Análisis
← vista completaPublicado el 12 de mayo de 2022 | http://doi.org/10.5867/medwave.2022.04.002511
Impacto de la pandemia por COVID-19 en la incidencia de artroplastías de rodilla en Chile: estudio transversal basado en registro nacional
Impact of COVID-19 outbreak in knee arthroplasty in Chile: a cross-sectional, national registry-based analysis
Abstract
Introduction The need for beds and health personnel to treat coronavirus (COVID- 19) patients has led to the suspension of many elective sur-geries in Chile, including knee arthroplasties. This study aims to determine the incidence of knee arthroplasty in 2020, reflecting the effect of the COVID- 19 pandemic, and estimate the cost and time it would take to recover the waiting list prior to March 2020.
Methods A cross- sectional study was designed. We analyzed databases from The Department of Statistics and Health Information databases from Chile for 2019 and 2020, identifying patients with surgical discharges associated with knee arthroplasty codes. We estimated the time it would take to recover the surgeries unperformed in 2020 by simulating a monthly workload increase from the 2019 baseline. The costs of knee arthroplasty paid by the National Health Fund to institutions were estimated by diagnosis-related groups.
Results We found that the incidence rate of knee arthroplasty in 2020 decreased by 64% compared with 2019. The impact was higher in the public system (68%) and the National Health Found (63%). A simulated increase in knee arthroplasty productivity by 30% would allow recovering the postponed knee arthroplasty surgeries in 27 months, at a monthly cost to the public system of 318 million Chilean pesos (378 thousand US dollars).
Conclusions The incidence rate of knee arthroplasty during 2020 decreased by 64%, revealing the extensive waiting line for people with knee osteoarthritis. An increase between 20- 40% in productivity compared with 2019 would allow recovering the unperformed surgeries in 20 to 41 months, at a monthly cost to the public network between 210 and 425 million Chilean pesos (250 to 506 thousand US dollars).
|
Main messages
|
Introduction
The coronavirus pandemic (COVID- 19) has highly affected health systems around the globe, including both outpatient and inpatient settings [1]. The need for beds and health personnel to treat coronavirus patients has led to the suspension of many elective surgeries in Chile, including knee arthroplasties [2]. For example, in the United States, there is an estimated decrease of 100 000 arthroplasties for each month of confinement [3].
Although there are reports of dissatisfaction with knee arthroplasty [4],[5], this surgery has proven to be a cost-effective treatment for severe gonarthrosis and has been recently proposed as a strong candidate to enter the program of Explicit Health Guarantees for Chileans [6]. Furthermore, the Organization for Economic Cooperation and Development (OECD) establishes the access to knee arthroplasty as an indicator of health, given the impact this treatment has on the quality of life of patients with knee disorders [7].
In the Chilean health system, coverage is mainly provided by two types of insurance: public insurance provided by the National Health Fund and private insurance. According to the National Socioeconomic Characterization Survey of 2020, it is estimated that 76.5% of the population belongs to the National Health Fund, 15.4% private health insurance, 2.6% to an insurance related to the armed forces, 4.3% to none, and 1.2% do not know [8].
Two types of institutions provide services for hospitalized patients: the public health network and private health institutions. The public health network serves patients affiliated to the National Health Fund. On the other hand, private health institutions correspond to a broad spectrum that includes university hospitals, workers' mutual funds, armed forces hospitals, police hospitals, and centers belonging to investment funds. In addition, some patients affiliated to the National Health Fund choose treatment in private health facilities at their own expense to avoid waiting time for surgery.
Prior to the pandemic (2019), the rate of knee arthroplasty in Chile was 28.23 per 100 000 population, being well below the 54.49 for hip arthroplasty [9]. Among the Member countries of the OECD, Chile ranks second to last in knee arthroplasty rate per 100 000 population [7]. Furthermore, prior to the pandemic, knee arthroplasty represented the second elective surgery with the longest waiting list in Chile – totaling 15 132 pending cases – according to the Ministry of Health of Chile via Transparency Portal (Annex 1).
The waiting time for elective surgeries directly impacts health user satisfaction. The magnitude of the wait depends on several factors, including the capacity and efficiency of the health system, medical management, and the population’s demographic characteristics [10]. Gathering information to plan future solutions is key to responding to the population’s health needs. According to the incidence of knee arthroplasty in the last five years in Chile [9], a rate of 29.29 knee arthroplasties per 100 000 population was estimated for 2020. In absolute terms, this represented 5699 arthroplasties. This article aims to determine the impact of the first year (2020) of the COVID- 19 pandemic on the incidence of knee arthroplasty in Chile. In addition, we seek to determine if this incidence is associated with the degree of confinement in Chile or the number of reported cases of COVID- 19, along with estimating the time and cost it would take to recover the waiting list prior to the COVID- 19 outbreak.
Methods
A cross- sectional study was designed, where the open-access database of the Department of Statistics and Health Information (DEIS, available at https://deis.minsal.cl/#datosabiertos) was analyzed. This database stores all hospital discharges in the country, both from public and private institutions. The databases for 2019 and 2020 were downloaded and scanned using ACCESS software (Microsoft®). All patients discharged with surgery codes 2104153 and 2104253 between January 1, 2019, and December 31, 2020, were identified. Public and private institutions use these codes in Chile to identify a knee arthroplasty procedure, regardless of the cause of osteoarthritis (e.g., primary or secondary to fracture sequelae), type of prosthesis (e.g., total or unicompartmental), or whether it corresponds to a revision arthroplasty.
The incidence rate of knee arthroplasty in Chile was calculated using the population data reported by the Chilean National Institute of Statistics. The "country mobility" was extracted from the report of the Instituto Sistemas Complejos de Ingeniería, which analyzes mobility based on the Global Positioning System provided by smartphones, giving information on the amount and distance of movements of each inhabitant in Chile during 2020. The first two weeks of March 2020 are used as a reference, and the mobility is expressed as the percentage variation throughout the year. This method allowed us to estimate the degree of confinement in Chile during the first year of the pandemic.
The cost of knee arthroplasty in the public system was calculated according to diagnosis-related groups (DRGs). This methodology of payment values procedures by setting a base price, equivalent to the average price of hospital discharges, multiplied by the relative weight of each diagnosis-related group. The estimated base price of diagnosis-related groups was $2 073 897 (2468 US dollars), and the relative weight of knee arthroplasty was 1.5. To this, we added – in the case of knee replacement – a technology adjustment for the use of implants, which totals $1 190 000 (1416 US dollars) for 2021. Therefore, the estimated price paid by the National Health Fund per knee arthroplasty discharge was $4 300 845 (5113 US dollars) (Annex 2). The price of knee arthroplasty in the private sector was not estimated because its cost varies through institutions and health coverages.
An exploratory analysis of the data was performed. Spearman correlation (Rho) was used to analyze the correlation between knee arthroplasties, the number of monthly cases of COVID- 19 reported by the Chilean Ministry of Health, and the country’s mobility. Subsequently, the average monthly knee arthroplasty in 2019 was calculated to estimate the number of prostheses per month that can be performed in scenarios of 20, 30, and 40% increase in productivity. Finally, the monthly cost for the public system was estimated according to diagnosis-related groups to compensate for the number of arthroplasties unperformed in the public system. STATA v.17 (StataCorp LP, College Station, Texas, USA) was used for the statistical analysis.
Results
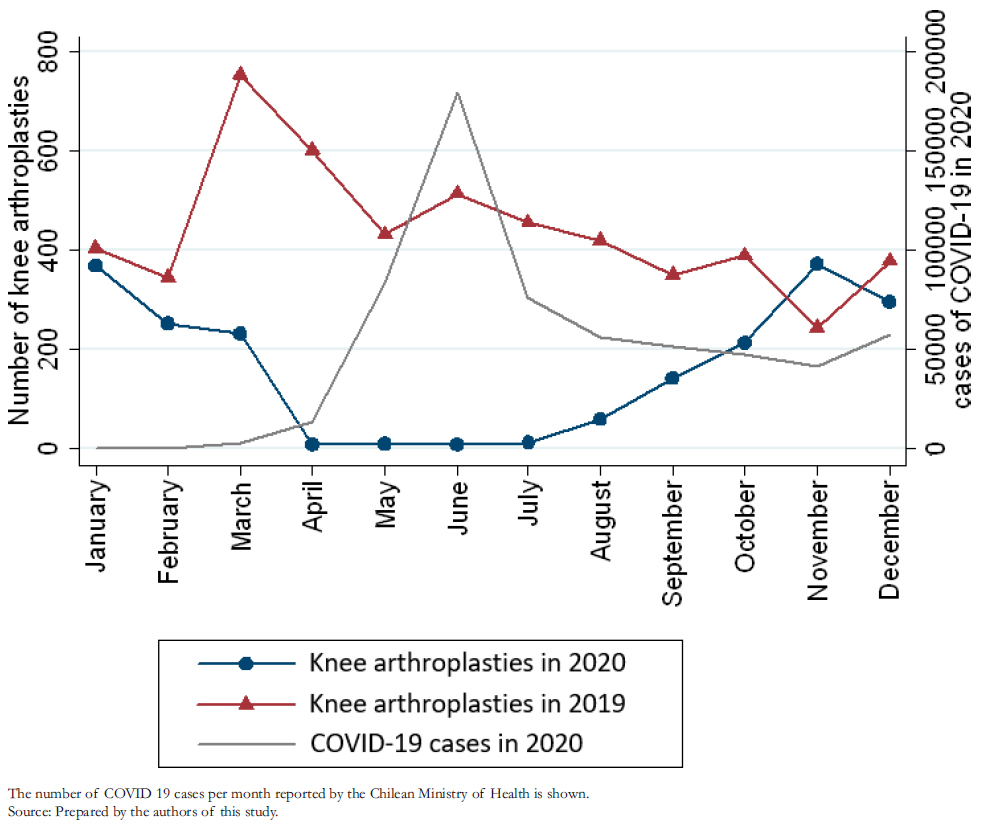
A total of 1972 knee arthroplasties were performed in 2020, corresponding to an incidence rate of 10.13 per 100 000 population. Compared to 2019, a 64% decrease in the rate of knee arthroplasties per 100 000 population was observed, being the lowest incidence since 2012 (Table 1). In absolute numbers, 3315 fewer knee arthroplasties were performed in 2020 than in 2019 (Figure 1) and 3727 fewer than the pre-pandemic projection for 2020. The number of knee arthroplasties in 2020 had a moderate correlation with the number of cumulative cases per month of COVID- 19 (Rho = -0.58; p = 0.0503) (Figure 1) and a strong correlation with the country’s mobility (Rho = 0.98; p < 0.0000) (Figure 2).
The greatest impact occurred in the public network, where the drop was 11% higher than in private centers. The same occurred with patients from the National Health Fund, who received 10% fewer arthroplasties than those from private health insurance (Table 2). Figure 3 shows that the increase in knee arthroplasties in public centers is one month behind the private centers. Regarding the incidence of knee arthroplasties in patients over 60 years, we observed that for every knee arthroplasty performed in patients of the National Health Fund, 3.7 knee arthroplasties were performed in patients affiliated to private insurance.
In 2019, the monthly average of knee arthroplasties was higher in public than in private institutions (247 vs. 194). If the productivity of 2019 were increased by 30% (321 knee arthroplasties per month), it would take 27 months to recover the surgeries unperformed during 2020. We estimated that this surplus in surgeries would add 318 262 530 Chilean pesos (379 000 US dollars) to the 2019 monthly expenditure on knee arthroplasties (Table3).
 Full size
Full size 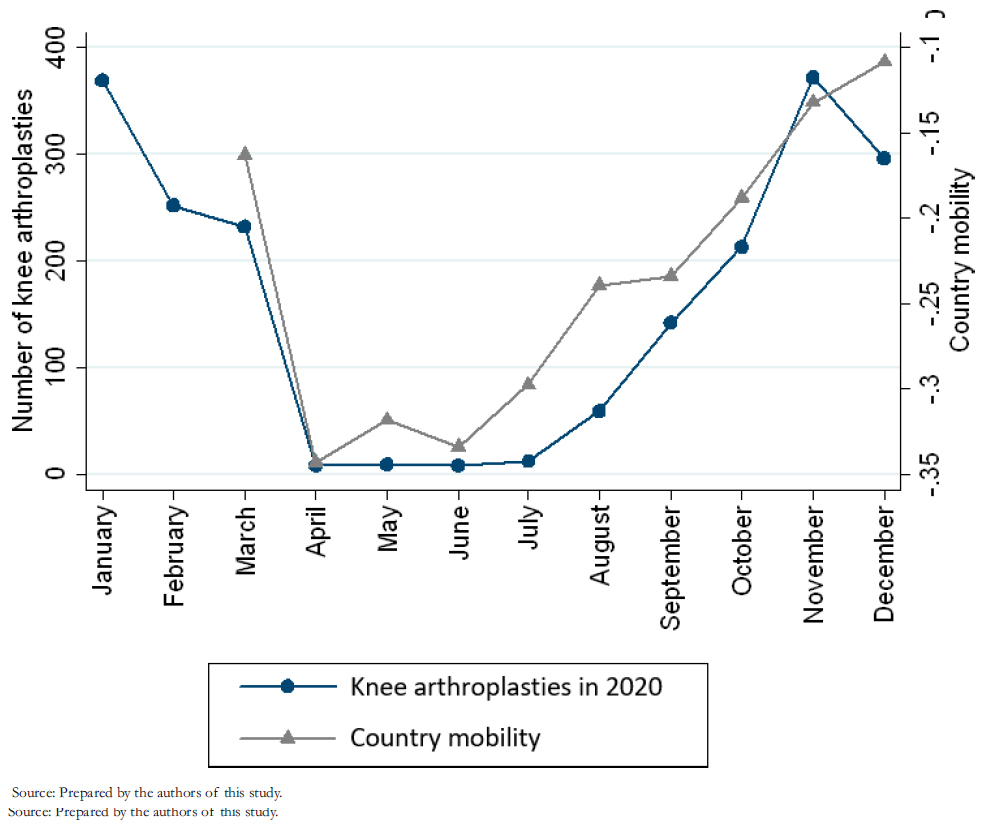 Full size
Full size 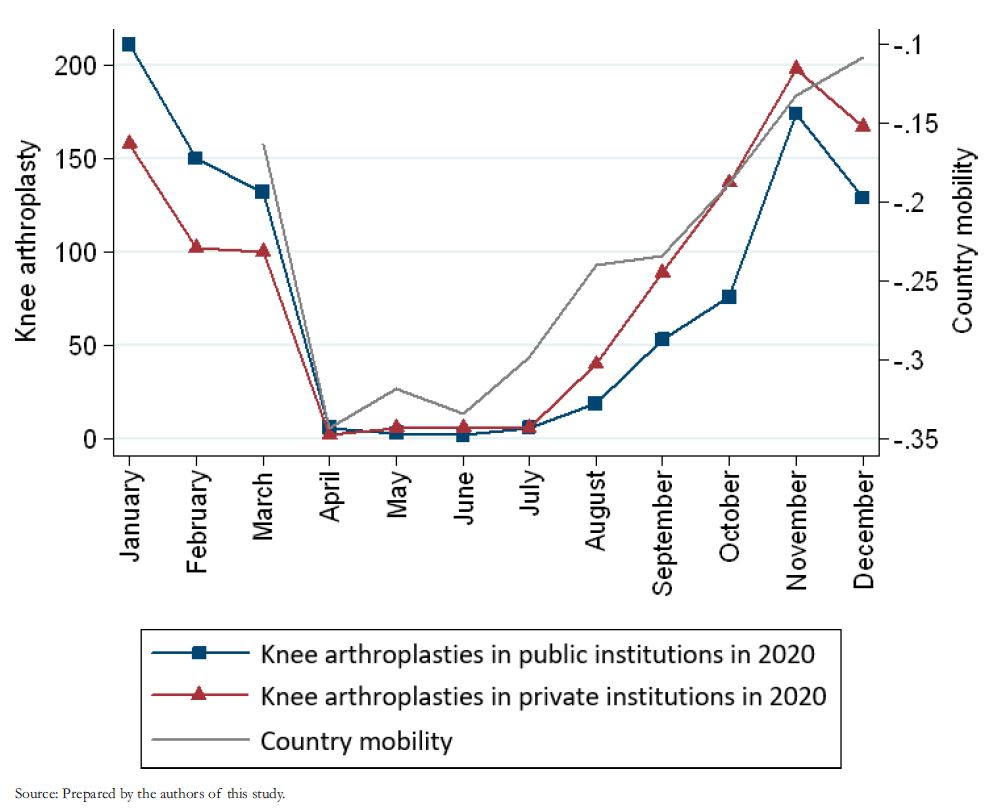 Full size
Full size 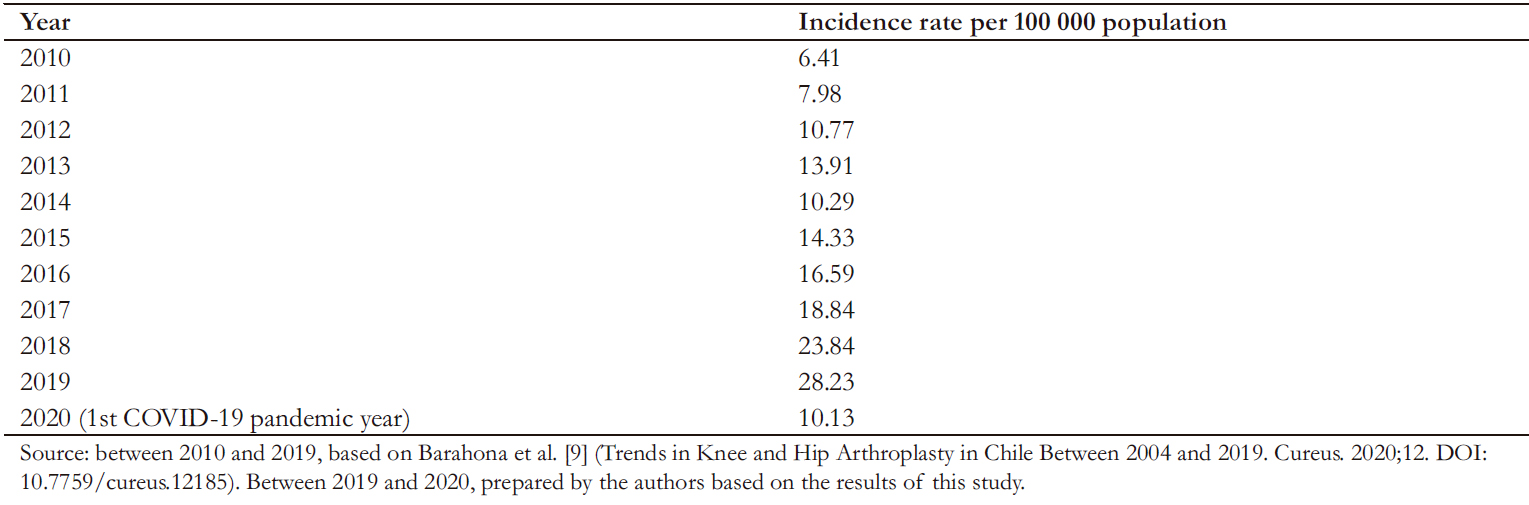 Full size
Full size 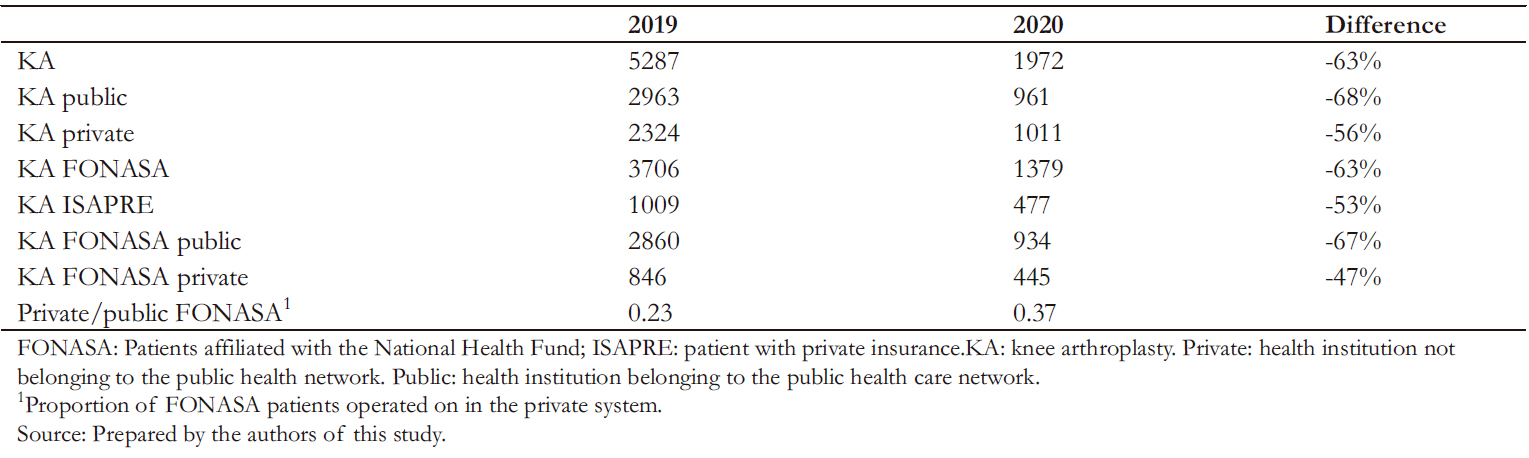 Full size
Full size 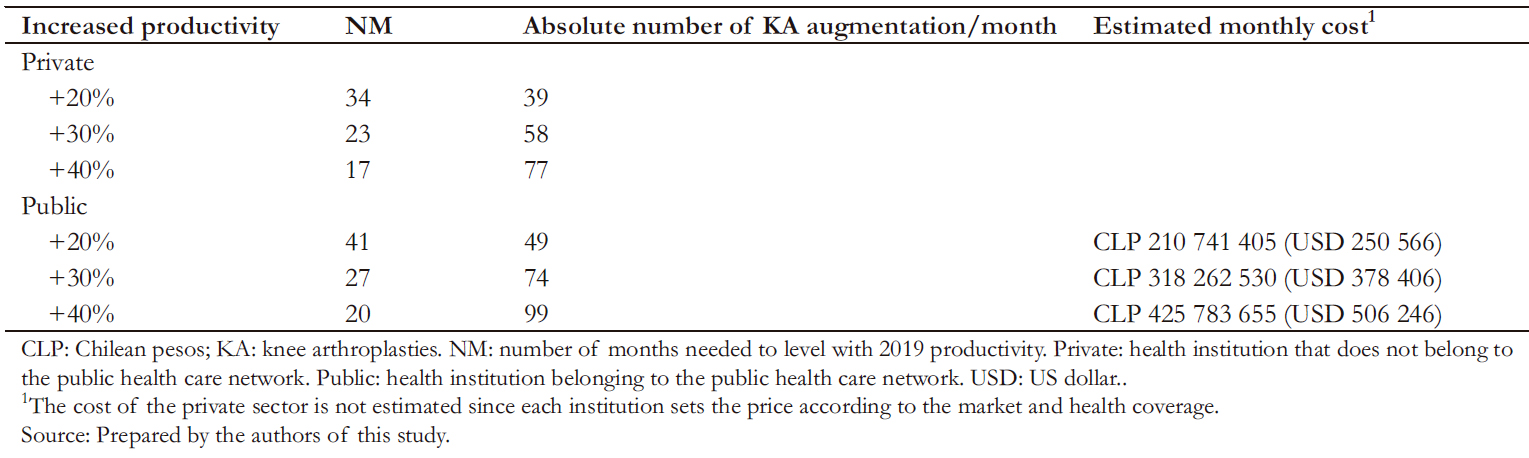 Full size
Full size Discussion
This study found that it would take 17 to 41 months to recover the number of knee arthroplasties unperformed due to the coronavirus pandemic, depending on the increase in productivity and the analyzed sector. Gonarthrosis is a highly disabling disease with increasing prevalence, and barriers to access surgery limit its treatment in Chile. Therefore, important planning is required to resolve this problem in our country. According to the Transparency Act website, the waiting list was already high prior to the pandemic, with 15 132 pending surgeries. Considering that 5290 were performed in 2019, the waiting list is equivalent to 2.8 years of surgeries. This number of waiting patients in Chile is only surpassed by the 16 548 patients waiting for cholecystectomy (Annex 1).
The decrease in the number of knee arthroplasties performed during 2020 is multifactorial and not limited to Chile. The fear of an increase in mortality in perioperative knee arthroplasty during the pandemic, the use of surgical areas for COVID-19 patients, and the redistribution of surgeons to other services for COVID- 19 patient care or collaboration in administrative activities were the main factors that influenced the marked decrease of knee arthroplasties [2]. A study conducted in the United Kingdom during the pandemic – prior to the closure of surgical wards – showed that knee arthroplasties did not increase morbidity and mortality, except in patients infected with COVID-19 during hospitalization, where mortality reached 20% [11]. For this reason, it is necessary to follow international guidelines and adapt them to each current reality in Chile to maintain elective surgeries in flare-ups of COVID-19. The proposed recommendations include zones free of COVID-19 patients, appropriate personal protective equipment, and routine examinations with nasal swabbing to rule out coronavirus infection prior to surgery. Moreover, these measures should be supported by appropriate vaccination campaigns [12],[13].
A center in Vienna, Austria, reported a decrease in 22% of knee arthroplasties during 2020 compared with 2019, which is milder than we found in Chile [14]. However, the Scottish registry estimated a 61% reduction in knee arthroplasties in 2020 compared with 2019. The same study estimated that a monthly increase of knee arthroplasty by 20% would take four years to return to the pre-pandemic waiting list in Scotland [15]. These findings are similar to ours, where a 20% increase in productivity would mean a recovery time of three years and five months in Chile. To shorten this waiting time to two years, we estimated that it would take a 40% increase in knee arthroplasty activity.
Three issues are vital to increasing the performance of knee arthroplasties in Chile: the number of beds, ward efficiency, and reducing costs associated with complications. Bed availability is critical for any institution that wants to increase knee arthroplasty volume, particularly during the COVID-19 pandemic. One strategy is to design early discharge or outpatient programs. Outpatient and early discharge knee arthroplasty programs are efficient when adequately implemented, ensuring interdisciplinary evaluation with appropriate patient selection and education [16],[17],[18],[19]. There is experience with outpatient management of hip arthroplasty in the Chilean public service with good results. This model could be extrapolated to knee prostheses and other hospitals in the country [20].
There is robust evidence on maximizing the efficiency of elective surgical wards, which require adaptations according to the infrastructure and times of each health center. Although common sense should not be overlooked, probabilistic algorithms for scheduling surgeries should be contemplated to maximize ward throughput [21]. Ward use has historically been more efficient in private than public institutions [22]. The major difference between these institutions appears to lie in waiting times between surgeries rather than the duration of the procedure itself. For example, a study conducted in New Zealand showed that the difference in average surgery time in knee arthroplasty is only three minutes between public and private centers [23].
Another option that health centers with high arthroplasty volume have taken to increase throughput is to alternate surgical wards. This strategy – consisting of a team utilizing two operating rooms in a block of time to increase the number of scheduled surgeries – appears to increase productivity in knee arthroplasty without increasing complications and associated costs [24],[25],[26].
Post-surgical complications are the main factor associated with increased costs in knee arthroplasty programs. Half of the complications occur due to medical decompensation, so preoperative evaluation and strict follow-up of comorbidities during the perioperative period are essential for a cost-effective program [27].
Another strategy to reduce costs associated with knee arthroplasty is to perform surgeries in centers with a high volume of knee arthroplasties because they tend to have lower complication rates [28]. Finally, providing the surgeon with information on surgical performance has been shown to reduce costs in knee arthroplasty resolution programs. These data are divided into three dimensions: patient demographics (e.g., age, gender, and weight), clinical outcomes (e.g., operative time, hospital stay, and patient functional outcomes), and costs associated with their procedure [29].
The COVID-19 pandemic presented us with an opportunity and a necessity to improve efficiency in knee arthroplasty. Many unresolved pathologies during the pandemic will further stress a system already overwhelmed by high-volume waiting lists. Early discharge programs, improving the efficiency of ward use, and boosting high-volume knee arthroplasty units are essential strategies for the post-pandemic era. As Explicit Health Guarantee for Chileans program appears to be a cost-effective policy, the strategies mentioned above could be articulated by incorporating this surgery into the Law [6].
The limitation of the study is that the data were obtained from a registry that may have data collection and coding biases. Also, this registry does not allow differentiation of the cause or type of arthroplasty performed. However, this bias is systematic in all years, not only for the 2020 results.
Conclusions
The incidence of knee arthroplasty per 100 000 inhabitants during 2020 decreased by 64%, so a large increase in the number of patients on the waiting list in the public health system is expected. A strong correlation was observed between the degree of confinement in Chile and the number of knee arthroplasties performed in the country beyond active COVID-19 cases.
An increase between 20 and 40% over the 2019 baseline work-load for 20 to 41 months would recover knee arthroplasties deficit at a monthly cost between 210 and 425 million Chilean pesos (250 to 506 thousand US dollars).
The capacity of each center to increase productivity will most likely not be homogeneous, as some centers will be able to do it closer to 20% and others to 40%. Therefore, it is essential to implement central policies that address strategies and create incentives to improve access to this surgery and quality of life in patients with gonarthrosis.
Notes
Contributor roles
MB: conceptualization, methodology planning, data management, writing the original paper, and project management. AM: methodology planning, research, critical review of the manuscript, and manuscript editing. MAB: research, data search, critical review of the manuscript, editing of the manuscript, and project management. MR: research, data search, data management, and writing the original paper. CB: validation, Research, data management, writing the original paper. CI: validation, research, critical review of the manuscript and editing of the manuscript, and project supervision.
Acknowledgments
The first and third authors are grateful for the continued support of Leonel Barahona to continue developing clinical research.
Competing interests
The authors declare that they have no conflicts of interest.
Funding
This work did not receive funding from any institution.
Ethics
The ethics committee of our institution determined that its approval was not necessary, given that the work only uses open- access data (study on secondary sources).
Provenance and peer review
Not commissioned. Externally peer- reviewed by four reviewers, double- blind.
Language of submission
Spanish.
Data availability statement
The databases used in this work are open- access and can be downloaded at: https://deis.minsal.cl/#datosabiertos and https://covidanalytics.isci.cl/movilidad/.

