Epistemonikos summaries
← vista completaPublished on July 22, 2020 | http://doi.org/10.5867/medwave.2020.06.7964
Pars plana vitrectomy plus scleral buckle versus pars plana vitrec-tomy in pseudophakic retinal detachment
Vitrectomía pars plana asociada a banda de silicona comparada con vitrectomía pars plana para desprendimiento de retina pseudofáquico y afáquico
Abstract
INTRODUCTION Cataract surgery increases the risk for rhegmatogenous retinal detachment. Pars plana vitrectomy and scleral buckling are two surgical procedures used for its repair. The combination of both techniques had been proposed for rhegmatogenous retinal detachment in patients with previous cataract surgery (pseudophakic or aphakic), but its effectiveness remains unclear.
METHODS We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
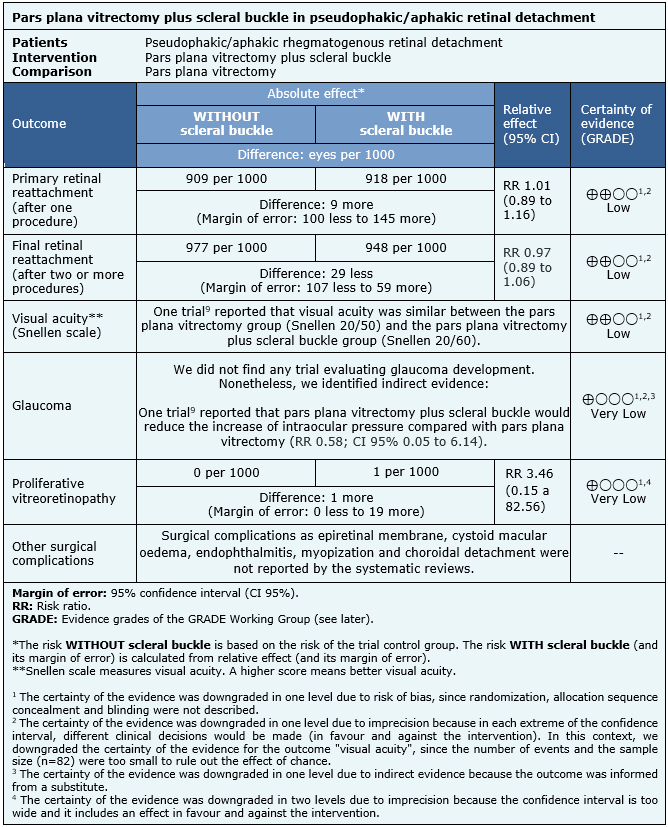
RESULTS AND CONCLUSIONS We identified four systematic reviews with eight studies overall, one of them was a randomized trial. With this data, we conclud-ed that pars plana vitrectomy plus scleral buckle may make little or no difference in primary or final retinal reattachment rate nor in final visual acuity, but the certainty of the evidence is low. In terms of surgery complications, we are uncertain if vitrecto-my plus scleral buckle increases the risk of proliferative vitreoretinopathy or reduces the risk of glaucoma because the certainty of the evidence is very low.
Problem
Rhegmatogenous retinal detachment is defined as the separation of the neurosensory retina from the underlying retinal pigment epithelium. Cataract surgery, an intervention that aims to replace the natural lens by an artificial lens (pseudophakia), could increase the risk of retinal detachment by a factor of seven to eight times [1], [2].
Pars plana vitrectomy and scleral buckle (or encircling band) are two surgical procedures employed to repair retinal detachments. Pars plana vitrectomy consists in the removal of vitreous gel associated with laser and injection of gas or silicone oil to compress the retina. In scleral buckle, the surgeon sutures a silicone implant to the outer surface of the sclera creating an indentation in the wall of the eye to achieve the apposition of the neurosensory retina and retinal pigment epithelium. Finally, the retinal break is repaired with cryotherapy or laser.
Although there is evidence about the effectiveness of these techniques separately in pseudophakic retinal detachments [3], it is not clear whether the combination of scleral buckling with pars plana vitrectomy is superior in patients with an artificial lens (pseudophakic) or patients without an intraocular lens (aphakic).
Methods
We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We identified four systematic reviews [4], [5], [6], [7] including eight primary studies [8],[9],[10],[11],[12],[13],[14],[15], one of which is a randomized control trial [9]. We excluded four studies from the analysis: in three of them [12], [13], [14] the comparison was unclear according to the information provided by the systematic reviews. In one study [15], the population had an additional condition besides retinal detachment. This table and the summary are based on the randomized trial [9] because the observational studies did not increase the certainty of the evidence nor provided additional relevant information. |
|
What types of patients were included* |
All patients included in the randomized trial [9] were pseudophakic with rhegmatogenous retinal detachment and inferior retinal tear. The mean age was 57 years old for the pars plana vitrectomy group and 61 years for the pars plana vitrectomy plus scleral buckle group. Patients had macular detachment (73% of the patients in pars plana vitrectomy group and 63% of the patients in pars plana vitrectomy plus scleral buckle group) and proliferative vitreoretinopathy at grade C or worse (27% of the patients from the pars plana vitrectomy group and 3% of the patients with pars plana vitrectomy plus scleral buckle group). |
|
What types of interventions were included* |
The trial [9] compared pars plana vitrectomy plus scleral buckle with pars plana vitrectomy alone. Laser photocoagulation in 360° and silicone oil instillation were performed in all patients randomized to the pars plana vitrectomy group. The scleral buckle was conducted using a 360° encircling band in the group which received both procedures. The systematic review [6] did not describe the procedure used to perform pars plana vitrectomy and scleral buckle. Neither if laser photocoagulation in 360° was applied nor if instillation of air or gas was used in the pars plana vitrectomy plus scleral buckle group. |
|
What types of outcomes |
The systematic review [6] evaluated multiple outcomes, which were grouped as follows:
|
* Information about primary studies is not extracted directly from primary studies but from identified systematic reviews, unless otherwise stated.
Summary of findings
The information about the outcomes of pars plana vitrectomy plus scleral buckle compared with pars plana vitrectomy in pseudophakic retinal detachment is based in one randomized controlled trial [9] which included 82 pseudophakic eyes.
The trial measured the following outcomes: primary retinal reattachment (retinal reattachment after one procedure) (82 eyes), final retinal reattachment (retinal reattachment after two or more procedures) (82 eyes) and visual acuity in Snellen scale (82 eyes). The latter is reported as a narrative synthesis since none of the systematic reviews provided the necessary information to perform a meta-analysis.
The trial [9] reported complications as proliferative vitreoretinopathy and increased ocular pressure (indirect evidence for the development of glaucoma) (82 eyes). Other surgical complications as epiretinal membrane, cystoid macular oedema, endophthalmitis, myopization and choroidal detachment were not described by the systematic reviews.
The summary of findings is as follows:
- Pars plana vitrectomy plus scleral buckle compared with pars plana vitrectomy may make little or no difference in primary retinal reattachment (low certainty evidence).
- Pars plana vitrectomy plus scleral buckle compared with pars plana vitrectomy may slightly increase final retinal reattachment rate (low certainty evidence).
- Pars plana vitrectomy plus scleral buckle compared with pars plana vitrectomy may make little or no difference to visual acuity (low certainty evidence).
- We are uncertain whether pars plana vitrectomy plus scleral buckle compared with pars plana vitrectomy reduces the risk of glaucoma because the certainty of the evidence has been assessed as very low.
- We are uncertain whether pars plana vitrectomy plus scleral buckle compared with pars plana vitrectomy reduces the risk of proliferative vitreoretinopathy because the certainty of the evidence has been assessed as very low.
- The outcome “other complications of the surgery” was not reported by the evidence included in this article.
| Follow the link to access the interactive version of this table (Interactive Summary of Findings – iSoF) |

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
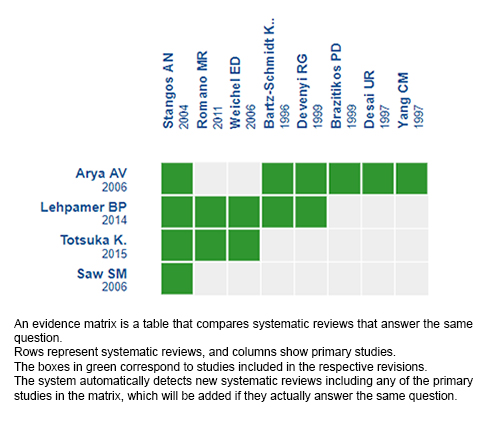
Follow the link to access the interactive version: Pars plana vitrectomy plus scleral buckle versus pars plana vitrectomy in pseudophakic/aphakic retinal detachment.
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.

