Epistemonikos summaries
← vista completaPublished on November 8, 2019 | http://doi.org/10.5867/medwave.2019.10.7677
B-type natriuretic peptide testing in the emergency setting for managing acute dyspnea
Péptido natriurético tipo B para manejo de disnea aguda en urgencias
Abstract
INTRODUCTION The performance of B-type natriuretic peptide to accurately diagnose dyspnea of cardiac origin has been widely proved. However, its impact in clinical practice is less clear.
METHODS We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS We identified two systematic reviews including five studies overall, of which all were randomized trials. We concluded the use of B-type natriuretic peptide for the management of acute dyspnea in the emergency setting probably leads to a small reduction in the need for hospitalization. Additionally, it may slightly reduce mortality and intensive care unit admission, but the certainty of the evidence is low.
Problem
BNP (brain natriuretic peptide or B-type natriuretic peptide) is a polypeptide, originally found in the brain, which is secreted by ventricular cardiomyocytes in response to the stretching of myocardial fibers due to an increased hydrostatic pressure. Therefore, its levels increase in heart failure, especially when there is a reduced left ventricular ejection fraction. Its function is to promote diuresis and natriuresis, and thus to lower blood pressure. Given its correlation with heart failure, it constitutes a diagnostic method in dyspnea of cardiac origin, with high sensitivity and specificity when used in conjunction with classic methods for the diagnosis of heart failure: symptoms, physical examination, chest radiography and electrocardiogram. However, it is not clear whether the addition of this test to the management of acute dyspnea leads to changes in the clinical decisions that will ultimately translate into benefits for these patients.
Methods
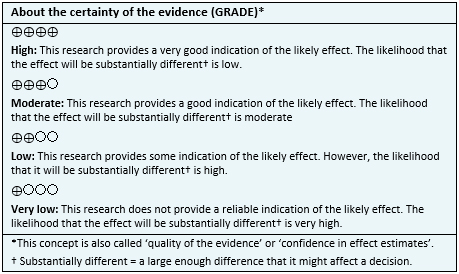
We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found two systematic reviews [1], [2], which included five primary studies [3], [4], [5], [6], [7], all corresponding to randomized controlled trials. |
|
What types of patients were included* |
All trials included patients that presented acute dyspnea in an emergency setting. The mean age ranged from 58 to 74 years across the different trials, with a small predominance of male participants. Three trials [3], [5], [6], reported that 17% to 40% of the patients included had past medical history of heart failure. Four trials [3], [4], [5], [6], reported that 24 to 45% of included patients had chronic obstructive pulmonary disease, and four trials [3], [4], [5], [6], reported past history of tobacco use in 28 to 50% of patients. |
|
What types of interventions were included* |
Three trials evaluated the use of BNP [4], [6], [7] and two trials measured Pro-BNP [3], [5]. All trials compared against routine evaluation, which included general blood exams, electrocardiogram and chest x-rays. |
|
What types of outcomes |
The trials evaluated multiple outcomes, which were grouped by the systematic reviews as follows:
The mean follow up time for the trials was 30 days, with a range from 30 to 60 days. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
Summary of findings
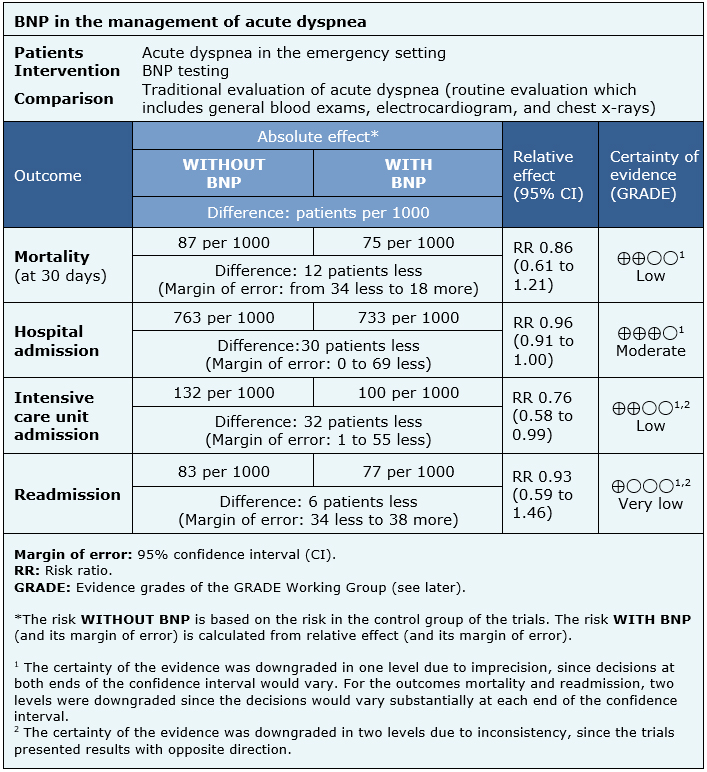
The information on the effects of BNP in the management of acute dyspnea in the emergency setting is based on five randomized trials [3], [4], [5], [6], [7] that included 2488 patients.
All trials reported hospital admissions (2488 patients), three trials evaluated mortality (at 30 days) (1524 patients) and intensive care unit admissions (1541 patients) [4], [5], [6] and two trials evaluated readmission (848 patients) [4], [5].
The summary of findings is as follows:
- The use of BNP in the management of dyspnea in the emergency setting may slightly reduce mortality at 30 days (low certainty of evidence).
- The use of BNP in the management of acute dyspnea in the emergency setting probably slightly reduces hospital admissions (moderate certainty of evidence).
- The use of BNP in the management of acute dyspnea in the emergency setting may slightly reduce intensive care unit admissions (low certainty of evidence).
- We are uncertain whether the use of BNP test in the management of acute dyspnea in the emergency setting has any impact on readmissions as the certainty of the evidence has been assessed as very low.
|
Follow the link to access the interactive version of this table (Interactive Summary of Findings – iSoF) |
Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
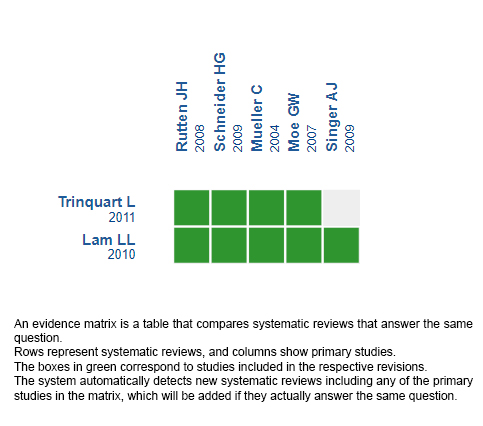
Follow the link to access the interactive version: B-type natriuretic peptide testing for managing acute dyspnea at emergency settings
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.

