Epistemonikos summaries
← vista completaPublished on November 15, 2017 | http://doi.org/10.5867/medwave.2017.09.7081
Early versus late surgical correction in congenital diaphragmatic hernia
Corrección temprana versus tardía en hernia diafragmática congénita
Abstract
INTRODUCTION The timing of surgical repair in patients with congenital diaphragmatic hernia has been a controversial topic over the years, and there is still no agreement as to whether immediate repair or late surgery with preoperative stabilization is preferable.
METHODS To answer this question we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS We identified four systematic reviews including 38 studies overall, of which two were randomized trials. We concluded it is not clear whether immediate surgical repair in congenital diaphragmatic hernia increases mortality or decreases hospitalization days compared to late repair because the certainty of evidence is very low.
Problem
Congenital diaphragmatic hernia presents with a prevalence of 2 to 4 per 10,000 live births and is associated with high mortality and high costs. Despite significant advances in neonatal and surgical care, management of newborns with congenital diaphragmatic hernia remains a challenge. As for timing of surgical repair, since the 1980s most investigators have advocated delayed surgery, post-preoperative stabilization, using a variety of ventilatory strategies. If late surgery is beneficial compared to immediate repair is still a controversial issue; a convincing improvement in survival has not yet been documented after this strategy is implemented. Patients who survive the neonatal period require long-term follow-up as they are more likely to develop important morbidity, such as chronic lung disease, gastroesophageal reflux, growth restriction, neurological and sensory abnormalities. Due to the high mortality and associated morbidity, it is important to find the best possible alternative to lower these rates.
In congenital diaphragmatic hernia, there is a defect in the diaphragm that allows the passage of intra-abdominal organs (small intestine, stomach, spleen, liver, etc.) to the thoracic cavity; this occupation determines compression of the thoracic organs during its development, which causes hypoplasia and pulmonary hypertension, which affect the normal transition of the cardiorespiratory system at the time of birth. One of the most important prognostic factors in these patients is the presence of pulmonary hypertension, also called persistent fetal circulation. Immediate repair may be beneficial in avoiding persistent pulmonary compression, making ventilation easier for these patients in theory. On the other hand, delayed surgery would allow the patient to make a more adequate transition to extra uterine life, allowing time for hemodynamic adaptation to better cope with the impact of early surgery that could aggravate preexisting pulmonary hypertension. Our purpose is to review available evidence about the optimum timing of repair.
Methods
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found four systematic reviews [1],[2],[3],[4] which together include 38 primary studies [5],[6],[7],[8], |
|
What types of patients were included* |
The two randomized trials [5],[6] included newborn patients with congenital diaphragmatic hernia which were symptomatic at birth; one of these with the additional requirement that they were symptomatic at within the 12 hours from birth [6]. |
|
What types of interventions were included* |
The two trials [5],[6] evaluated immediate surgical repair, and compared it with late repair.One trial [5] defined immediate repair to the surgery performed within the first 4 hours of admission to the center, and late repair to that performed at least after 24 hours, at the time when the patient was considered stable. The other trial [6] defined immediate repair to the surgery performed within the first 6 hours of admission to the center, and late repair to that performed after 96 hours, when there was no evidence of pulmonary hypertension. |
|
What types of outcomes |
The studies measured multiple outcomes, however, those that were grouped in the identified reviews were:
|
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
Summary of findings
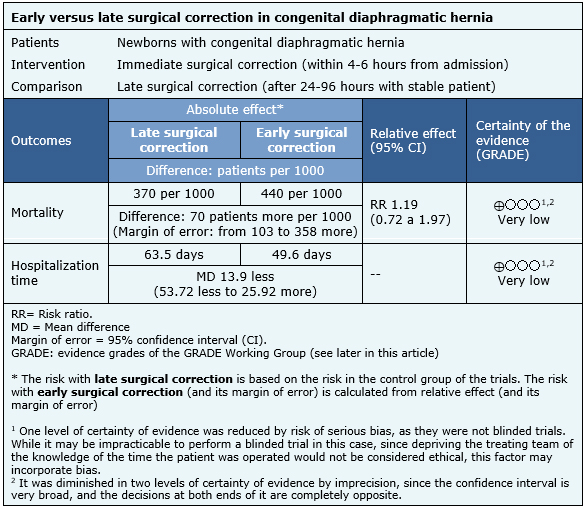
The information on the effects of immediate versus late surgical repair in patients with congenital diaphragmatic hernia is based on two randomized trials [5],[6] including 84 patients in total. Both trials reported the outcome mortality and hospitalization time in survivors. One trial [6] further measured the use of extracorporeal membrane oxygenation, the type of procedure used and the complications associated with the interventions. The summary of findings is as follows:
- It is not clear whether immediate surgical repair in congenital diaphragmatic hernia increases mortality because the certainty of the evidence is very low.
- It is not clear whether immediate surgical repair in congenital diaphragmatic hernia decreases the length of hospitalization, because the certainty of the evidence is very low.
Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
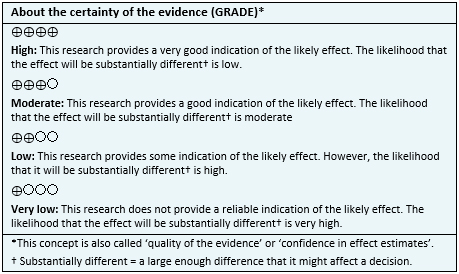
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
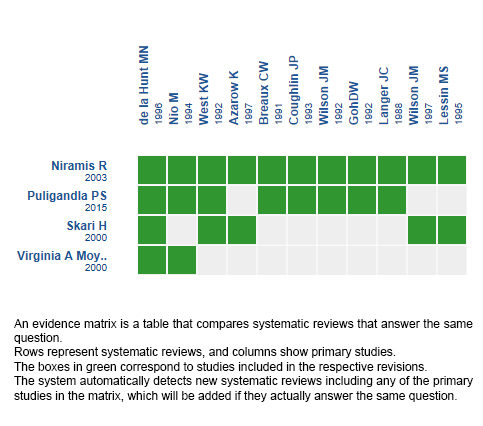
Follow the link to access the interactive version: Late versus early surgical correction for congenital diaphragmatic hernia.
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.

