Resúmenes Epistemonikos
← vista completaPublicado el 26 de diciembre de 2017 | http://doi.org/10.5867/medwave.2017.09.7109
¿Es el ultrasonido de onda pulsátil una alternativa en el tratamiento de la artrosis?
Is pulsed ultrasound an alternative for osteoarthritis?
Abstract
INTRODUCTION Many osteoarthritis patients persist symptomatic despite nonsurgical treatment. Pulsed ultrasound might be a viable alternative for such cases, but its real clinical relevance remains unclear.
METHODS A literature review was conducted in Epistemonikos, the largest database for sys-tematic reviews in health that compiles multiple sources, including MEDLINE, EMBASE, and Cochrane, among others. Relevant data were extracted, and infor-mation from the primary studies was reanalyzed. A subsequent meta-analysis was conducted, and summary of findings tables were constructed using the GRADE methodology.
RESULTS AND CONCLUSIONS Six systematic reviews including eight randomized trials were identified. In conclusion, it is not clear whether pulsed ultrasound improves functionality, and it might slightly decrease pain but the certainty of the evidence is low.
Problem
Osteoarthritis is a highly prevalent disease worldwide and a frequent cause of medical consultation for both, primary care and specialists. The persistence of pain despite nonsurgical treatment is one reason for such consults, and no clearly established alternatives exist for pain management.
Pulsed ultrasound corresponds to the use of sound waves in order to relieve pain or disability. For this purpose, it can direct the beam with a transducer over the area to be treated and it is interrupted in the form of pulsations, allowing higher intensities in order to have a greater effect.
There is no precise information about side effects of the use of therapeutic ultrasound, possibly because they do not exist, or they are very infrequent and related to the use in supra physiological intensities.
Methods
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found six systematic reviews [1],[2],[3],[4],[5],[6] including eight studies overall, corresponding to randomized controlled trials [7],[8],[9],[10],[11],[12],[13],[14]. |
|
What types of patients were included* |
All of the trials focused on osteoarthritis of the knee. Average body mass index (BMI) ranged between 28.75 and 32.2 in four trials [7],[8],[11],[14] and four did not report it [9],[10],[12],[13]. Average age of the participants ranged between 57 and 65 years in the different trials. The proportion of women was between 33 and 100% in the different trials. |
|
What types of interventions were included* |
All of the trials used pulsed ultrasound. One trial used ultrasound with a frequency of 1 MHz and potency of 1.5 W/cm2 in sessions of twelve minutes each, for two weeks (10 sessions in total) [7]. One trial used ultrasound with a frequency of 1 MHz and potency of 1.5 W/cm2 in sessions of fifteen minutes each, for eight weeks (24 sessions in total) [9]. One trial used ultrasound with a frequency of 1 MHz and potency of 2.5 W/cm2 in sessions of fifteen minutes each, three times a week for eight weeks (24 sessions in total) [10]. One trial used ultrasound with a frequency of 1 MHz and potency of 0.2 W/cm2 in sessions of nine and a half minutes each, for eight weeks (24 sessions in total) [11]. One trial used ultrasound with a frequency of 2.5 MHz in sessions of fifteen minutes each, for eight weeks (24 sessions in total) [13]. One trial used ultrasound with a frequency of 1 MHz and potency of 2 W/cm2 in sessions of five minutes each, for two weeks (10 sessions in total) [14]. Two trials did not describe the frequency or the power of the pulsed ultrasound, or the amount of sessions or the duration of them [8],[12]. Two trials associated isokinetic exercises to the pulsed ultrasound [9],[10]. Four trials compared against placebo or standard therapy [10],[11],[12],[13]. Four trials compared against placebo and against continued wave ultrasound [7],[8],[9],[14]. |
|
What types of outcomes |
The outcomes, as classified in the identified systematic reviews, were as follows: effect on the intensity of pain (analyzed as a decrease or improvement) according to visual analogue scale; knee osteoarthritis severity index established by Lequesne; and sub-scale of physical functionality established by the Western Ontario and McMaster Universities Arthritis Index (WOMAC). The average follow-up of the trials was 16 weeks with a range between 2 and 52 weeks. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
Summary of Findings
The information on the effects of pulsed ultrasound was based on three randomized trials that included 200 patients [8],[9],[10]. The remaining trials were not included in the meta-analysis as none of the identified systematic reviews extracted sufficient trial data. The three evaluated trials reported improvement in pain measured with visual analogue scale, and functionality by Lequesne knee osteoarthritis severity index. The summary of findings is as follows:
- Pulsed ultrasound could lead to a small decrease in pain in osteoarthritis, but the certainty of the evidence is low.
- It is not clear if the use of pulsed ultrasound produces an improvement in functionality in patients with osteoarthritis, because the certainty of the evidence is very low.
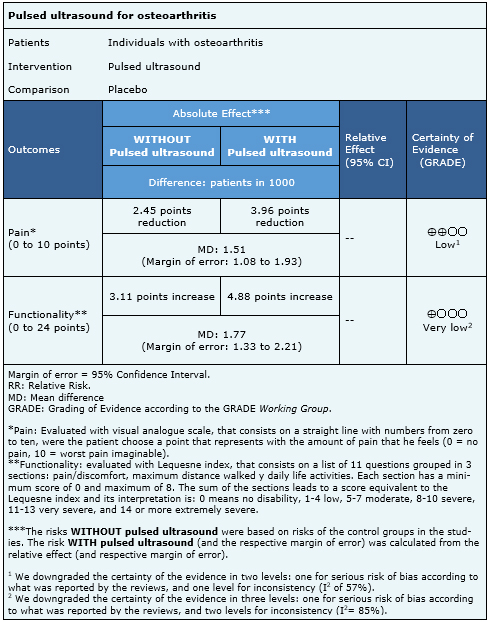
| Visit the following link to access the interactive version of this table (Interactive Summary of Findings - iSoF) |

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
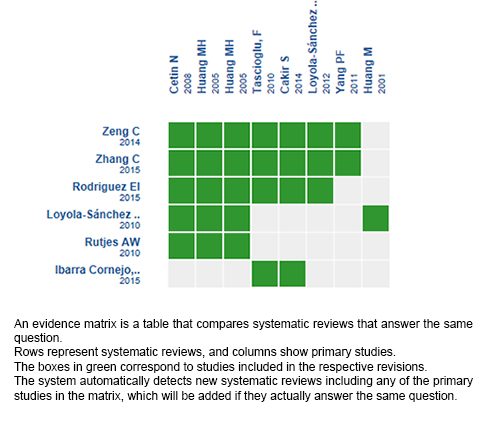
Follow the link to access the interactive version: Pulsed ultrasound versus placebo for osteoarthritis
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.

