Resúmenes Epistemonikos
← vista completaPublicado el 14 de octubre de 2016 | http://doi.org/10.5867/medwave.2016.6577
¿Es efectivo el uso de terapia electroconvulsiva en el tratamiento de pacientes con esquizofrenia resistente que usan clozapina?
Is electroconvulsive therapy effective as augmentation in clozapine-resistant schizophrenia?
Abstract
Clozapine is considered to be the most effective antipsychotic drug for patients with treatment resistant schizophrenia, but up to a third of the patients do not respond to this treatment. Various strategies have been tried to augment the effect of clozapine in non-responders, one of these strategies being electroconvulsive therapy. However, its efficacy and safety are not yet clear. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified six systematic reviews including 55 studies, among them six randomized controlled trials addressing clozapine-resistant schizophrenia. We combined the evidence using meta-analysis and generated a summary of findings following the GRADE approach. We concluded electroconvulsive therapy probably augments response to clozapine in patients with treatment resistant schizophrenia, but it is not possible to determine if it leads to cognitive adverse effects because the certainty of the evidence is very low.
Problem
Up to 20-30% of patients with schizophrenia receive the diagnosis of treatment resistant schizophrenia, an entity that is defined as the absence of treatment response to two different antipsychotic drugs. In some of these cases, clozapine manages to control patient’s symptoms, but 30-40% of them do not respond to this antipsychotic.
Various strategies have been tried to augment the effect of clozapine in non-responders, one of these strategies being electroconvulsive therapy, or the electric stimulation of the patient’s brain under anesthesia. Its mechanism is not completely understood, but four pathways have been proposed: increased monoamine release, stimulation of the pituitary secretion of TSH, ACTH, endorphins and prolactin, increased neurogenesis, and post-session anticonvulsive effect.
This article seeks to address if electroconvulsive therapy is effective and safe as clozapine-augmentation in patients with treatment resistant schizophrenia.
Methods
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found six systematic reviews [1],[2],[3],[4],[5],[6] that include 55 primary studies [7],[8],[9],[10],[11],[12], [13],[14],[15],[16],[17],[18],[19],[20],[21],[22],[23], [24],[25],[26],[27],[28],[29],[30],[31],[32],[33],[34], [35],[36],[37],[38],[39],[40],[41],[42],[43],[44],[45], [46],[47],[48],[49],[50],[51],[52],[53],[54],[55],[56],[57], [58],[59],[60],[61], 24 of which are randomized control trials [7],[8],[9],[10],[11],[12],[13],[14],[15],[16],[17], [17],[18],[19],[20],[21],[22],[23],[24],[25],[26],[27],[28], [29],[30]. In six of the latter [7],[8],[9],[12],[16],[17], the patients were treated with clozapine, ergo our review will focus mainly in those studies. Nonetheless, the information about some of the outcomes was only reported in observational studies, and will be included in our analysis. |
|
What types of patients were included |
Four of the six randomized trials made the diagnosis of schizophrenia with CCMD-3 criteria [8],[9],[12],[17] and only one with DSM-IV criteria [16]. One study did not report the diagnostic method [7]. Two studies [9],[16] defined resistance as the lack of treatment response to two or more antipsychotics, while three studies defined it as the lack of response to three or more [8],[12],[17]. One study did not report the way in which they defined treatment resistance [7]. The observational studies [38],[55],[62] did not describe the diagnostic criteria used to define schizophrenia or how they defined treatment resistance. |
|
What types of interventions were included |
One trial [17] did not report the dose of clozapine used, three trials used >600mg/day of chlorpromazine equivalents [8],[9],[16], one used >250mg/day [7] and one used >1000mg/day [12]. The trials used 6 to 20 sessions of electroconvulsive therapy, but one study [7] did not report the number of sessions. The observational studies did not report the number of electroconvulsive therapy sessions used. Four trials performed electroconvulsive therapy sessions 2-3 times per week [8],[9],[16],[17] and two trials did not report the frequency [7],[12]. The observational studies [38],[55],[62] did not describe the dose or the frequency of electroconvulsive therapy. All trials compared the intervention against placebo or standard treatment. |
|
What types of outcomes |
The systematic reviews evaluated the symptoms improvement according to any definition provided in the studies. The primary studies defined symptomatic improvement as a change in the Positive and Negative Syndrome Scale ≥20% [17], ≥25% [9] or ≥40% [16], or as a change in the Brief Psychiatric Rating Scale (BPRS) of ≥20% [7] or ≥25% [8],[12]. Only one systematic review evaluated the cognitive performance after electroconvulsive therapy [6]. |
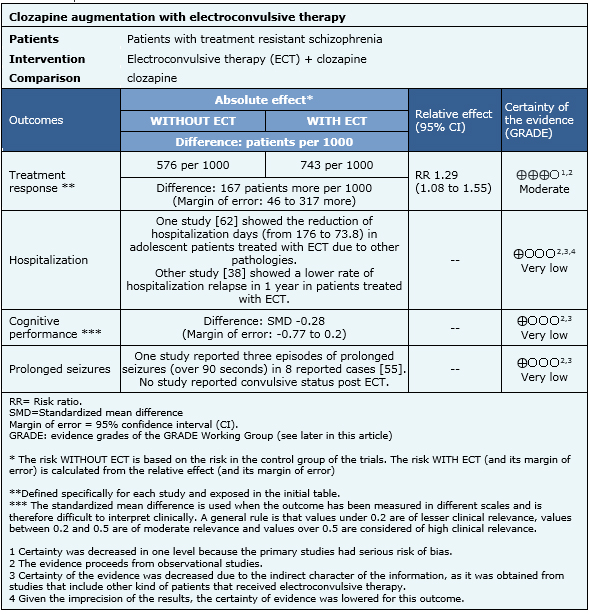
Summary of findings
The information about the effects of electroconvulsive therapy is based on six randomized trials that include 368 patients, and in three observational studies for the outcomes in which no information was found in the trials. All of the trials measured treatment response. The information regarding performance in cognitive tests was reported in one systematic review [6], which included four primary studies for the measurement of the outcome. The presence of prolonged seizures was evaluated in only one observational study [55] and the influence over hospitalization days was reported in two observational studies [38],[62].
- Electroconvulsive therapy probably augments the effect of clozapine treatment in patients with treatment resistant schizophrenia. The certainty of the evidence is moderate.
- It is not clear whether electroconvulsive therapy decreases the need of hospitalization in patients with treatment resistant schizophrenia because the certainty of the evidence is very low.
- It is not clear whether electroconvulsive therapy produces cognitive adverse effects because the certainty of the evidence is very low.
- It is not clear whether electroconvulsive therapy increases the risk of seizures because the certainty of the evidence is very low.

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
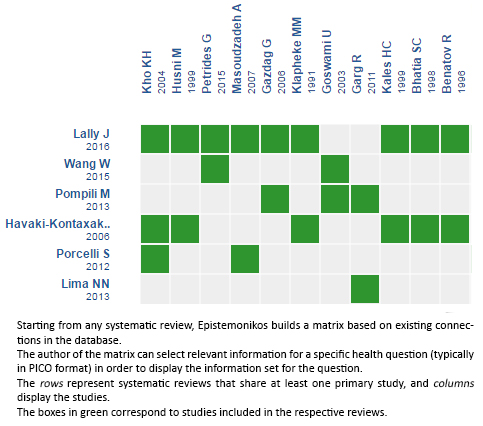
Follow the link to access the interactive version: Electroconvulsive therapy for treatment resistant schizophrenia.
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.

