Resúmenes Epistemonikos
← vista completaPublicado el 23 de diciembre de 2021 | http://doi.org/10.5867/medwave.2021.11.8184
Radiocirugía para oligometástasis cerebral en cáncer de pulmón.
Radiosurgery for brain oligometastases in lung cancer.
Abstract
INTRODUCTION Brain metastases are a common problem in oncology patients, especially in lung cancer. The usual treatment for cerebral oligometastases is whole brain radiation therapy. Given the persistent poor prognosis of this disease, other therapeutic alternatives such as stereotactic radiosurgery have been considered. However, there is no clarity regarding the effectiveness of its addition.
METHODS We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS We identified 17 systematic reviews including seven studies overall, of which four were randomized trials. All trials assessed patients with brain oligometastases, but none of them included exclusively lung cancer population. We concluded that it is not possible to clearly establish whether radiosurgery decreases neurological functionality, cognitive impairment, mortality or serious adverse effects, as the certainty of the existing evidence has been assessed as very low.
Problem
Brain oligometastases are a common problem in oncology patients. It is usually defined by a limited number of metastases (less than five), placing it as an intermediate state between localized and metastatic cancer. This stage is associated with better prognosis, since it is possible to administer local treatment in addition to the systemic treatment of the disease. Within the histological origins we can find breast, kidney and colon cancer, among others, being the most frequent lung cancer.
The usual local treatment for cerebral oligometastases is the use of corticoids or whole brain radiotherapy and it is estimated that survival could vary between two and six months [1]. Given the persistent poor prognosis of this disease, other therapeutic alternatives such as stereotactic radiosurgery has been proposed, which allows the administration of higher doses of radiation in a localized area and may be more effective in the ablation of brain metastases. However, its indication is controversial, as it is not clear how effective can be its addition to systemic treatment or whole brain radiotherapy.
Methods
We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We identified 17 systematic reviews [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], including seven studies overall reported in eight references [19], [20], [21], [22], [23], [24], [25], [26], of which four were randomized trials reported in five references [19], [20], [21], [22], [26]. The table and summary are based on the randomized trials, as the observational studies did not increase the level of certainty of the evidence, nor added any additional relevant information. |
|
What types of patients were included* |
All trials included patients with a diagnosis of cerebral oligometastases, regardless of their primary histology. Only two trials reported the number of patients with primary lung cancer: in one trial it was 64% [19] and in another 44% [20]. Three trials included patients with one to three brain metastases [19], [21], [22], and one trial with two to four brain metastases [20]. Three trials excluded patients with a functionality below 70 points on the Karnofsky scale [19], [20], [21]. |
|
What types of interventions were included* |
All trials evaluated the addition of stereotactic radiosurgery to whole brain radiotherapy in comparison with whole brain radiotherapy alone. Regarding the doses used in the intervention, one trial reported that stereotactic radiosurgery was administered with doses between 14 to 20 Gy (average 14.6 Gy) [21]; one applied 20 Gy [22], another a 16 Gy dose [20], and one trial did not report the dose administered [19]. Only one trial specified the type of radiosurgery (Gamma knife) [22]. Regarding the comparison, three trials administered 30 Gy for the whole brain radiotherapy in 10 sessions [20], [21], [22]. One trial administered 37.5 Gy with a daily dose of 2.5 Gy [19]. |
|
What types of outcomes |
The trials evaluated multiple outcomes, which were grouped by the systematic reviews as follows:
The average follow-up of the trials was not reported. However, outcomes had a follow-up with a range between 3 to 18 months [19], [20], [21], [22]. |
*Information about primary studies is not extracted directly from primary studies but from identified systematic reviews, unless otherwise stated.
Summary of findings
Information on the effects of stereotactic radiosurgery on brain oligometastases in lung cancer is based on four randomized trials involving 596 patients [19], [20], [21].
Two trials evaluated mortality (358 patients) [19], [20]. One trial evaluated the outcome neurological functionality (42 patients) [21]. One trial evaluated the outcomes cognitive deterioration (154 patients) [19] and acute and late serious adverse effects (326 patients) [19]. None of the systematic reviews reported the outcome quality of life.
The summary of findings is as follows:
- We are uncertain whether the addition of stereotactic radiosurgery reduces mortality as the certainty of the evidence has been assessed as very low.
- We are uncertain whether the addition of stereotactic radiosurgery reduces the deterioration of neurological functionality as the certainty of the evidence has been assessed as very low.
- We are uncertain whether the addition of stereotactic radiosurgery reduces cognitive deterioration as the certainty of the evidence has been assessed as very low.
- We are uncertain whether the addition of stereotactic radiosurgery reduces late serious adverse effects as the certainty of the evidence has been assessed as very low.
- We are uncertain whether the addition of stereotactic radiosurgery reduces acute serious adverse effects as the certainty of the evidence has been assessed as very low.
- No studies were found that looked at quality of life.
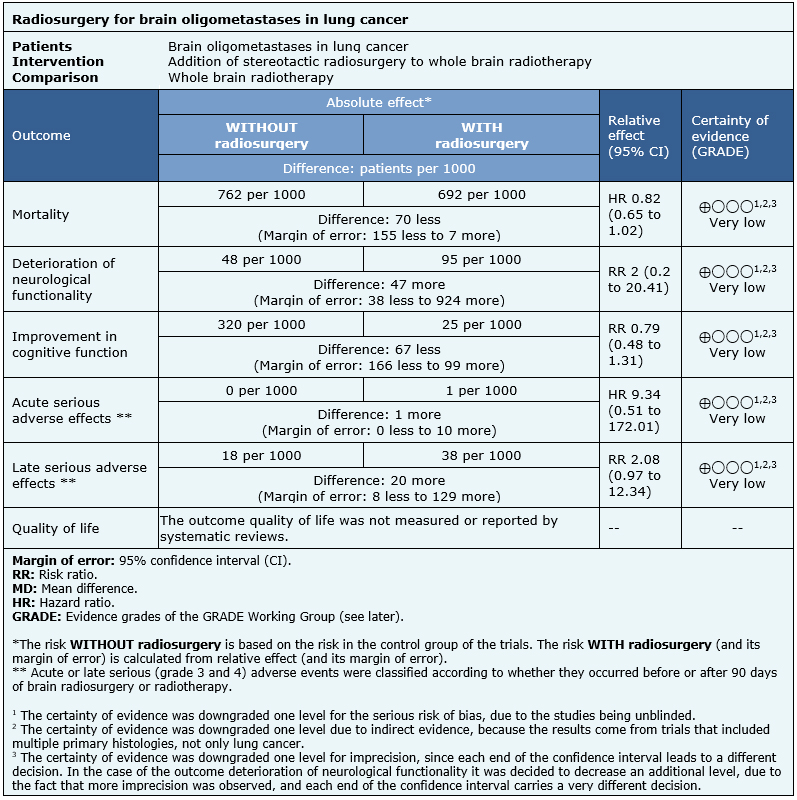
| Follow the link to access the interactive version of this table (Interactive Summary of Findings – iSoF) |
Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
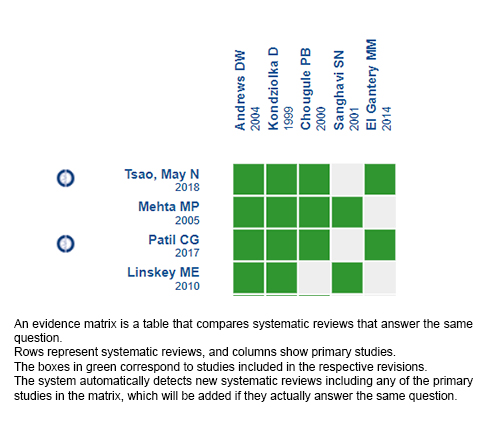
Follow the link to access the interactive version: Addition of radiosurgery to whole brain radiotherapy or systemic therapy for the treatment of brain oligometastases.
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.

