Epistemonikos summaries
← vista completaPublished on July 30, 2018 | http://doi.org/10.5867/medwave.2018.04.7233
Are postoperative prophylactic antibiotics effective for orbital fracture?
¿Son efectivos los antibióticos profilácticos postoperatorios en fractura de órbita?
Abstract
INTRODUCTION Infection is one of the main complications of orbital fracture, either because of the connection to the paranasal sinuses or as a postoperative complication. Despite the advances made in this condition, there is still controversy regarding the role of prophylactic antibiotics.
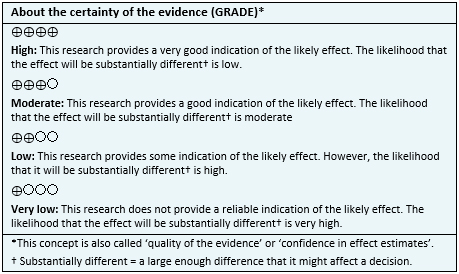
METHODS To answer this question we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS We identified only one systematic review including four studies overall, of which only one was a randomized trial. We concluded that postoperative antibiotic prophylaxis might not decrease the risk of infection in orbital fracture, and probably increases the risk of diarrhea.
Problem
An increase in the incidence of traumatic facial fracture has been reported in the last years, with 30-40% compromising the orbit [1]. While the risk of infection associated to this type of fracture is difficult to determine, it is estimated at less than 1% [2]. Because of the anatomical characteristics of the orbit and its proximity to the paranasal sinuses, the prophylactic use of postoperative antibiotics has been suggested, but it is not clear if they are actually effective.
Methods
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found one systematic review [3] including four studies [4],[5],[6],[7], of which only one corresponded to a randomized trial [4]. This table and the summary in general are based on the latter, since the observational studies did not increase the certainty of the existent evidence nor did they contribute any relevant additional information. |
|
What types of patients were included* |
The trial [4] included patients with orbital blow-out fracture that required surgical intervention and with no need of intensive care; without bacterial infection at the moment of the fracture, bullet wounds, pathological fracture, basilar skull fracture with cerebrospinal fluid rhinorrhoea or intracranial emphysema, history of malignancy or radiation in the head and neck area, known hypersensitivity or allergy to penicillin or other beta-lactam antibiotics, compromised host defense, severe renal insufficiency or lack of compliance. |
|
What types of interventions were included* |
The trial [4] compared the use of intravenous amoxicillin/clavulanic acid 1.2g every eight hours from the time of admission to 24 hours after the surgery, followed by four days of orally administered placebo every eight hours, versus the use of intravenous amoxicillin/clavulanic acid 1.2g every eight hours from the time of admission to 24 hours after the surgery, followed by four days of orally administered amoxicillin/clavulanic acid 625 mg every eight hours for four days. |
|
What types of outcomes |
The outcomes reported by the systematic review were postoperative infections and adverse effects (skin rash and diarrhea). The mean follow-up of the trial was six months [4]. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
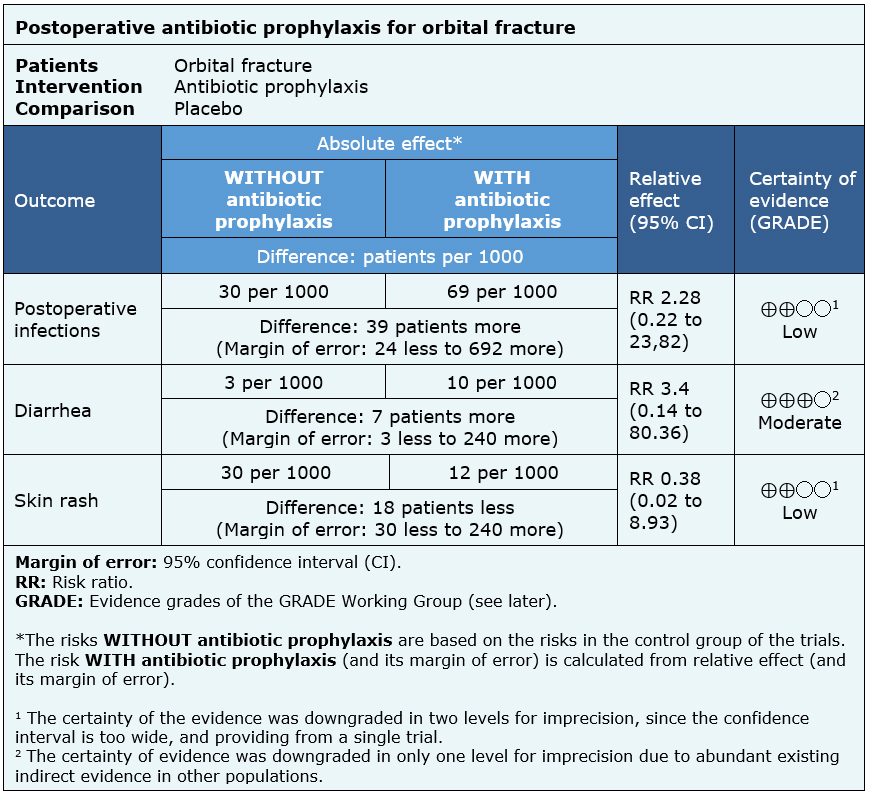
Summary of findings
The information about the effects of postoperative antibiotic prophylaxis in orbital fracture is based on one randomized trial [4] that included 62 patients.
This trial [4] reported the outcomes postoperative infection, diarrhea and skin rash (62 patients).
The summary of findings is the following:
- Postoperative antibiotic prophylaxis might not decrease the risk of infection in orbital fracture, but the certainty of the evidence is low.
- Postoperative antibiotic prophylaxis probably increases the risk of diarrhea. The certainty of the evidence is moderate.
- Postoperative antibiotic prophylaxis might not increase the risk of skin rash, but the certainty of the evidence is low.
Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
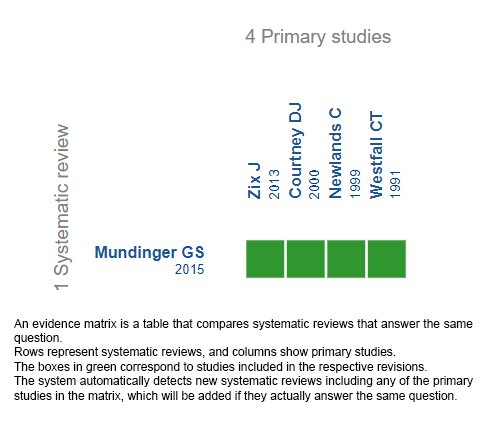
Follow the link to access the interactive version: Prophylactic antibiotics for orbital fractures
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.

