Resúmenes Epistemonikos
← vista completaPublicado el 27 de diciembre de 2017 | http://doi.org/10.5867/medwave.2017.09.7115
¿Es efectiva la pregabalina perioperatoria para reducir el dolor postoperatorio en cirugías mayores?
Is perioperative pregabalin effective for reducing postoperative pain in major surgery?
Abstract
INTRODUCTION Pregabalin is a structural analog of γ-aminobutyric acid that may have a role in acute pain management. It has been used in the perioperative context, but there is controversy regarding its real clinical utility.
METHODS To answer this question we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS We identified 21 systematic reviews including 77 randomized trials. We concluded the use of perioperative pregabalin in major surgeries probably does not produce a clinically important decrease in acute postoperative pain. Although it could decrease nausea, postoperative vomiting and opioid requirements, it also produces an increase in sedation.
Problem
Postoperative pain management is an important aspect of anesthesiology practice. Among the most commonly used drugs to manage acute pain are opioids, which despite being very effective have adverse effects such as nausea, vomiting, sedation and respiratory depression. One of the strategies to reduce these unwanted effects is to use adjuvant analgesics that act through different pathways involved in pain response.
Pregabalin is a structural analog of γ-aminobutyric acid (GABA) that binds to the α2δ subunit of voltage-dependent calcium channels in the central nervous system decreasing the release of various neurotransmitters. Although it is usually used as an antiepileptic and for chronic pain management, its role for acute postoperative management has also been raised. However, is it not clear if it constitutes an effective alternative in this context.
Methods
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found twenty one systematic reviews [1],[2],[3],[4], |
|
What types of patients were included* |
Sixteen trials included patients undergoing abdominal |
|
What types of interventions were included* |
In all trials oral pregabalin was administered. In forty-nine trials pregabalin was administered during Forty-six trials used a single dose of pregabalin [23], The dose of pregabalin varied between 50 mg and 600 mg. Dexamethasone was coadministered in one trial [51], remifentanil infusion in two trials [58],[69], nonsteroidal anti-inflammatory drugs in two trials [60],[70], acetaminophen in one trial [73], acetaminophen and diclofenac in one trial [55], and in the rest of the trials there was no coadministration of drugs. Regarding postoperative analgesia, acetaminophen with Sixty eight trials compared against placebo [22],[23], |
|
What types of outcomes |
The main outcomes analyzed by the systematic reviews were postoperative pain, sedation, opioid consumption, stay in a postoperative care unit, preoperative anxiety, adverse effects, postoperative nausea and vomiting, and morbidity. The average follow-up of the trials was 24 hours, with a range that fluctuated between 2 and 72 hours postoperatively. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
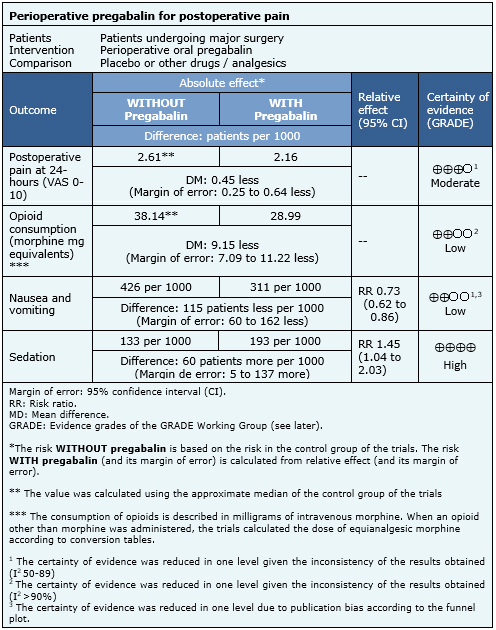
Summary of Findings
The information regarding the effects of perioperative pregabalin is based on 53 randomized trials that include 3543 patients in total [23],[26],[29],[30],[31],[32],[33],[34],[35],[36],[37],[38],[40],[41],[44],[45],[49],[50],[52],[53],[54],[56],[57],[58],[59],[60],[61],[63],[64],[65],[66],[69],[70],[72],[73],[74],[75],[76],[77],[78],[79],[81],[84],[85],[86],[90],[91],[92],[93],[94],[95],[96],[97]. The rest of the trials did not report any of the outcomes of interest or did it in a way that it was not possible to incorporate into a meta-analysis.
Forty-six trials reported the outcome pain at 24 hours after surgery (3037 patients) [23],[26],[30],[31],[32],[33],[34],[35],[36],[37],[38],[40],[41],[44],[45],[49],[50],[53],[54],[56],[57],[58],[59],[60],[61],[63],[64],[66],[69],[70],[72],[73],[75],[76],[77],[78],[81],[85],[86],[90],[91],[92],[93],[94],[96],[97], 27 trials the outcome opioid consumption (1712 patients) [23],[31],[35],[37],[44],[45],[49],[50],[52],[53],[56],[58],[59],[60],[63],[66],[72],[73],[77],[78],[79],[84],[91],[92],[96],[97], 31 trials the outcome nausea and vomiting (2461 patients) [23],[29],[31],[32],[33],[35],[37],[38],[50],[53],[56],[57],[59],[60],[64],[65],[69],[72],[73],[74],[77],[78],[79],[84],[86],[90],[91],[93],[95],[96],[97]; and 18 trials the outcome sedation (1587 patients) [23],[31],[33],[36],[37],[38],[53],[56],[61],[63],[64],[65],[72],[73],[90],[91],[95],[96]. The summary of findings is the following:
- Perioperative pregabalin probably does not produce a clinically significant reduction of acute postoperative pain after major surgeries. The certainty of this evidence is moderate.
- Perioperative pregabalin could decrease postoperative opioid consumption in major surgeries, but the certainty of this evidence is low.
- The use of perioperative pregabalin in major surgeries could decrease the incidence of postoperative nausea and vomiting, but the certainty of this evidence is low.
- Perioperative pregabalin in major surgeries produces an increase in postoperative sedation. The certainty of this evidence is high.

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
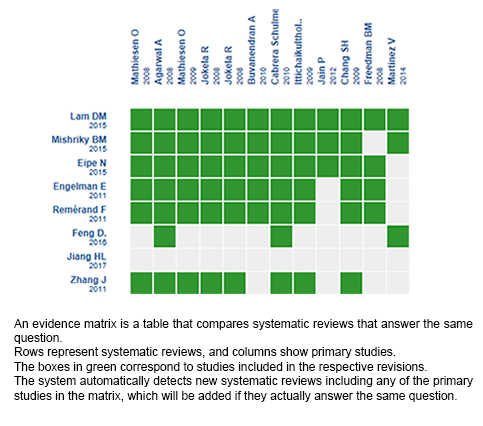
Follow the link to access the interactive version: Perioperative pregabalin for acute postoperative pain in major surgeries
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.

