Epistemonikos summaries
← vista completaPublished on January 13, 2017 | http://doi.org/10.5867/medwave.2017.6821
Are cannabinoids effective for epilepsy?
¿Son efectivos los cannabinoides en la epilepsia?
Abstract
Several beneficial effects have been proposed for cannabinoids in different clinical conditions, including epilepsy. However, their clinical role is controversial. Searching in Epistemonikos database, which is maintained by screening multiple databases, we identified five systematic reviews including four randomized trials addressing the question of this article. We extracted data and generated a summary of findings following the GRADE approach. We concluded it is not clear whether cannabinoids reduce the frequency of seizures in epilepsy because the certainty of the evidence is very low, and they probably increase adverse effects.
Problem
Epilepsy is a condition that disturbs the normal functioning of the brain and it is characterized by stereotyped and recurrent seizures. Although antiepileptic drugs usually achieve disease control, about 30% of patients have persistent seizures. Both tetrahydrocannabinol and cannabidiol have anticonvulsant properties by activating the CB1 and/or CB2 receptors of endocannabidiol system. However, their actual clinical role is not clear.
Methods
We used Epistemonikos database, which is maintained by screening multiple information sources, to identify systematic reviews and their included primary studies. With this information, we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found five systematic reviews [1],[2],[3],[4],[5] including six primary studies [6],[7],[8],[9],[10],[11], of which four [6],[7],[8],[9] correspond to randomized controlled trials.This table and the summary in general are based on the latter. |
|
What types of patients were included |
All trials [6],[7],[8],[9] included patients with epilepsy, however only one trial [9] specified the type of epilepsy (secondarily generalized). |
|
What types of interventions were included |
All trials [6],[7],[8],[9] compared oral cannabidiol in different doses and different periods against placebo. |
|
What types of outcomes |
The systematic reviews identified [1],[2],[3],[4],[5] grouped outcomes in the following way: |
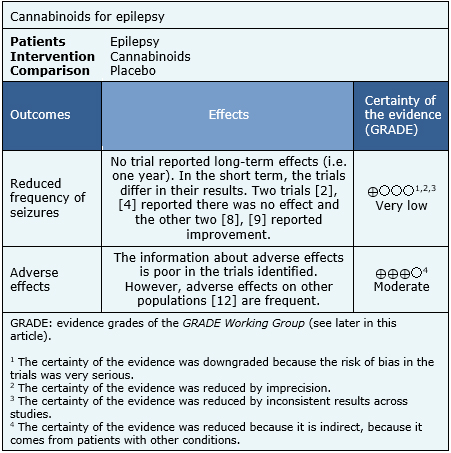
Summary of findings
The information about the effects of cannabinoids for control of epilepsy is based on four randomized trials including 48 patients [6],[7],[8],[9]. All of the trials reported both the frequency of seizures and adverse effects associated with its use, but none of the systematic reviews was able to conduct a meta-analysis with their data. The information on adverse effects was supplemented with a systematic review evaluating the adverse effects of cannabinoids in different populations, and includes 29 studies reporting this outcome [12]. The summary of findings is as follows:
- It is not clear whether cannabinoids reduce the frequency of seizures because the certainty of the evidence is very low.
- Cannabinoids are probably associated with transient but frequent adverse effects. The certainty of the evidence is moderate.

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
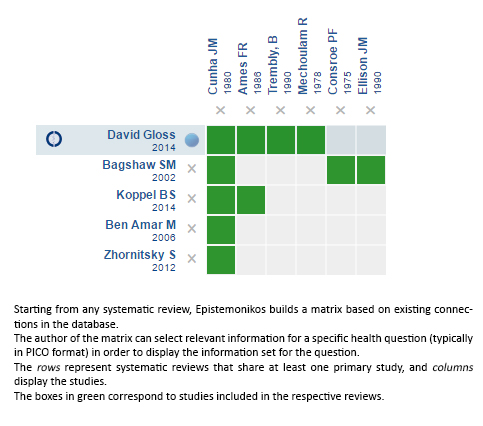
Siga el enlace para acceder a la versión interactiva: Cannabinoids for epilepsy
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.

