Análisis
← vista completaPublicado el 21 de agosto de 2024 | http://doi.org/10.5867/medwave.2024.07.2929
Epidemiología del trauma de alta energía en Chile: análisis ecológico con registros públicos
Epidemiology of high-energy trauma in Chile: An ecological analysis using public registries
Abstract
High-energy trauma is defined as severe organic injuries resulting from events that generate a large amount of kinetic, electrical, or thermal energy. It represents a significant public health concern, accounting for 10% of global mortality. This article aims to describe the epidemiology of high-energy trauma in Chile. Specifically, it seeks to compare the mortality rate per 100 000 inhabitants among member countries of the World Health Organization (WHO), provide a descriptive analysis of notifications under the Explicit Health Guarantees (GES) for the health issue of polytraumatized patients, and analyze the trend in the mortality rate due to external causes in Chile. This study employs an ecological design using three open-access databases. First, the WHO database on deaths from traffic accidents in 2019 was used. Then, the GES database was consulted for the "Polytraumatized" issue between 2018 and 2022. Finally, the Chilean Department of Health Statistics database on causes of death between 1997 and 2020 was utilized. In 2019, Chile ranked in the middle regarding the mortality rate per 100 000 inhabitants due to traffic accidents. GES notifications for polytrauma predominantly involved men aged 20 to 40 years and those affiliated with the public health system, highlighting a primary focus for prevention efforts. Mortality from accidents showed a decreasing trend, with significant structural changes identified in 2000 and 2007.
Main messages
- Morbidity and mortality linked to injuries in the context of high-energy trauma are a major challenge for health institutions and public health worldwide. It is estimated that high-energy trauma generates 255 million disability-adjusted life years annually.
- The most affected population is men of working age under 65 years and it is one of the leading causes of death in adults under 45 years.
- This study contributes a robust initial analysis to generate hypotheses to demonstrate measures to improve high-energy trauma indicators, leading to public policies that impact on the indicators.
- Among the limitations of the study is that there is no single indicator for high-energy trauma, which makes comparison with other publications difficult.
Introduction
High-energy trauma is defined as severe organic injuries resulting from events that generate a large amount of kinetic, electrical, or thermal energy [1]. Morbidity and mortality related to injuries in the context of high-energy trauma are a major challenge for healthcare institutions and public health worldwide [2,3], accounting for 16% of the burden of disease, 10% of global mortality, and an expenditure of 1 to 3% of gross domestic product [4,5].
High-energy trauma falls into two main categories: voluntary and involuntary. Acts of suicide, homicide, and injuries resulting from military conflicts are often grouped within the causes categorized as voluntary. In contrast, road traffic accidents, firearm injuries, poisoning, and drowning are considered involuntary. Among the most documented aetiologies are falls, motor vehicle accidents, and injuries caused by ballistic projectiles [6]. The most affected population are men under 65, i.e., of active working age. Specifically, it is one of the leading causes of death in adults under the age of 45 [7]. However, some studies report an increase in the average age in this pathology, which is associated with an increase in comorbidities [2]. On the other hand, male patients consult more frequently, present with more severe cases, and have a higher mortality rate in high-energy trauma [2].
High-energy trauma comprehensively affects patients' health [8]. In addition to the organic injuries it causes and its potential sequelae, it is essential to consider the psychological impact on both the patient and their environment, representing an additional challenge [9]. The economic dimension is also affected because of the costs associated with treatment, which often includes several interventions and prolonged rehabilitation, and because of the impact on the individual’s employment and close environment [10]. It has been estimated that high-energy trauma generates 255 million disability-adjusted life-years of disability annually [5].
The burden of high-energy trauma injuries, especially from road traffic crashes, has been steadily increasing in low- and middle-income countries, including Chile, necessitating a deeper understanding of epidemiological patterns and underlying factors [11]. It is imperative to implement effective prevention strategies and improve healthcare systems in order to reduce both the economic impact and the physical and social consequences of high-energy trauma.
The organization of the health care network is crucial to improve outcomes in treating high-energy trauma. This has been studied in Canada, where implementing four high-complexity centers, followed by secondary and tertiary stabilization centers, has significantly impacted high-energy injury mortality [12].
In 1993, Chile created the National Traffic Safety Commission (CONASET), a governmental entity responsible for creating and implementing public policies to prevent traffic accidents. Among the most important measures are the creation of the role of professional driver in 1997, safety requirements for cars in 2000 and for motorbikes in 2001, the regulation of the braking system in 2006, the Zero Tolerance Law for alcohol consumption by drivers in 2012, the compulsory use of airbags in 2015 and child restraint systems in 2017, among other measures. Along the same lines, in Chile, workers' mutual insurance companies are responsible for risk prevention and treating occupational accidents. Every hired worker must have insurance that covers the employer’s costs for the care and follow-up of accidents occurring at work. On the other hand, the Explicit Health Guarantees Law (GES) is the most essential health legislation in Chile in this century and provides guarantees of timely access, quality, and financial protection for the treatment of a limited number of pathologies, currently 87. In 2007, health problem No. 48 was integrated, called ’severe polytraumatized', which includes any patient admitted through the emergency service due to a high-energy trauma pathology.
The health care system in Chile is mixed. Residents in Chile can opt for either private or public insurance. Private insurance is known as 'Instituciones de Salud Previsional' (ISAPREs), while public insurance is the only one of its kind, Fondo Nacional de Salud (FONASA). The latter is divided into four brackets according to the insured’s income and the size of his or her family group. The 'A' bracket is for those with no resources; the 'B' bracket for those with a monthly income of less than 400 000 Chilean pesos (CLP, approximately USD 439 at the time of writing); the 'C' bracket for those with a monthly income of less than 584 000 CLP (approximately USD 641) and with fewer than three dependents; and the 'D' bracket for those with a monthly income of more than 584 000 CLP.
Beneficiaries of the National Health Fund are mostly treated in public network institutions, although they can also access private institutions under particular modalities or at their own cost. On the other hand, the 'Instituciones de Salud Previsional' beneficiaries are mainly treated in private centres and, exceptionally, in public institutions when the required complexity is unavailable. This tends to be the case in the extreme regions of the country. Levels of complexity organize the public network of health institutions. However, only one centre dedicated exclusively to trauma is located in the Metropolitan Region, the Hospital de Urgencia de la Asistencia Pública.
In order to properly implement and evaluate public policies, it is essential to carry out an accurate diagnosis of the current situation of the health problem [13]. In the case of high-energy trauma, unfortunately, there is no single indicator, as it is generally limited to the description of motor vehicle accidents or falls from height [14]. Knowing these limitations, we set out to conduct an analysis using various sources to detail and study the trends in incidence and mortality of high-energy trauma in Chile and to compare them with situations in other countries. The objective of the present study is to describe the epidemiology of high-energy trauma in Chile. The first specific objective is to compare the number of deaths per 100,000 inhabitants in 2019 among WHO countries and to identify associated risk factors. Secondly, the specific objective is to report the number of notifications of Explicit Health Guarantees made between 2018 and 2022, describing age, gender, and geographical location. Finally, the third specific objective is to report the number of deaths associated with external causes between 1997 and 2020 in Chile and to identify whether there has been a significant change in the period studied.
Methods
We conducted an ecological study sourced from open databases, which was exempted from ethics committee approval. Three databases were analyzed. First, we used the World Health Organization’s open database,
Secondly, a request was made via the Transparency Portal to the Superintendence of Health and the National Health Fund to send open data on age, gender, cause, type of accident, type of health insurance, care institution, diagnoses, outcome, and hospital stay of all those patients notified for health problem number 48 - severe polytraumatization - of the Explicit Health Guarantees between 2018 and 2022. Both entities responded by sending only gender, age, type of insurance, and health institution where the patient was treated. A one-way analysis of variance test by ranks (Kruskal-Wallis test) was used to determine whether there were significant changes in age during the period studied. If significance was found (p < 0.05), post hoc comparisons were performed, adjusting for reference and significance. For categorical variables, such as sex and patient prognosis, the Chi-square test was used. If significant differences were found (p < 0.05), a regression model was estimated for longitudinal data, and comparisons were made between each year post-estimation using contrast tests.
Finally, the Chilean Department of Health Statistics (DEIS) mortality database, including patients who died in Chile from 1997 to 2020, was analyzed. This database is open-access and available at
The Stata V.17 statistical program was used for the analysis, and 0.05 was used for significance.
Analysis
Chile compared with the rest of the world in 2019
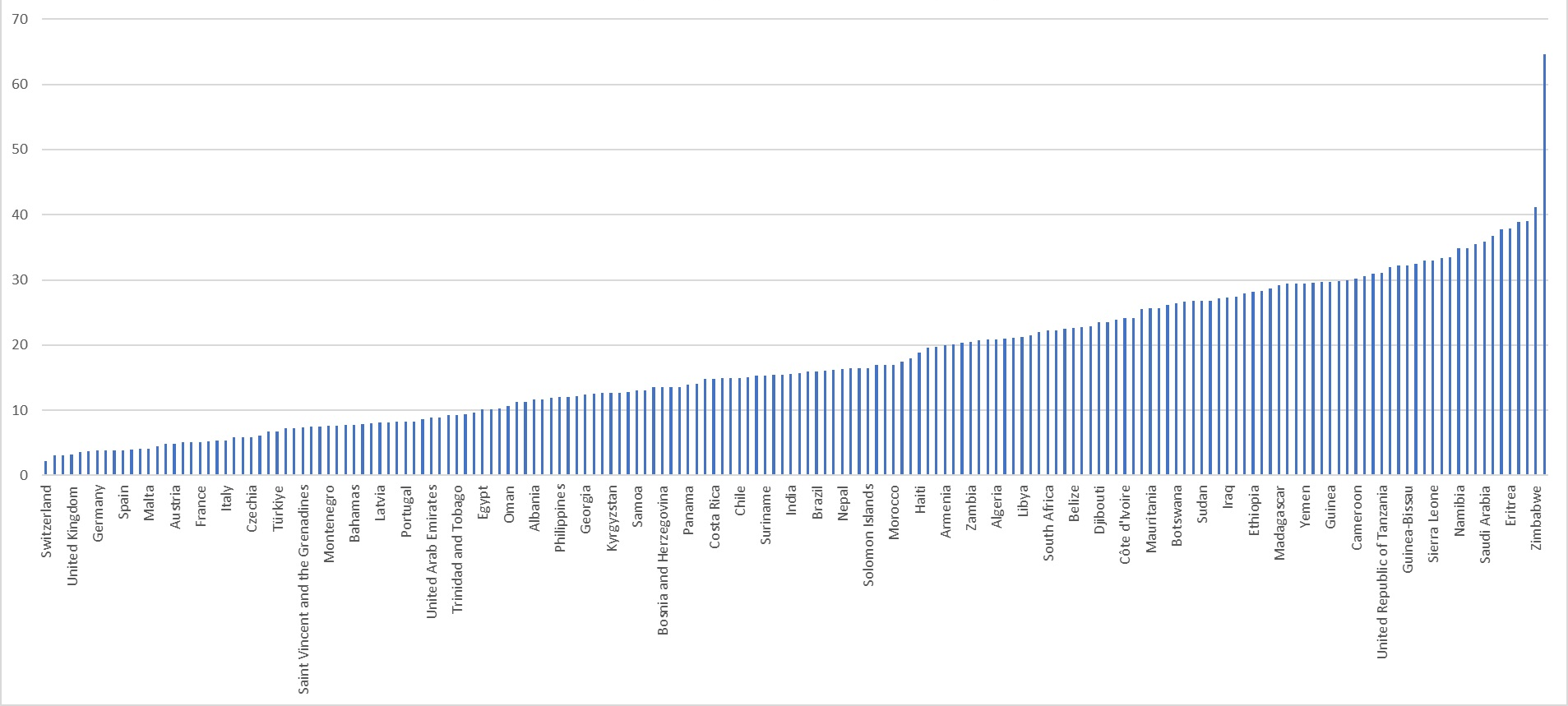
According to the WHO, Chile had a motor vehicle fatality rate of 14.9 per 100 000 inhabitants, ranking 82nd out of 176 countries included in the database. The country with the lowest rate is Switzerland, with 2.2, and the country with the highest rate is the Dominican Republic, with 64.6 deaths per 100 000 inhabitants. Among South American countries, Chile ranks fourth, behind Peru (13.6), Argentina (14.1), Uruguay (14.8) and ahead of Colombia (15.4), Brazil (16.0), Ecuador (20.1), Bolivia (21.1) and Paraguay (22.0) (Figure 1).
Death rate per 100 000 people in countries belonging to the World Health Organization (WHO).
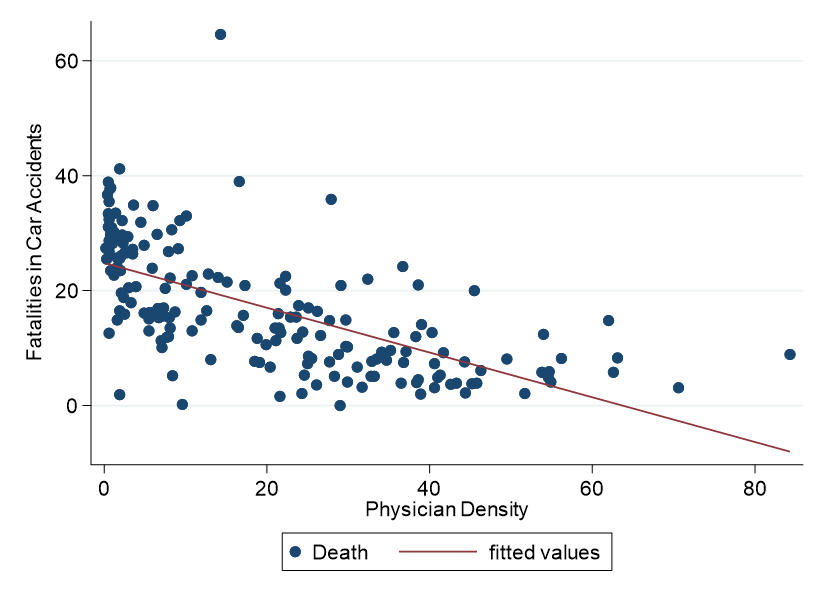
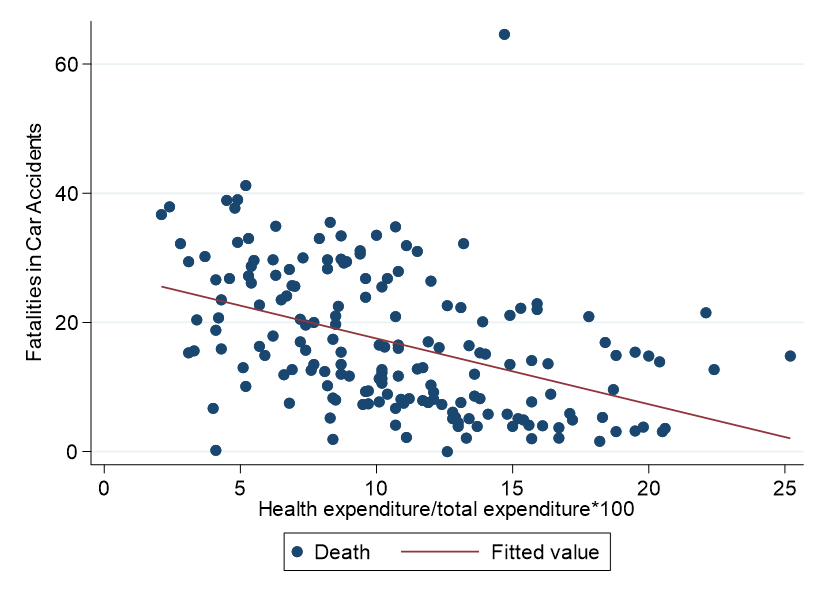
The analysis shows a significant association with physician density, with an R2 of 0.40, β1 = 0.4 (p < 0.000), and a constant of 24 (p < 0.000) (Figure 2). The ratio of health expenditure to total expenditure in each country also has a significant relationship, but with a lower R2 (0.20), reporting a β1 of -1.01 (p < 0.000) and a constant of 27.0 (p < 0.000) (Figure 3). No significant relationship was found with investment in health research.
Relationship of physician density and death rate in 2019 per 100 000 population in WHO countries.
Ratio of health expenditure to total expenditure by country and death rate in 2019 per 100 000 population in WHO countries.
Notifications of explicit health guarantees for polytrauma from 2018 to 2022
During the five years included in this database, 10 647 notifications were found, with a mean age of 38.8 years (± 18.8), of which 8338 (78.3%) were in male patients. 2022 had the highest number of notifications (n = 2187), while 2018 had the lowest number (n = 2040), with an annual mean of 2190 notifications.
The distribution by age group was 1235 (11.6%) in patients older than 65 years, 586 (5.5%) in patients younger than 15 years, and 8826 (82.9%) in patients between 15 and 64 years. In the 15 to 64 age group, 4884 (55.3%) reported patients aged 20 to 40. When performing a Kruskall-Wallis test, a significant difference is observed (p = 0.0028), showing in the subsequent analysis, only significant between 2018 and 2020 (p = 0.0021) and between 2020 and 2022 (p = 0.000204; supplementary file, Table 1). This difference does not show a trend, as in 2018, patients were less young than in 2020, while in 2020, they were younger than in 2022 (Table 1). The proportion of females per year did not vary significantly over the period studied (Chi-square, p = 0.059), with the lowest proportion being 18.1% in 2020 and the highest 19.3% in 2018.
Regarding forecasting, 71 cases per 100 000 National Health Fund affiliates are estimated, while four cases per 100 000 private health insurance affiliates are estimated. The proportion of patients affiliated to the National Health Fund reported has been steadily increasing from 2018 (92.2%) to 2022 (95.6%), with a significant change between years (Chi-square, p = 0.059). Estimating the logit model for longitudinal data (supplementary file, Table 2) shows a significant increase over the period studied, with comparisons between 2018 and the period from 2020 to 2022, between 2019 and 2021 to 2022, between 2020 and 2021 and 2022; and between 2021 and 2022 being significant.
The national rate of reported patients is 11.37 cases per 100 000 population. The regions of Tarapacá, O'Higgins, Biobío), Los Lagos, Metropolitan, and Los Ríos are above the national rate (Table 2).
Trauma-related deaths in Chile from 1997 to 2020
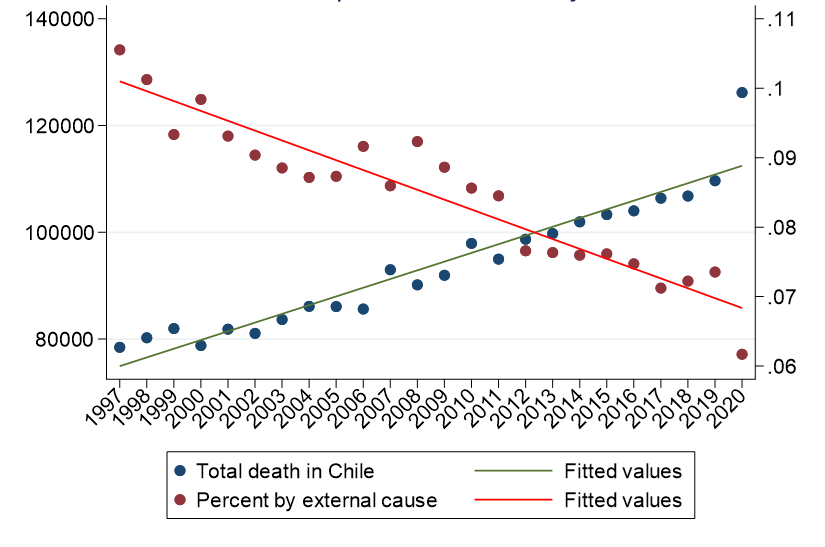
A total of 2 248 881 people died in the period 1997 to 2020, of which 187 632 were due to trauma or external causes (8%). This was the fourth leading cause of death overall, after those linked to the cardiovascular system (27%), tumors (25%), and the respiratory system (10%). However, the proportion of deaths decreased over the studied period (Figure 4).
Comparison of total deaths and percentage associated with external causes between 1997 and 2020.
Segregating by specific causes, 115 007 deaths were identified (61%). The most frequent diagnosis was traumatic brain injury 36 606 (31.8%), followed by multiple trauma 23 348 (20.3%) and femur fracture 10 050 (8.74%). In terms of causes, pedestrian traffic accidents were the leading cause with 20 629 (17.9%), followed by falls 16 651 cases (14.5%), assaults 16 389 (14.3%), and other traffic accidents with 16 116 (14.0%). Regarding the place of death, 61 278 (46.7%) were classified as 'other', 41 333 (35.9%) occurred in a health center, and 12 396 (10.8%) at home.
Analysis by time series shows an average rate of 2.31 cases per month per 100 000 people, with the maximum in February 2010, the only month in which the rate exceeds 3.5 cases (Figure 5).
Number of deaths per 100 000 population between 1997 and 2020.
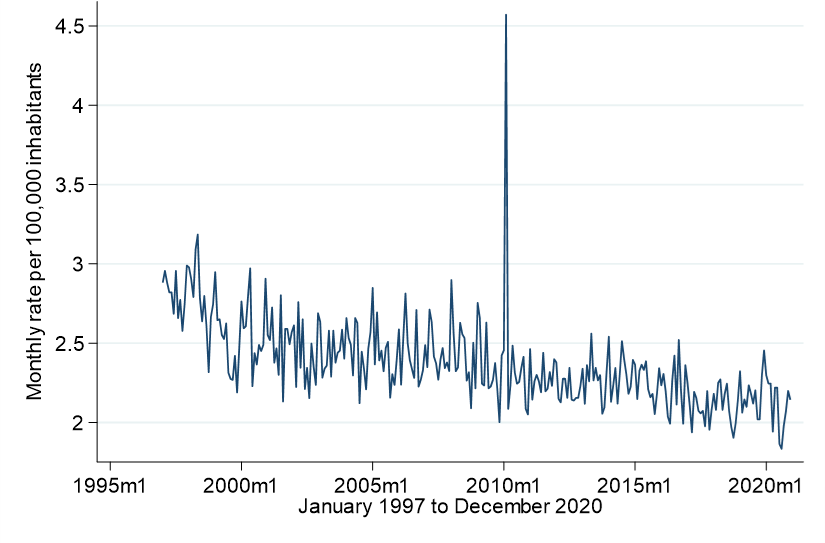
The trend is decreasing, with an R2 of 0.51 and β1 of -0.0002 (p < 0.000) and a constant of 3.6 (p < 0.000). However, the heteroscedasticity of the model is significant (p > 0.000), violating the principles of the linear regression model. Applying a Markov switching model, a significant structural change in the time trend is observed for November 2000 (p = 0.000). On the other hand, when plotting by time series the rate of monthly deaths occurring in health facilities and then applying a Markov switching model, it is observed that it is significant (p < 0.000). Here, August 2007 is identified as the break point (Figures 6 and 7).
Cumulative hospital deaths between 1997 and 2020 with a 95% confidence interval.
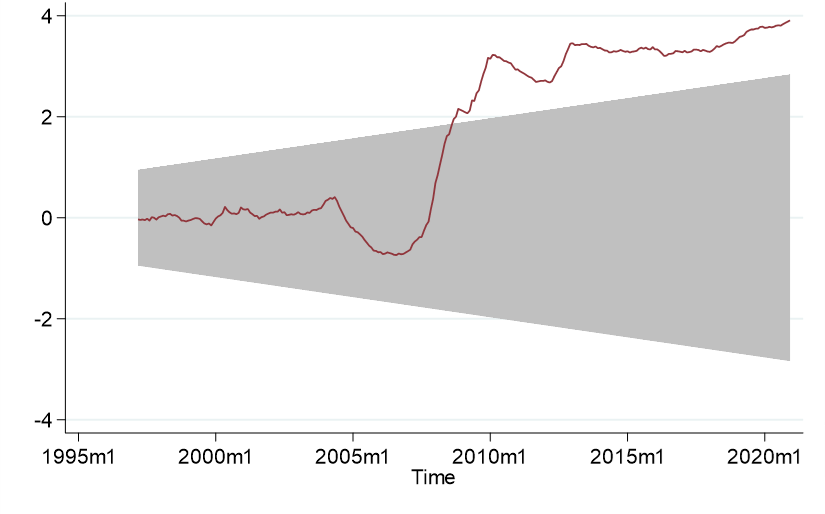
Source: Prepared by the authors based on the results of the study.
In-hospital mortality from high-energy trauma in Chile between 1997 and 2020.
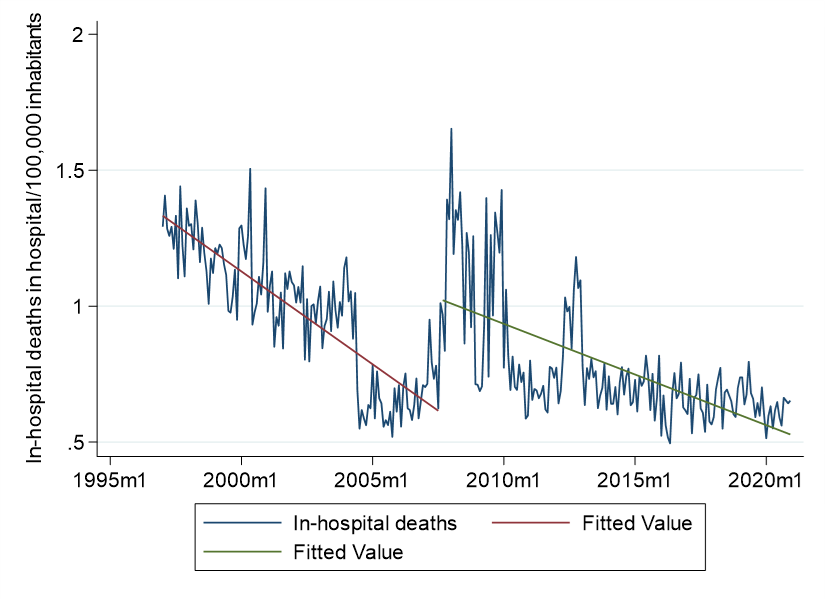
Source: Prepared by the authors based on the results of the study.
Discussion
In this study, we conducted a comprehensive analysis using three databases to describe high-energy trauma in Chile. We used mortality from motor vehicle accidents to compare the national context with other countries through notifications from the Explicit Health Guarantees system to determine the incidence and deaths from trauma to evaluate the results and impact of public policies. However, it is essential to note that in high-energy trauma, there is no universal indicator due to the diversity of injuries that occur, different causes, and asynchronous outcomes [14].
Mortality secondary to motor vehicle accidents reported by the WHO is an important indicator to understand the impact of high-energy trauma and to compare the situation in Chile with other countries. During 2019, the mortality rate due to motor vehicle accidents in Chile was 14.9 per 100 000 inhabitants, ranking fourth in South America. This indicator is inversely associated with the country’s economic power, physician density, and the ratio of health spending to the country’s total expenditure. Several studies have explored economic power and road traffic mortality, finding an inverse relationship between per capita income or income level and road traffic mortality [15,16]. Other factors, such as the employability rate and the proportion of alcohol consumption in the region, have also been identified as influencing road traffic mortality [17]. Our study observed a significant association between physician density and trauma mortality, highlighting the importance of considering this factor, especially given that physician density varies considerably between different regions in Chile [18]. However, it is essential to note that although it identified significant findings, this analysis has moderate R2. This suggests that unanalyzed variables such as road safety measures and vehicle characteristics could explain mortality.
Concerning the notifications of Explicit Health Guarantees for severe polytraumatization, we observed that the highest volume of notifications corresponds to male patients affiliated with the public health insurance system. Higher male prevalence has been consistently found in other regions of the world, including Europe, Asia, and the United States [19,20,21,22], with a ratio of up to three men with polytrauma to every woman. On the other hand, the private health care system, to which 15 to 20% of the population belongs, comprises people from higher socioeconomic segments. Therefore, it could be inferred that people with fewer economic resources have a higher proportion of polytrauma victims in Chile. Several studies have found an association between socioeconomic status and the incidence of polytrauma, explaining this finding by the use of vehicles with less safety equipment and a greater distance traveled as a pedestrian [23,24].
Concerning the age of the patients reported for health problem No. 48, this is consistent with international reports, in which the most affected group is between 15 and 64 years of age, half of whom are between 20 and 40 years of age [22,25]. It is essential to highlight this result given that they correspond to patients of productive age, which is associated not only with health care costs per se but also with significant social costs due to absenteeism from work, prolonged rehabilitation periods, and even disability pensions [26]. Finally, mental health expenditure must be considered for the affected individual and the family group [3]. Although not the most affected group, people over 60 years of age, especially in road traffic accidents, require age-specific actions to reduce the incidence of high-energy trauma injuries, especially in those with low socioeconomic status [27].
In addition, there is great diversity in notification rates by region, with higher rates in geographically adjacent regions. This is the case in the Metropolitan and O'Higgins Regions and the Los Lagos and Los Ríos Regions. Future research should delve deeper into these patients' flow and outcomes to define whether these areas require specialized trauma centers or higher physician density. However, it should be noted that adding trauma centers in areas without access may improve the availability of trauma care. Conversely, adding trauma centers in areas without access problems may dilute expertise and patient volume for those centers [28].
Regarding the influence of implementing the Explicit Health Guarantees Law on the mortality of polytrauma patients, unfortunately, the Explicit Health Guarantees database does not have patient outcomes, so it was impossible to determine post-notification mortality. This is important, given that all pathologies that enter the system of Explicit Health Guarantees undergo an a priori cost-effectiveness study. However, once the measure is in place, there is no follow-up of outcomes, and the measure’s impact is not systematically evaluated. The current guideline related to the Explicit Health Guarantees for severe polytrauma was published in 2007. Although it was intended to be updated every two years, this has not happened. To infer the impact of the Explicit Health Guarantees on mortality through the external cause mortality database of the Department of Health Statistics, we analyzed only those cases of death occurring in a health institution. This is because those grouped under 'other' or 'home' may correspond to instantaneous deaths, not being notified, and not receiving care corresponding to the Explicit Health Guarantees. This analysis identified a change in the rate of deaths due to external causes precisely in 2007, a change that can be attributed to including this pathology in the system of Explicit Health Guarantees. However, this analysis has the bias that those who were notified received the benefits of the Explicit Health Guarantees and died at home as a result of sequelae were excluded from the analysis.
Analysis of the mortality database of the Department of Health Statistics showed that deaths due to trauma or external causes are the fourth leading cause of death in Chile, followed by cardiovascular deaths, tumors, and respiratory system diseases. A similar situation was reported in the United States in 2021 [29], with the leading causes being cardiovascular, tumors, and death from COVID-19. Head trauma was identified in this study as the leading cause of high-energy trauma deaths in Chile, a situation similar to that reported in the Netherlands [19] and the United States [30].
On the other hand, the main mechanism of mortality in high-energy trauma found in this study was pedestrian accidents (17%) and in fourth place with 14% other motor vehicle accidents. This highlights the relevance of reducing road accidents in order to reduce mortality in high-energy trauma. In this context, road factors, including the availability of high-capacity roads, the percentage of the population consuming alcohol, and the proportion of heavy vehicles, have been described as modifiable risk factors [24].
The work of the National Traffic Safety Commission since 1993 has been important for the prevention of traffic accidents in Chile, with a broad spectrum of action ranging from requiring safety measures for motor vehicles, raising the requirements for obtaining a driver’s license, zero tolerance for alcohol and other drugs, and implementing mandatory safety features such as seat belts, airbags, and child restraint systems. The time series analysis conducted in this paper shows a significant structural change in high-energy trauma mortality in 2020, which can be attributed to the National Traffic Safety Commission’s implementation of basic car safety requirements. However, it is also important to note that other studies have reported that the 2005 traffic law reform in Chile has positively impacted the reduction of traffic accidents, thus contributing to a decrease in high-energy trauma [31]. This reform, which included mandatory child restraint systems, has proven to be crucial in reducing both fatality and severe injury rates in children involved in road crashes [32]. A subsequent analysis of drink-driving laws in Chile, which included increased penalties in 2012 and 2014, also showed a decrease in crashes and injuries, underlining the importance of legal measures to address high-energy trauma [33].
To decrease mortality in high-energy trauma, efforts should not be limited to road traffic crashes. In this study, it is observed that the second and third leading causes of death are falls and assaults. In this framework, the maximum number of deaths occurred during the 2010 earthquake. Therefore, it is relevant to note that other events, such as the 2010 earthquake, the 2019 social crisis, and the COVID-19 pandemic, may also influence trauma patterns in Chile, underlining the need for a comprehensive approach to address this public health problem [34]. Furthermore, this comprehensive approach must include occupational accidents, where falls from height are frequent, especially in the transport and communications, mining, and fishing sectors, where fatal occupational accident rates are exceptionally high [35]. By adopting a public health framework that considers the multilevel factors that influence trauma, Chile can make significant progress in reducing the burden of high-energy injuries and improving its population’s overall health and well-being.
This study has limitations. Primarily, it is a retrospective study based on international and national registries. Therefore, there is a risk of bias inherent in the quality of the records for each event. In addition, there is no single indicator for high-energy trauma. In some databases, it is restricted to car accidents. In others, it includes external causes such as food or drug poisoning, making it complex to compare with other publications. Moreover, the databases reviewed only contain patient sex and not gender, which limits addressing possible gender inequalities in terms of access to health care, social support, and differences in risk behavior.
Finally, the explanatory variables in each section do not include all the factors associated with high-energy trauma, so the authors suggest caution when extrapolating the results. However, we consider this study to be a robust initial analysis to generate hypotheses to demonstrate measures to improve high-energy trauma indicators and, in the future, to trigger public policies that impact the indicators. For example, to determine how the density of doctors and specialists per region influences mortality and the number of notifications of Explicit Health Guarantees in each region of Chile. Especially in the Metropolitan-O'Higgins and, Los Ríos and Los Lagos regions, where the highest notifications of Explicit Health Guarantees were found. Thus, future studies could focus on identifying how the global variables of the country affect notifications and mortality in each region of our country.
Conclusions
In 2019, Chile ranked 82nd among WHO countries in deaths per 100,000 inhabitants caused by motor vehicle accidents. On the other hand, the proportion of health expenditure and the density of physicians in each country are significantly associated with the rate of road traffic deaths.
Notifications of Explicit Health Guarantees for severe polytraumatization are more frequent in patients between 20 and 40 years of age, male, and affiliated with the National Health Fund. No data are available on the outcome of those patients who were notified.
The rate of deaths due to external causes shows a decreasing trend concerning the total proportion of deaths, with the year 2000 being identified as a moment of significant change in the total number of deaths due to external causes. The same happened in 2007 for the total number of deaths due to external causes in a hospital center.

