postpolypectomy bleeding can cause significant morbidity (readmission for monitoring, transfusion, repeat endoscopy and therapy) and a significant cost to hospitals and insurers.
The main predictor of postpolypectomy bleeding is the size of the polyp. For example, for polyps > 20 mm located in the right colon, postpolypectomy bleeding rates exceeding 10% have been reported [9],[10],[11],[12],[13],[14],[15],[16],[17].
Prophylactic measures like adrenaline injection, argon plasma coagulation or mechanical haemostasis (endoclips or endoloops) have been studied. These interventions could reduce risk of bleeding but have not been universally adopted for endoscopists, or recommended in guidelines [18],[19],[20],[21],[22],[23],[24].
Methods
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found two systematic reviews [25],[26], which include 10 randomized controlled trials [19],[20],[21],[22],[23],[24],[27],[28],[29],[30]. |
|
What types of patients were included |
Patients undergoing colonoscopy with resection of colorectal polyps larger than 10 mm. |
|
What types of interventions were included |
Prophylactic endoscopic haemostatic measures (adrenaline injection, argon plasma coagulation, endoclips or endoloops). |
|
What types of outcomes |
Early (within 24 hours of the procedure) or delayed bleeding (first few days until four weeks after colonoscopy). Presenting as haematochezia, >10% drop in haematocrit or decrease in the level of hemoglobin > 1 mg/d. Length of hospital stay Postpolypectomy syndrome (abdominal pain, fever, leukocytosis, increased C-Reactive Protein, or signs or symptoms of peritoneal irritation 4 to 24 hours after colonoscopic polypectomy with electrocoagulation in the absence of visualized perforation on abdominal computed tomography). |
Summary of findings
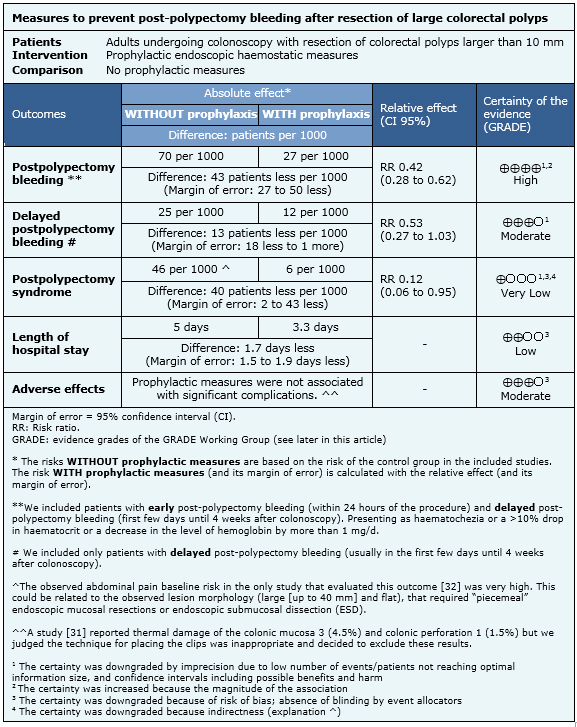
Information on the effects of endoscopic prophylactic haemostatic measures for postpolypectomy bleeding is based on 13 randomized trials involving 4,899 patients.
Ten studies assessed at least one prophylactic measure versus no prophylaxis; five compared adrenaline versus no intervention or placebo (saline solution injection]; one study compared detachable snare (endoloop) versus no intervention; another study compared endoloop or adrenaline versus no intervention; and three studies assessed clips versus no intervention. The remaining three studies compared different prophylactic measures (clips + endoloop versus adrenaline, endoloop + adrenaline versus adrenaline, and argon plasma coagulation versus adrenaline).
All studies reported total postpolypectomy bleeding (early + delayed), and seven studies also informed delayed bleeding. Three studies reported length of hospital stay but the information could only be extracted for two of them. One study also assessed postpolypectomy syndrome [19],[20],[21],[22],[23],[24],[27],[28],[29],[30],[31],[32].
The summary of findings is the following:
- Prophylactic measures (adrenaline injection, argon plasma coagulation, clips or endoloops) are effective in reducing the risk of total postpolypectomy bleeding (early + delayed) after resection of large colorectal polyps. The certainty of the evidence is high.
- Use of prophylactic measures (adrenaline injection, argon plasma coagulation, clips or endoloops) could be effective in reducing the length of hospital stay. The certainty of the evidence is low.
- The use of combined prophylactic mechanical measures (clips or endoloops) or argon plasma coagulation, plus adrenaline could be more effective than single adrenaline injection in reducing the risk of global postpolypectomy bleeding. The certainty of the evidence is low.
- The effect of prophylactic measures on postpolypectomy syndrome is not clear because the certainty of the evidence is very low.
- Prophylactic measures (adrenaline injection, argon plasma coagulation, clips or endoloops) are probably not associated with significant complications. The certainty of the evidence is moderate.

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
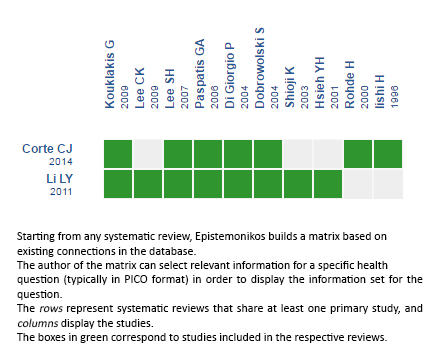
Follow the link to access the interactive version: Prophylactic endoscopic treatments for colorectal postpolypectomy bleeding
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.

