Notas metodológicas
← vista completaPublicado el 13 de diciembre de 2024 | http://doi.org/10.5867/medwave.2024.11.2981
Conceptos generales sobre las evaluaciones económicas en salud
General concepts on health economic evaluations
Abstract
Health economics is an area of study that has critical tools for evidence-based healthcare decision making, among which are economic evaluations. These tools allow us to weigh the costs incurred for a given intervention in relation to its health outcomes. The main utility of these studies lies in accomplishing decision-making in healthcare and the formulation of public policies. This article is the first of two reviews on whose main purpose is to address fundamental theoretical concepts of health economic evaluations to facilitate their understanding and critical analysis. The text is part of a methodological series on clinical epidemiology, biostatistics and research methodology conducted by the Evidence-based Medicine team at the School of Medicine of the University of Valparaíso, Chile.
Main messages
- Health economic evaluations are structured quantitative techniques that estimate and compare the relationship between the health effects or outcomes of two or more health technologies in terms of their associated costs.
- The cost estimation process considers the identification, quantification and valuation of these costs.
- Health outcomes in economic evaluations are represented as clinical effectiveness indicators or outcome measures, such as quality-adjusted life years or disability-adjusted life years.
Introduction
Health economics is the branch of economics that studies the use of resources in the healthcare environment by answering questions about what and how goods and services are produced and who will receive them. This area is relevant in the face of the accelerated emergence of health technologies and the availability of critical evidence-based decision-making tools. Health economics focuses on allocating limited resources most efficiently [1], and critical tools of this discipline are health economic evaluations. However, during the training of health professionals, these topics are not usually addressed in the curricula. This is because they are often considered exclusive competencies of those involved in public health and health management [2]. These tools are helpful for managers to make rational decisions in health, and in turn, they are valuable instruments for health adequacy, health prevention programs, public policies, and the appropriate allocation of resources.
This article is part of a methodological series on clinical epidemiology, biostatistics, and research methodology by the Chair of Research Methodology and Evidence-Based Medicine of the University of Valparaiso, Chile. This article will review the concepts of economic evaluation techniques, the concept of costs, their classifications and estimation processes, and the quality of life scales as possible outcomes to be studied in economic evaluations. In a future article, a continuation of this one, the cost-effectiveness, cost-utility, and cost-benefit analysis designs will be reviewed.
Health economic evaluations
Health economic evaluations are structured quantitative techniques for estimating and comparing the relationship between the outcomes and costs of two or more health technologies [3]. Health technology is any intervention developed to prevent, diagnose, and treat medical conditions, promote health, rehabilitate patients, or organize health services [3,4]. Generally, health economic evaluations are carried out to determine the most effective and efficient courses of action [3,5].
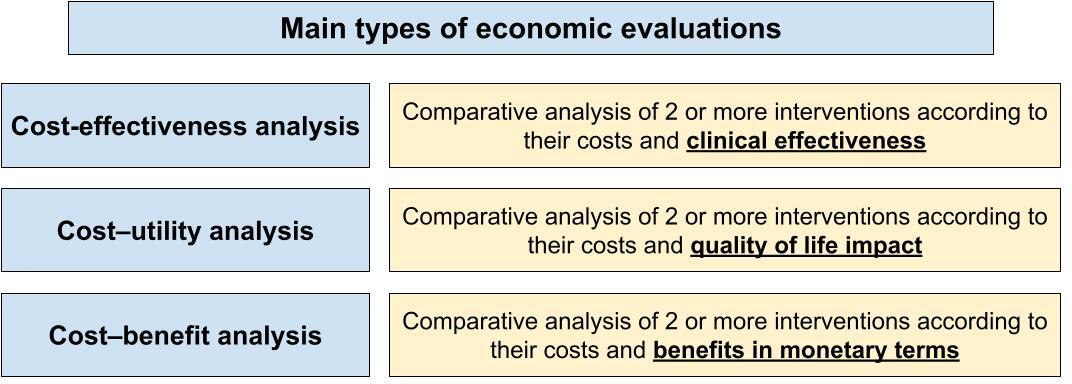
There are three main types of health economic evaluations: cost-effectiveness analyses, cost-utility analyses, and cost-benefit analyses [3].
The first group corresponds to studies that compare different interventions concerning their clinical effectiveness and costs. Their main objective is to determine which intervention offers a better health outcome for the money invested [6].
Cost-utility analyses evaluate the utility or value of quality-of-life-adjusted health outcomes in terms of costs [3]. Their central importance lies in evaluating the quality of life and the years of life gained related to a monetary unit invested [3].
Finally, in cost-benefit analyses, an evaluation is made in which both the costs and the benefits of the intervention are expressed in monetary terms. These studies calculate the economic return of investing in health technology [7]. Figure 1 shows a scheme that summarizes the main characteristics of these designs.
Main health economic evaluations.
Economic evaluations make it possible to evaluate health interventions and/or programs that have already been carried out, where the investment can be compared with the benefits obtained, as in the case of Example 1 (Box 1 [8]).
The cost-benefit study published by Sargazi et al. 2022 [8] discusses the economic impact of the HPV vaccination program in Iran during 2020 by comparing the costs and benefits between vaccinated and unvaccinated women. The disease-related costs were estimated based on the expenses for care received by HPV-positive (+) patients in an Iranian referral hospital and the cost of vaccines available in the country.
The total vaccine costs were estimated based on the unit cost, considering USD 29 for bivalent immunization and USD 151 for quadrivalent immunization. The costs associated with HPV infection and cervical cancer were USD 31.5 million, with a cost per person of USD 9266.
The net difference between the program’s benefits, due to the prevention of HPV infection and cervical cancer, and the estimated per-person vaccination costs was USD 7346 for the bivalent vaccine and USD 6439 for the quadrivalent vaccine.
In example 1, a program has already been implemented, but this analysis could be carried out preliminarily with data obtained from international literature.
These data are then grounded in the local environment to assess feasibility and applicability. Thanks to this, a health decision-maker can define a course of action or determine the continuity or otherwise of measures.
Costs
Costs correspond to the monetary value of the consumption of resources linked to producing a good or service sold during an established period. These costs directly impact the selling price of any product or service and the volume of its production [9].
Opportunity cost
Opportunity cost is the benefit foregone by making one decision over another over time [3]. Opportunity cost is not a direct monetary expenditure but the value of what is sacrificed due to a specific choice, as seen in Example 2 (Box 2, 10]). This involves considering what could have been gained if a different decision had been made [3].
In Argentina, in 2019, the treatment for type I spinal muscular atrophy with Spinraza was included in the benefits plan. This drug costs USD 483 480 per patient per year, and the program is estimated to treat 100 patients during 2019, leading the healthcare system to incur a cost of USD 48 348 000. The intervention reduces mortality at 13 months by 47%, with a minimum number needed to treat (NNT) of 3.4 patients per year.
During the same period, amidst the COVID-19 pandemic, Argentina estimated a 60% reduction in mortality from severe pneumonia caused by COVID-19, with a minimum NNT of 1.7 patients. A mechanical ventilator in the Argentine market costs approximately USD 20 000 per unit.
With the budget allocated for Spinraza, 2417 ventilators could have been purchased. Theoretically, financing the purchase of Spinraza with the mentioned outcomes would result in the loss of 2018 lives due to COVID-19.
It is important to emphasize that the hypothetical decision in Example 2 is dichotomous: either the ventilators are purchased, or Spinraza treatment is funded. Therefore, the decision involves setting aside an option that may or may not have benefited community health.
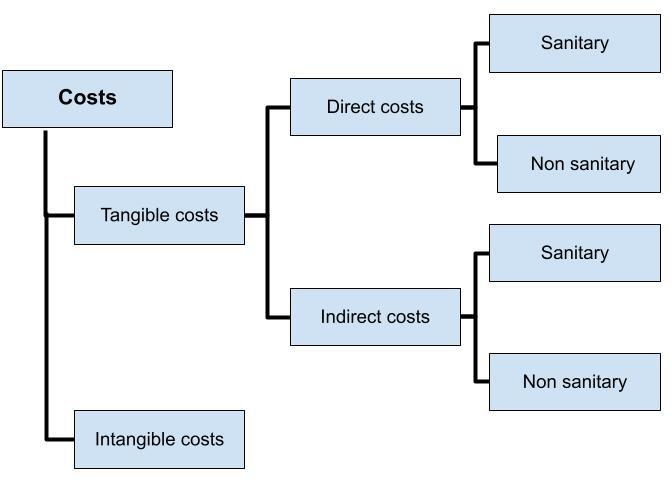
Types of costs
There are two broad groups of cost types: tangible and intangible. Although there are several classifications in the literature, we will use the one that subdivides tangibles into direct and indirect, which can be health or non-health. This is depicted in Figure 2 [3 and 11]. The categories mentioned come from the first Washington panel conducted in 1996 [12].
Traditional classification of costs related to health interventions.
 Full size
Full size Tangible costs are those that can be measured in monetary terms. They refer to the material and financial resources used in medical care, such as the cost of drugs, treatments, medical tests, and medical equipment [13]. Tangible costs can be direct or indirect. Direct costs are associated with the health intervention, while indirect costs are related to sequelae or consequences of the disease or health care [14].
On the other hand, intangible costs cannot be easily quantified in monetary terms. They refer to subjective or emotional aspects associated with medical care, such as pain, anxiety, or quality of life perceived by the patient [14].
Direct health costs are linked to therapies, health benefits, or health care in general. However, there are also direct costs that result from the health problem (such as transportation, accommodation, caregiver expenses, etc.), which the patient must incur. These are called direct non-health costs.
On the other hand, indirect health costs are related to the prolonged use of social or health services to prolong life. Similarly, indirect non-health costs derive from productivity losses due to illness or health intervention [3]. Some examples of the types of costs mentioned above can be seen in Table 1.
Cost estimation
Cost estimation corresponds to identifying, quantifying, and valuing the consumption of resources associated with the alternative actions considered in the economic evaluation. This process must be adjusted to each research question, context, and methodology. Generally, it consists of three stages: identification, quantification, and valuation.
The first stage identifies the costs associated with the interventions to be included in the analysis. This decision is made considering the objective of the research, the perspective to be adopted for the analysis [3], the time horizon of the analysis, and the ability to obtain this information from various sources (since a cost may be relevant but not included because quantifying or monetarily valuing the investment is not feasible). The perspectives of an economic evaluation can vary widely based on the research objective and the stakeholders' needs. Adopting a particular perspective is crucial, as it determines which costs will be relevant, how these are valued, and how the consequences of interventions are interpreted [3]. The main perspectives to be considered are:
This is the broadest perspective of all and considers the costs incurred by the system that provides the benefits and those incurred by the patient and his or her family to access such benefits. It is often used to evaluate publicly funded programs by considering the costs covered by the state and society [15]. In this perspective, the costs related to the production of the intervention, the costs directly borne by the patient and his or her family, and the indirect consequences of the intervention, such as loss of productivity, among others, should be included [16].
This considers the specific costs incurred by the health system [15]. This perspective analyzes the financial resources allocated to the health system and how they are distributed to provide the required medical services. Only the direct and indirect costs of the resources used to produce the intervention and the savings obtained due to the intervention will be considered [16].
These are the costs that impact the institutions in charge of health insurance, both providers and health insurers, or also the clinicians directly [15]. It should be noted that in case of any co-funding by the patient, the costs will not be considered in this classification. This perspective focuses on the direct costs incurred to perform the service [16].
Considers costs incurred by the patient out-of-pocket, with costs covered by insurers or national health plans already discounted. This perspective will generally include direct and indirect non-health costs and, depending on national coverage, direct and indirect health costs [15,17].
This is related to the fact that an economic evaluation of any kind carried out by the Ministry of Health from the perspective of society will be different from that of a healthcare center. In the case of having a correctly formulated research question together with the relevant perspective defined by the researchers, the results of the subsequent cost estimation process should be similar, regardless of the researcher who carries it out [18]. In case of divergences, these would be due to differences in the researchers' ability to obtain information.
Determining a perspective of the analysis will allow, in the first instance, the formulation of an appropriate research question, the choice of a relevant research methodology, and the consideration of the relevant costs to be reported. This will shape the data analysis to obtain relevant conclusions [18].
Finally, another relevant aspect to consider is the time horizon of the analysis, understood as the period over which the costs and consequences associated with the interventions to be evaluated will be considered. Its duration should ideally include all the costs and effects of the intervention under study. For this reason, the duration will generally be extended for those associated with chronic diseases or whose effect is prolonged, such as vaccination programs [15].
Second, the quantification of costs is performed. This corresponds to identifying the unit amount of resources consumed to carry out a single intervention, which can be presented with varying degrees of precision, depending on the information available on unit costs. Thus, minimum units of analysis can be used, such as the cost of the standard management of acute myocardial infarction in the emergency department, or aggregate measures can be used, such as "days of hospitalization". Quantification can come from experimental and observational clinical studies or a mathematical model that seeks to represent reality through data synthesis [3].
Thirdly, a cost valuation is performed. This is how the price to be paid per unit of resources involved in the intervention is determined [18]. In theory, the real price of a resource is the opportunity cost of that good in a given situation, which differs from the practice where the markets determine prices according to the time at which the transaction is incurred [9].
A problem at the time of valuation is that the expenditure will often be incurred at a future time, and once the investment has been made, the benefits may appear immediately or in the long term. This phenomenon is known as "time preference", where it is usually preferred to defer expenses as long as possible and receive benefits as soon as possible. To consider this factor at the time of valuation, the analysis must discount the future value to the present value, where the future value is adjusted based on the interest or discount rate that the cost of the resource suffers concerning time [3]. Through this technique, the researcher will be able to determine how time affects the valuation of costs. These notions are included in the analysis through correction factors, which can change according to the variables considered by the study.
Health outcomes
Outcomes in economic evaluations correspond to the relevant effects of a health intervention on the health status of the population studied. Quantitative clinical effectiveness measures (such as reducing mortality or hospitalization times using mean differences) can be used (as well as dichotomous outcome measures, such as relative mortality risk). In addition, there are multidimensional measures of quality of life, which will be described below. Finally, health outcomes can be assessed regarding costs incurred or opportunity costs [16,19]. Figure 3 shows a schematic division of some measures for assessing health outcomes used in economic evaluations.
Schematic classification of measures used to present health outcomes in economic evaluations.
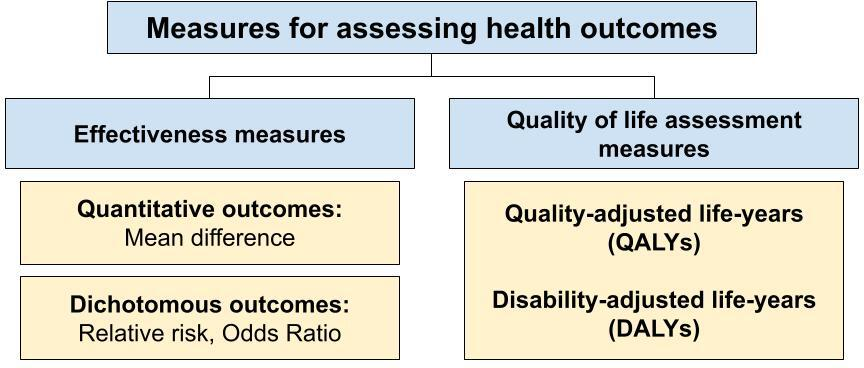
Outcome measures, such as Quality Adjusted Life Years (QALYs) or Disability-adjusted life years (DALYs), are metrics that seek to quantify both the quantity and quality of life gained or lost as a result of a specific intervention or disease [20]. These are essential in health economic evaluations, as they allow the integration of societal valuation in the evaluation of health interventions. These indicators correspond to how outcomes are reported in cost-utility analyses [21], allowing morbidity and mortality to be evaluated as an outcome of an investment made.
In addition, quality-of-life scales are also helpful for assessing the impact of chronic diseases and disabilities on patients' quality of life and society in general. These concepts will be discussed in more detail below.
Quality-adjusted life years
QALYs or QALYs (quality-adjusted life years) is an outcome measure that considers both individuals' survival and quality of life [22]. It is calculated as the product of life expectancy in years, weighted by a quality of life index defined on a scale from zero to one [22]. Thus, QALY is a global outcome measure that allows the comparison of interventions that have different effects on health in terms of quantity and quality of life [21]. The estimation of life expectancy should be made according to local estimates for each population, which can be rescued from the databases of the ministries of health.
It is essential to emphasize that standardized surveys should be used to measure quality of life. This is because they provide a measure that is comparable between different studies. This is crucial to ensure that the results of QALY studies are valid and reproducible. The primary surveys available are the EQ-5D used in the UK, China, and Chile, for example, and the SF-36 [22].
Among the limitations of using QALY, we find that it depends on the results of surveys' subjective quality of life and may vary from person to person. For this reason, it is susceptible to bias, given interpersonal variability [22]. In addition, QALYs are measurements performed in a particular place and time, so knowing the value of a particular pathology in 1999 is very different and not extrapolable to the results obtained from the same pathology today. Another limitation is the inability to make clinically small changes visible, which can be highly relevant. This can be seen in patients with terminal cancer, where there are very low life expectancies that considerably decrease the value of the indicator [23]. Another point to highlight is the concerns about the bioethical implications of using this measure since it could imply discrimination against people with disabilities or who are carriers of chronic diseases. This is due to how this indicator is calculated, since considering that a life with a disability has intrinsically a lower quality of life, a year of life for a person with a disability is worth less than a year of life for a person without disability [22].
For the interpretation of this indicator, it should be considered that a QALY is obtained by multiplying the number of years in a given state of health by the quality of life indicator associated with this state, where 1 indicates a perfect state of health and 0 indicates death [22]. In the case of Example 3 (Box 4 [24]), we have a gain of 1.7 QALY. This would be equivalent to 1.7 years of life in perfect health. Or 3.4 years of life with an intermediate health status of 0.5 and other possible combinations.
Sutherland et al. conducted a cost-utility analysis of laparoscopic cholecystectomy for symptomatic cholelithiasis. The study was carried out between 2013 and 2017 in Vancouver, Canada, through a secondary analysis of results from a prospective cohort.
The EQ-5D scale was applied before surgery, with an average score of 0.841 ± 0.133, and six months after surgery, with an average score of 0.908 ± 0.141, showing statistically significant differences. The calculation of QALYs was performed assuming two different scenarios: the first considering a life expectancy of 82 years in the country, and the second assuming that the health benefits would be reflected over 25 years.
Based on these assumptions, a gain of 1.76 QALYs was calculated for the first scenario and a gain of 1.743 QALYs for the second.
Disability-adjusted life years
DALYs or DALYs (disability-adjusted life years) correspond to an outcome measure that considers the effect of the burden of diseases and non-fatal conditions on health. This synthetic indicator combines potential years of life lost (PYLLL) with years lived with disability (YLD), reflecting health losses due to both premature mortality and disability related to these diseases.
The main advantages of using DALYs are to consider non-lethal effects on the quality of life of individuals, to consider individual life expectancy concerning the life expectancy of a given community, and to quantify the incidence of the point health condition on the health status of the person quantitatively from life expectancy [25,26,27].
The main disadvantage of using DALYs is that their accurate measurement can only be performed retrospectively. That is, the person must already be deceased to calculate the number of years of life lost prematurely and the number of years lived with a disability. Trying to counteract this last point leads to having to estimate each person’s life expectancy according to the evaluator’s judgment [27]. Another disadvantage to consider is the determination of whether each year of life lost is equally relevant to the other. This is why a mathematical function assumes that a year of healthy life between 20 and 25 years of age is more valuable than the rest of the periods of life. This assessment assumes the value that should be given to the individual and society [27].
Regarding whether a healthy year is more valuable today or in the future, Seuc [26] argues that there is a debate about whether to discount the value of the future year or not. According to the Global Burden of Disease and Injury Series, 3% of the annual value is discounted, so the adjustment could be made as a rule of thumb [27]. Finally, it is assumed that the disease burden for the individual and society does not vary according to socioeconomic status [27].
In Example 4 (Box 5 [28]), it can be concluded that the ROTARIX vaccine prevented 268 178 disability-free life-years or 268 178 life-years of premature death have been prevented.
Lourenço et al., a 2022 publication, presents a cost-utility analysis of the ROTARIX vaccine, introduced in 2015 in Mozambique, based on the outcomes of a cohort of patients between 2016 and 2020. Using national records, WHO databases, and the local immunization committee in Mozambique, the authors retrospectively obtained the corresponding values.
Through the vaccination plan, 963 701 cases of rotavirus diarrhea were prevented in children under 5 years old, of which 269 784 were severe cases, and 4628 deaths were avoided. According to the authors, this corresponds to 268 178 DALYs averted, considering the years lost to premature death in the cohorts and the time lived with the disease, based on the progression duration of the condition.
Conclusions
Nowadays, in the face of the great development of health technologies that offer new alternatives for the prevention, detection, and treatment of multiple conditions and pathologies, it is increasingly relevant to know how to efficiently allocate the resources allocated to health care, which are limited, in order to maximize health benefits. Health economic evaluations are fundamental tools for dealing with this problem because, by considering both the costs and possible benefits of alternative courses of action, they make it possible to assess what type of interventions can have the greatest impact on the health of the target population by making rational use of the resources available.
In order to be able to understand and critically analyze a health economic evaluation, clinical and administrative personnel should be familiar with the fundamental concepts of this type of methodological design since it not only involves adequately assessing the quality of the evidence from which the expected yield and cost figures are obtained but also familiarizing themselves with methodological aspects unique to health economic evaluations, such as the choice of a perspective and a time horizon relevant to the problem to be studied. All this with the ultimate goal of being able to contribute to rational and informed decision-making.
We hope this article will serve as a general introduction to the field of health economics. Continuing this paper, we will review fundamental methodological aspects of interpreting cost-effectiveness, cost-utility, and cost-benefit analyses.
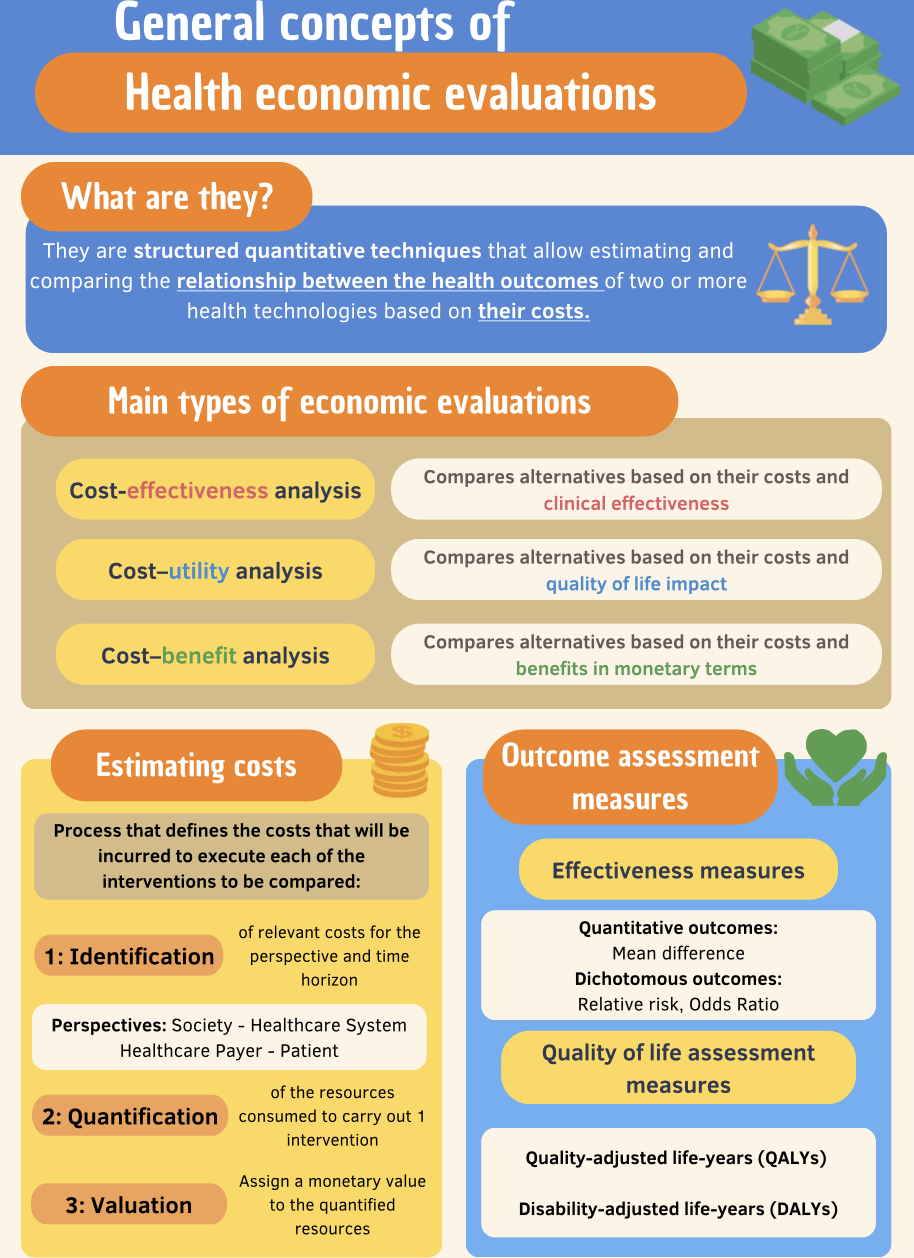
Finally, we present an infographic in Figure 4, which summarizes the most relevant aspects of the article.
Infographic summary of the concepts presented in this article.