Resúmenes Epistemonikos
← vista completaPublicado el 18 de diciembre de 2018 | http://doi.org/10.5867/medwave.2018.08.7387
Natamicina versus voriconazol para queratitis fúngica
Natamycin versus voriconazole for fungal keratitis
Abstract
INTRODUCTION Infectious keratitis of fungal origin mainly affects people in tropical and subtropical countries, and is an important cause of preventable blindness. Topical antifungals, particularly natamycin and voriconazole, are considered effective, but it is not clear which one is the best treatment alternative.
METHODS We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS We identified three systematic reviews including three studies overall,all of which were randomized trials. We concluded natamycin probably is associated with better visual acuity after infection, and it prevents corneal perforation and/or need to perform therapeutic keratoplasty compared to voriconazole in fungal keratitis.
Problem
Fungal keratitis corresponds to a fungal infection of the cornea, mainly of the epithelium and stroma. The most frequent etiological agents correspond, firstly, to filamentous fungi of the Fusarium, Aspergillus and Curvularia genus, in descending order of frequency and, secondly, to yeasts. In tropical and subtropical countries it constitutes an important cause of preventable blindness, in contrast to what occurs in developed countries, where it scarcely affects the population. The main risk factor corresponds to ocular trauma associated to contamination with plant material, but it has also been associated with the use of corticosteroids, antibiotics, immunosuppressants, chemotherapeutic drugs and ocular prosthetic devices.
There are multiple topical antifungal agents for treatment, such as polyenes (natamycin, amphotericin B), imidazoles (ketoconazole, econazole) and triazoles (fluconazole, posaconazole). The treatment of choice has been for decades topical natamycin, the only antifungal approved by the Food and Drugs Administration (FDA), but the recent emergence of topical voriconazole, a second-generation broad spectrum triazole, has posed new questions, arising thus, the need to evaluate which of these topical antifungals is presented as the best therapeutic alternative.
Methods
We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found three systematic reviews [1], [2], [3] that included three primary studies reported in seven references [4], [5], [6], [7], [8], [9], [10], all corresponding to randomized controlled trials. |
|
What types of patients were included* |
All trials included male and female patients older than 16 years with an average age of 46.7 years, with microbiological evidence of fungal keratitis; direct visualization of hyphae in corneal scraping by smear with 10% KOH stain or Gram stain [5], smear with 10% KOH stain, Giemsa stain or Gram stain [4] and positive corneal ulcer smear for fungi in patients with visual acuity of 20/40 (0.3 logMAR units) at 20/400 (1.3 logMAR units) [8]. All trials excluded patients who had concomitant corneal coinfection (viral, bacterial or protozoal), signs of imminent corneal perforation or history of corneal perforation [4], [5], [8]. Two trials [4], [8] excluded patients with visual acuity worse than 20/200 (1.0 logMAR units) in the unaffected eye and with bilateral ulcers. Two trials excluded patients without light perception in the affected eye [4], [5], and one trial also excluded pregnant patients [4]. |
|
What types of interventions were included* |
All trials used topical 5% natamycin as intervention: two trials administered 1 drop every hour for 1 week and then 1 drop every 2 hours for 2 weeks (while the patient was awake) [4], [8] and one trial 1 drop every hour for 2 weeks [5]. As comparison, topical 1% voriconazole was used: in two trials 1 drop was administered every hour for 1 week and then every 2 hours for 2 weeks (while the patient was awake) [4], [8] and one trial administered 1 drop each hour for 2 weeks [5]. |
|
What types of outcomes |
The trials evaluated multiple outcomes, which were grouped by the systematic reviews as follows:
The average follow-up of the trials was 11.3 weeks, with a range between 10 and 12 weeks. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
Summary of findings
The information about the effects of topical 5% natamycin versus topical 1% voriconazole is based on three randomized trials including 473 patients [5], [6], [8].
One trial reported clinical cure (30 patients) [5], three trials reported changes in visual acuity (logMAR) and corneal perforation and/or need to perform therapeutic keratoplasty (434 patients) [5], [6], [8].
The summary of findings is as follows:
- The use of natamycin in fungal keratitis, compared with voriconazole, might be associated with a higher probability of clinical cure, but the certainty of the evidence is low.
- The use of natamycin in fungal keratitis, compared with voriconazole, probably is associated with better visual acuity. The certainty of the evidence is moderate.
- The use of natamycin in fungal keratitis, compared to voriconazole, prevents corneal perforation and/or need to perform therapeutic keratoplasty. The certainty of the evidence is high.
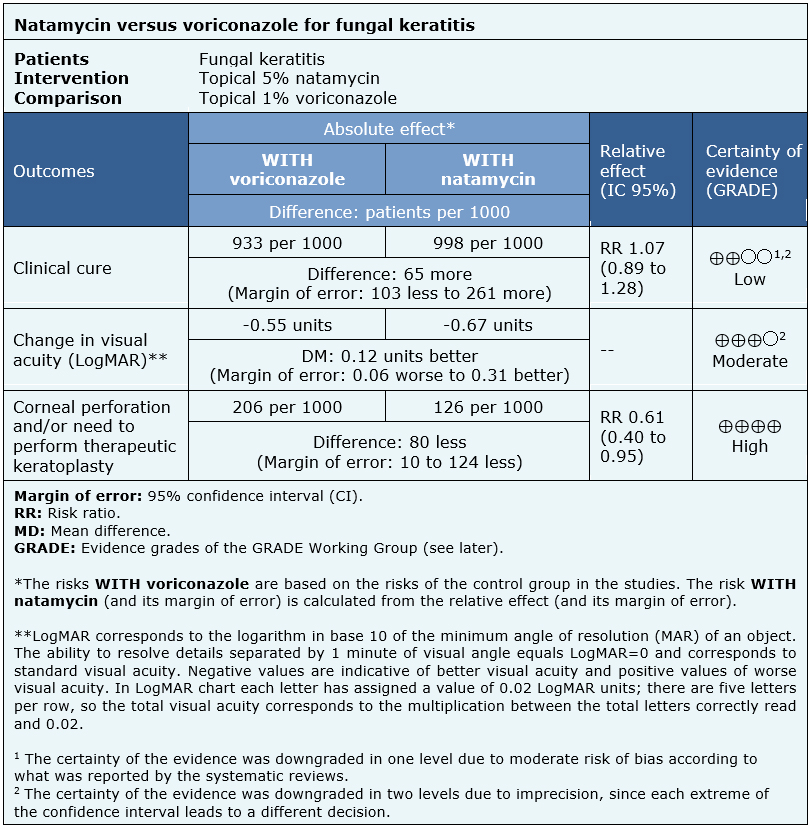
| Follow the link to access the interactive version of this table (Interactive Summary of Findings – iSoF) |

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
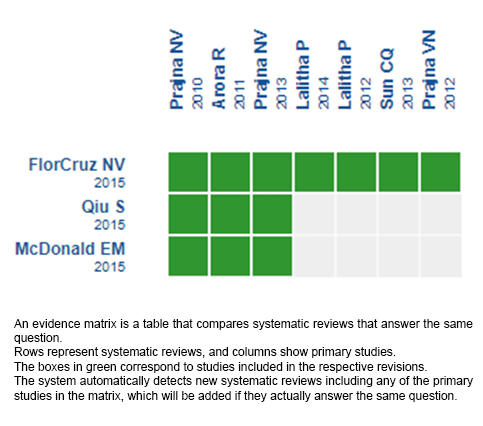
Follow the link to access the interactive version: Natamycin versus voriconazole for fungal keratitis.
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.

