Epistemonikos summaries
← vista completaPublished on January 30, 2018 | http://doi.org/10.5867/medwave.2018.01.7146
Does adding interbody fusion to posterolateral fusion increase success in the surgical management of degenerative lumbar spondylolisthesis?
¿Es útil agregar una artrodesis intersomática a una artrodesis posterolateral en el tratamiento quirúrgico de la espondilolistesis lumbar degenerativa?
Abstract
INTRODUCTION Surgical treatment of lumbar degenerative spondylolisthesis usually involves an interbody fusion in addition to a posterolateral fusion. However, the value of this procedure has not been established.
METHODS To answer this question we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS We identified four systematic reviews, including nine primary studies; none of them randomized. We concluded performing interbody fusion in addition to posterolateral fusion during the surgical treatment of lumbar degenerative spondylolisthesis might decrease vertebral body slippage and lead to a slight improvement in quality of life. However, it is associated with higher costs.
Problem
Spondylolisthesis corresponds to the slippage of one vertebra over the lower one; degenerative spondylolisthesis is secondary to a degenerative process of the articular facets and the intervertebral disc. Degenerative spondylolisthesis is a cause of lumbar pain, radicular pain, and neurological claudication.
Surgical treatment of degenerative spondylolisthesis aims to reduce pain and to improve function and quality of life by decompressing neural elements. Currently, there is consensus about the need of adding a fusion to the decompression, being the posterolateral fusion, with or without instrumentation, is the most frequently used approach.
The addition of an interbody fusion (IBF), either through an anterior, posterior or transforaminal approach has theoretical benefits since it would increase fusion rate. Moreover, an interbody fusion would stabilize the anterior column, which supports most of the body weight. However, an interbody fusion also carries a higher risk of complications and cost. So, the value of adding an interbody fusion to a posterolateral arthrodesis has not been established.
Methods
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found four systematic reviews [1],[2],[3],[4], including nine primary studies [5],[6],[7],[8],[9],[10],[11],[12],[13]; none of them corresponding to a randomized trial. Two were prospective cohorts [5],[13] and seven were retrospective cohort studies [6],[7],[8],[9],[10],[11],[12]. One study was excluded from the analysis [13] because it compared two types of lumbar interbody fusion. |
|
What types of patients were included* |
All of the studies included patients with lumbar degenerative spondylolisthesis. The average age ranged from 56 to 70 years in the different studies. |
|
What types of interventions were included* |
Regarding the type of intervention, all of the studies added an interbody fusion to a posterolateral arthrodesis. Regarding the type of interbody fusion, five studies used a posterior approach [5],[9],[10],[11],[12] and three used a transforaminal approach [6],[7],[8]. Regarding the comparison, all of the studies compared against posterolateral fusion alone. |
|
What types of outcomes |
The systematic reviews grouped the outcomes as follows:
The average follow-up of the studies was 32 months, with a range of 12 to 53 months. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
● Adding an interbody fusion to the posterolateral fusion during the surgical treatment of degenerative spondylolisthesis might decrease slippage of the vertebral body, and could slightly improve quality of life.
● It is not clear whether adding an interbody fusion improves fusion rate or clinical outcomes such as pain or disability.
Summary of Findings
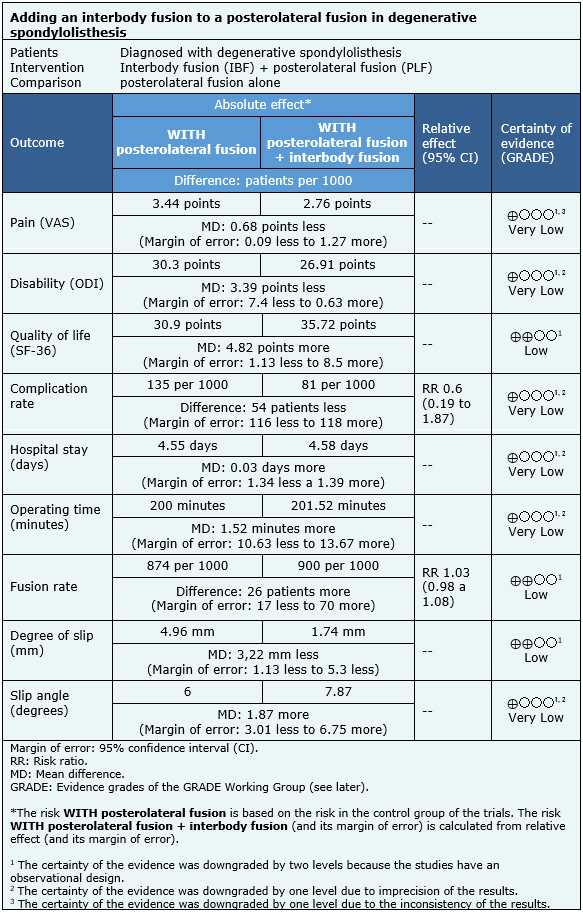
The information on the effects of adding an interbody fusion to a posterolateral fusion in degenerative lumbar spondylolisthesis was based on five studies including 582 patients in total [5],[7],[9],[10],[11].
The remaining three studies [6],[8],[12] were not included in the analysis as none of the identified systematic reviews was able to extract data suitable for meta-analysis from them.
Three studies evaluated pain (277 patients) [7],[9],[10]; three studies assessed disability (277 patients) [7],[9],[10]; three studies determined quality of life (511 patients) [5],[7],[9]; four studies determined complication rate (542 patients) [5],[7],[9],[11]; two studies assessed hospital stay (455 patients) [5],[9]; three studies measured operating time (511 patients), [5],[7],[9]; five studies evaluated fusion rate (521 patients) [5],[7],[9],[10],[11]; two studies measured the degree of slip of the vertebral body (87 patients) [7],[11] and three studies assessed slip angle (127 patients) [7],[10],[11].
The summary of findings is as follows:
- It is not clear whether the addition of an interbody fusion reduces pain, because the certainty of the evidence is very low.
- It is not clear whether the addition of an interbody fusion decreases disability, because the certainty of the evidence is very low.
- It is not clear whether the addition of an interbody fusion reduces complication rates, because the certainty of the evidence is very low.
- It is not clear whether the addition of an interbody fusion decreases hospital stay, because the certainty of the evidence is very low.
- It is not clear whether the addition of an interbody fusion decreases operating time, because the certainty of the evidence is very low.
- It is not clear whether the addition of an interbody fusion decreases slip angle, because the certainty of the evidence is very low.
- The addition of an interbody fusion may produce a slight improvement in quality of life, but the certainty of the evidence is low.
- The addition of an interbody fusion might result in little or no difference in fusion rate, but the certainty of the evidence is low.
- The addition of an interbody fusion might decrease the degree of slip, but the certainty of the evidence is low.

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
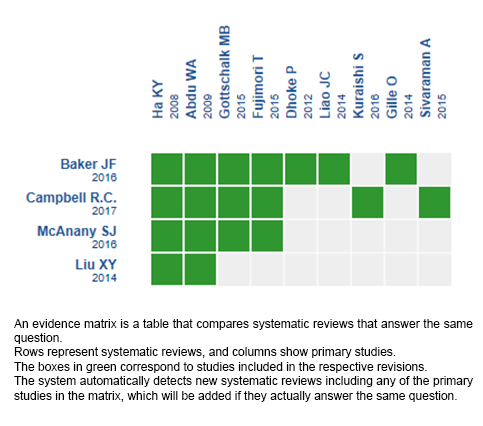
Follow the link to access the interactive version: Posterolateral fusion with or without interbody fusion for lumbar degenerative spondylolisthesis
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.

