Resúmenes Epistemonikos
← vista completaPublicado el 12 de diciembre de 2020 | http://doi.org/10.5867/medwave.2020.11.8071
Profilaxis antibiótica de esquema largo comparado con esquema corto en pacientes sometidos a cirugía ortognática
Long-term antibiotic prophylaxis regimen compared to short-term antibiotic prophylaxis regimen in patients undergoing orthognathic surgery
Abstract
INTRODUCTION Orthognathic surgery, being an invasive surgical procedure, may present significant postoperative morbidities for the patient. Among the most frequently described complications is surgical site infection. The administration of prophylactic antibiotics prior to this type of procedure is a common practice, however, the cost-benefit of the use of antibiotics, the type of antibiotics, the route of administration, the dosage, and the regimen to be used have not been clearly defined and are still considered a controversial issue. In this summary of evidence, we will compare long-term antibiotic prophylaxis with short-term prophylaxis.
METHODS We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS We identified five systematic reviews including nine studies overall, of which all nine were randomized trials. We conclude that administering a long-term prophylactic antibiotic regimen probably decreases the risk of surgical site infection and that it may increase the risk of hospital stay longer than two days, nevertheless, regarding this last point, the certainty of the evidence is low.
Problem
Orthognathic surgery corresponds to a set of surgical techniques that allow the correction of the anomalies of the maxillofacial complex through the realignment of the maxillary and mandibular bones; allowing the improvement of the functionality, facial harmony, and aesthetics. Some of the postoperative complications include hemorrhage, temporary or permanent neurological alterations and infections. In relation to this last complication, the use of antibiotic prophylaxis is frequent, and is defined as the use of antibiotics to prevent infection at the surgical site [1]. However, there is no clear consensus regarding the type of antibiotic, dose, route of administration or regimen to use.
Additionally, prophylactic antibiotic schedules can be classified according to the time of administration:
- Preoperative prophylaxis: a single dose before surgery.
- Short-term prophylactic antibiotic regimen: begins with pre-surgical doses and is maintained for and/or up to 24 hours after surgery.
- Long-term prophylactic antibiotic regimen: starts with pre-surgical doses and is maintained for and beyond 24 hours after surgery [1].
In this summary of evidence, the long-term and short-term prophylactic antibiotic regimen will be comparatively evaluated, with the intention of clarifying which of these would be more effective in reducing postoperative complications.
Methods
We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We identified five systematic reviews [1], [2], [3], [4], [5] including nine studies overall [6], [7], [8], [9], [10], [11], [12], [13], [14], of which all were randomized trials. |
|
What types of patients were included* |
All trials included patients that underwent orthognathic surgery, without distinction in the subtype of surgery. The trials included men and women with ages ranging from 15 to 48 years [6], [7], [8], [9], [10], [11], [12], [13], [14]. |
|
What types of interventions were included* |
All trials evaluated long antibiotic prophylaxis regimens compared with short prophylaxis regimens. Long-term prophylactic regimens considered administration of antibiotics before the operation, on the day of the surgery, and for several additional postoperative days: two days [7], [13],12 three days 12], five days [6], [11], seven days [10], [14]. This information was not reported in two trials [8], [9]. Short-term prophylactic antibiotic regimens considered preoperative and during the same day (up to 24 hrs.) antibiotic administration [6], [7], [8], [9], [10], [11], [12], [13], [14]. Three trials used placebo within the regimen [6], [7], [13]. The antibiotics used by each trial were:
The routes of drug administration used were Two trials did not report the regimen, antibiotic or route of administration used [8], [9]. |
|
What types of outcomes |
The trials evaluated multiple outcomes, which were grouped by the systematic reviews as follows:
|
* Information about primary studies is not extracted directly from primary studies but from identified systematic reviews, unless otherwise stated.
Summary of findings
The information on the effects of antibiotic prophylaxis in a long-term regimen is based on nine randomized trials [6], [7], [8], [9], [10], [11], [12], [13], [14], involving 472 patients.Nine trials measured the outcome surgical site infection [6], [7], [8], [9], [10], [11], [12], [13], [14] (472 patients) and only one trial measured the outcome hospital stay longer than two days (171 patients) [8].
The summary of findings is as follows:
- The use of a long-term prophylactic antibiotic regimen compared with a short-term prophylactic antibiotic regimen probably decreases the risk of surgical site infection (moderate certainty of evidence).
- The use of a long-term prophylactic antibiotic regimen compared to a short-term prophylactic antibiotic regimen may increase the risk of hospital stay longer than two days (low certainty of evidence).
- No studies were found that looked at adverse effects.
- No studies were found that looked at mortality.
- No studies were found that looked at systemic infection.
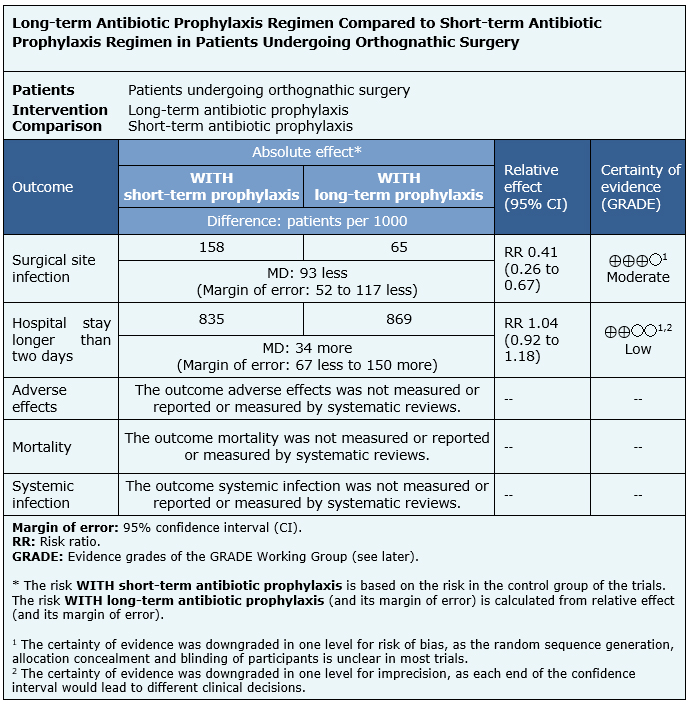
| Follow the link to access the interactive version of this table (Interactive Summary of Findings – iSoF) |

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
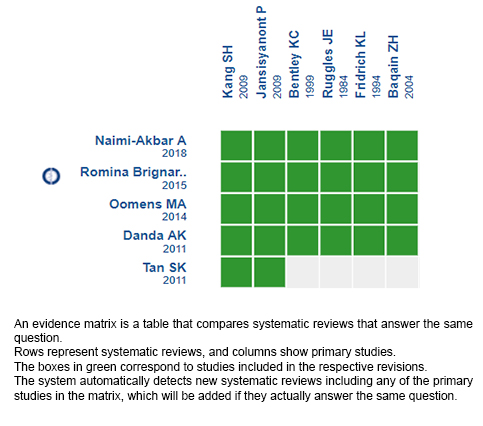
Follow the link to access the interactive version: Long-term antibiotic prophylaxis regimen compared to short-term antibiotic prophylaxis regimen in patients undergoing orthognathic surgery.
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.

