Revisión clínica
← vista completaPublicado el 12 de noviembre de 2020 | http://doi.org/10.5867/medwave.2020.10.8060
Aspectos esenciales sobre el uso de hemocomponentes en el paciente hospitalizado: revisión narrativa de literatura
Essential aspects for the administration of blood components in hospitalized patients: A narrative literature review
Abstract
Introduction Transfusion medicine develops and disseminates guidelines that govern the optimal conditions for transfusion. The purpose of this article is to review the current evidence on the use of blood components.
Methods We searched PubMed, Scholar Google, ScienceDirect, SciELO and Cochrane web portals, as well as official documents published in the Chilean Society of Hematology. Articles from the last ten years were included, of which 42 were appropriate for this narrative literature review.
Conclusion First of all, there is a controversy between two types of strategies regarding the practice of red blood cell transfusion: a liberal strategy and a restrictive strategy. Second, for the management of coagulopathies, clotting times do not reflect the true ability of patients to clot. Third, to reverse the effect of coumadin, the administration of vitamin K would suffice over the use of fresh frozen plasma. Fourth, the use of physiological triggers could help define the best time for a transfusion.
|
Main Messages
|
Introduction
A blood component is a member of a group of elements that make up the blood, as highlighted by red blood cells (erythrocytes), platelets, plasma, and cryoprecipitate[1]. As a field of medicine, transfusion medicine is continually evolving. It develops and disseminates guidelines that state the optimal conditions for transfusing blood components, based on the balance between the benefits of transfusion and the possible adverse outcomes that need to be avoided. These adverse outcomes include hemolysis, the spread of viral diseases, nosocomial infections, thrombosis, inflammation, immunomodulation, acute lung injury, multi-organ failure, and circulatory overload secondary to transfusion, among others[2],[3],[4],[5].
This makes transfusion a costly and complex therapeutic intervention[6] since there is no conclusive evidence to determine a safety profile for its administration or the clinical benefit that some transfusion procedures could offer in critical settings. This creates a false sense of safety in its use, especially in some cases being used in excess or an ill-judged manner[2]. Nevertheless, transfusions are one of the most common procedures carried out in the hospital, where it is estimated that around 12.5% of patients will be transfused during their stay. Of this total, 47.1% of transfusions are performed in general medicine wards, 25.7% in the intensive care unit, and 19.8% in surgical wards. This incidence presents an increasing trend, especially in patients over 60 years of age[7]. It is, therefore, important to comprehend when and how to administer this therapy and what possible adverse reactions could happen after its use.
In this sense, this article’s objective is to review the current evidence regarding the use of blood components in clinical scenarios relevant to the hospital setting, such as managing anemia in critically ill patients, prophylactic correction of coagulopathy, and the reversal of the anticoagulant effect of coumadinics.
Methodology
For the selection of articles, we used the web portals and databases of the U.S. National Library of Medicine (PUBMED), Scholar Google, Science Direct, SciELO, and The Cochrane Library (Cochrane); we used keywords such as “Transfusion of blood components”, “transfusion of erythrocyte” and “transfusion of platelet” in the Medical Subject Headings Section (MESH), combined through the Boolean operators AND and OR. In addition, official documents published in the Sociedad Chilena de Hematología (Chilean Society of Hematology) were used.
From the resulting documents, which include review and research articles from the last ten years, 42 articles were selected that fulfilled the objectives set for this narrative literature review. The results are exposed per the following themes: pathophysiology, evidence-based recommendations for the transfusion of red blood cells, prophylactic correction of coagulopathies, and the reversal of the anticoagulant effect of coumadin utilizing fresh frozen plasma or Vitamin-K, with a final comment on the physiological triggers of transfusion.
Pathophysiology
1. Anemia, transportation, and oxygen consumption
The objective behind the transfusion of red blood cells is to improve the flow of oxygen in the blood (DO2) due to the intricate relationship at the tissue level between the flow of oxygen and its consumption (VO2)[8]. Once homeostatic mechanisms are lost, oxygen consumption becomes dependent on its flow, generating a physiological relationship altered in critically ill patients. Experimental studies show that, as anemia progresses, the flow of oxygen progressively falls[8]. This relationship is based on a critical point that suggests 5.0 g/dl of hemoglobin (Hb) as the nadir value, at which homeostatic mechanisms are lost, and tissue hypoxia and anaerobic metabolism ensue, achieving up to a 100% mortality rate with Hb values less than or equal to 2.0 g/dl[9].
In addition, it has been shown that anemic patients with critical Hb levels presented a rapid fall in lactate levels after transfusion of red blood cells, which consequently improved brain oxygenation[10]. However, one study showed no improvement in severely anemic critically ill subjects who were transfused with red blood cells (measured by parameters of tissue oxygenation)[11]. Furthermore, other studies have shown that the transfusion of red blood cells can deteriorate tissue oxygenation, which has been linked to increased morbidity, mortality, and duration of hospital stay in a dose-dependent relationship [10]. This deleterious result of transfusion may be associated with a direct cytopathogenic effect of the transfused erythrocyte[12], such as decreased nitric oxide availability and marked iron toxicity, and a loss of vasodilation within the microcirculation, ultimately leading to a state of inflammation, macrophage activation and endothelial injury[12].
2. Hemostasis and hemostatic capacity
Hemostasis is a phenomenon that depends on an adequate concentration of procoagulant factors (FI, FII, FV, FVII, FVIII, FIX, FX, FXI) and anticoagulants (Protein C, Protein S, and Antithrombin)[13], associated with an appropriate quantity and function of platelets, which in turn, depend on the inflammatory status, the endothelial function, the state of the vascular wall, the magnitude of the injury, and the pharmacological interaction (phenomena that are part of a system that determines the coagulation cascade)[13].
In this sense, the hemostatic potential is defined as this system’s capability to form a hemostatic clot once the coagulation cascade has been activated. This requires recruiting and activating a sufficient amount of prothrombin (prothrombin activation capacity) to form thrombin at a necessary rate and quantity (thrombin generation rate), which in turn generates fibrin (fibrin generation rate) in order to form a hemostatic clot from the recruitment and activation of fibrinogen. The thrombin generation rate can be kept constant as the clotting factors decrease until their concentration reaches 20% or less[14]. Therefore, it is estimated that the concentration of the factors may be in ranges higher than those necessary, which would mitigate the sudden change in their levels before altering the thrombin generation rate [14]. This situation can be seen in patients with hemostatic disorders such as hemophilia, who may show differences in thrombin generation rate (measured with a thrombinogram) compared to patients without this illness[15].
Evidence-based recommendations for red blood cell transfusion
Today there is a controversy between two trends when approaching transfusion in critically ill patients: a liberal strategy (with Hb levels between 9.0 and 10 g/dl) and a restrictive strategy (with Hb levels between 7.0 and 8.0 g/dl)[16]. A study carried out in 1999 randomized more than 800 patients into two groups for each transfusion strategy. This showed that the restrictive strategy to perform red blood cell transfusion for Hb levels < 7.0 g/dl was safe to perform[17], displaying lower mortality compared to the liberal transfusion strategy[17],[18]. Because of this, the restrictive strategy was considered a safe option in most cases[19], even reducing the mortality of patients in specific sub-populations, which indicates that certain permissive anemia does not seem to hinder clinical results.
Regarding complications, no significant differences were observed in the rates of infections and pneumonia; however, there was an increase in respiratory distress, acute lung edema, and acute coronary syndrome (ACS)[18] in the liberal strategy group[17]. Nonetheless, more recent studies ignited the controversy again when trying to compare these strategies, although it was shown that the restrictive strategy is indeed safer[20]. In critical conditions such as ACS and cardiac or oncological surgery, the liberal strategy tends to generate fewer complications[21],[22],[23]. This is in contrast to a systematic review that ended up refuting the evidence from observational studies for liberal red blood cell transfusion thresholds in patients undergoing cardiac surgery, associating them with a substantially higher risk of mortality and morbidity[24].
On the other hand, another study carried out in patients in the perioperative period and in critically ill patients compared these strategies again, and the results displayed lower mortality in the group that received the liberal strategy in the perioperative period (odds ratio: 0.81; 95% confidence interval: 0, 66 to 1.00; P = 0.05; I (2) = 25%), and no differences in mortality between critically ill patients for both strategies (odds ratio: 1.10; 95% confidence interval: 0.99 ± 1.23; P = 0.07; I (2) = 34%)[25]. Along these same lines, it has been documented that liberal transfusion strategies can produce better results in geriatric patients than restrictive transfusion strategies, which have increased the risk of mortality in this population at 30 and 90 days, contradicting current restrictive transfusion approaches[26].
Overall, it has been documented that restrictive transfusion strategies do not increase or reduce the risk of mortality at 30 days compared to liberal strategies[16], resulting in an uncertain risk/benefit balance using transfusions when Hb values are between 7.0 g/dl and 9.0 g/dl. Nevertheless, evidence has shown that transfusion, when Hb levels are greater than 9.0 g/ dl, does increase mortality, except in critical conditions in which the threshold may vary. Based on this, it is possible to recommend the restrictive use of red blood cell transfusion in the hospitalized patient as the standard strategy. In the absence of a critical condition, transfusion may be prescribed only in the case of severe symptomatic anemia with clinical evidence of tissue hypoxia[27]. The transfusion threshold of Hb < 7.0 g/dl ensures that Hb values are above critical Hb in most critically ill patients; however, what happens in situations where the Hb value varies between 7.0 and 9.0 g/dl and in those scenarios in which resuscitation is required must be clarified. The studies mentioned above conclude that Hb threshold values of 8.0 g/dl could be sufficient in circumstances in which resuscitation is required, especially if events such as ACS and cardiac or oncological surgery develop (as occurs in the postoperative period)[27]. It is recommended to transfuse only one unit of red blood cells and evaluate the response, restricting ourselves to the smallest number of units necessary to avoid complications (Table 1)[27]. One unit of red blood cells is expected to raise Hb by 1 g/dL or hematocrit by approximately 3%[1].
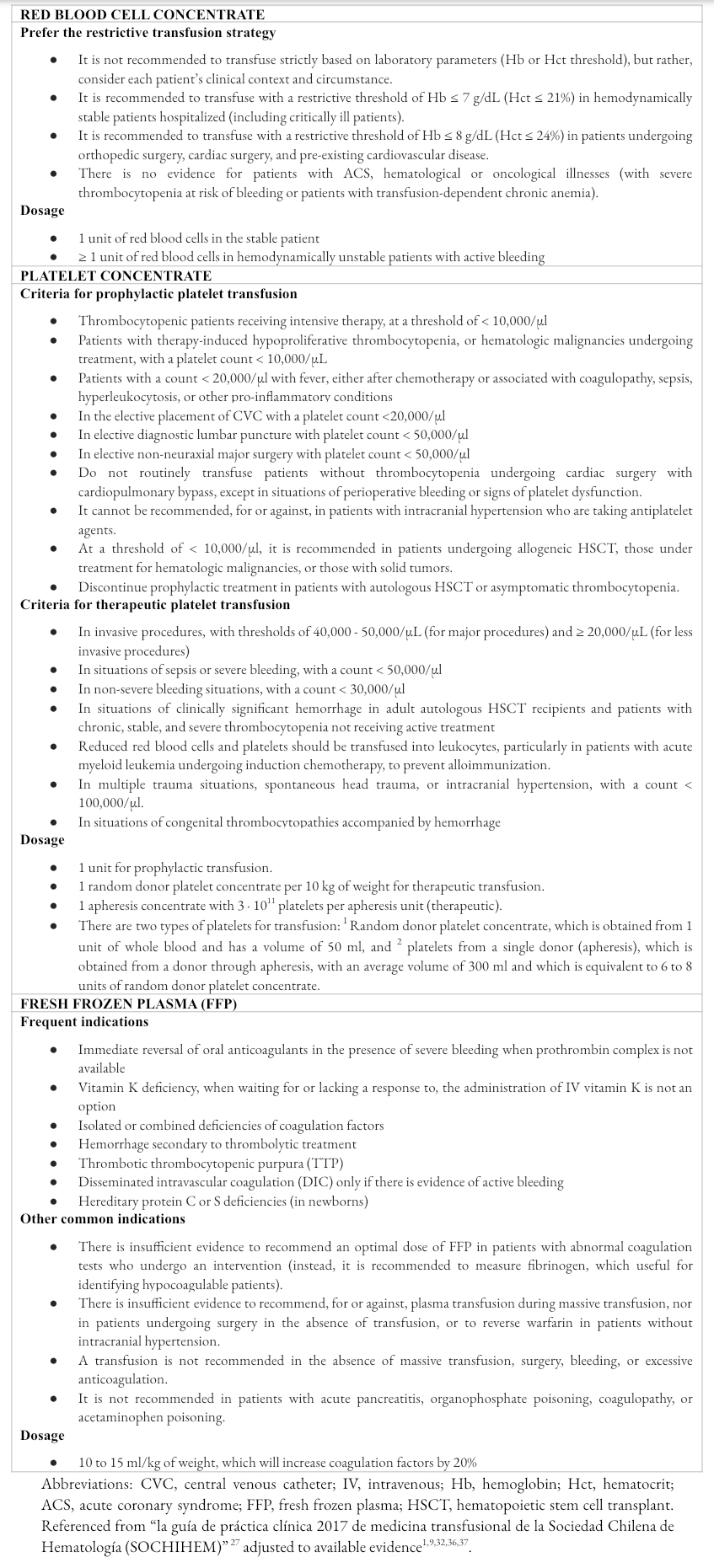 Full size
Full size Evidence-based recommendations for prophylactic correction of coagulopathies
Coagulopathy is a clinical concept defined as the inability to carry out hemostasis, involving a risk of bleeding, and does not depend on a specific laboratory abnormality. A study revealed that as chronic liver damage is accentuated, there is an increase in the capacity to generate thrombin[28], which could be translated as a hypercoagulable state (this is why they tend to generate a greater amount of thrombin). If this finding is compared with anticoagulant users, for the same INR (International Normalized Ratio), an individual with chronic liver damage may have a different hemostatic capacity than a patient anticoagulated with coumadins[28],[29], who could be in a hypocoagulable state. Therefore, clotting times do not reflect the true clotting ability of the patients.
On the other hand, in septic subjects, it is possible to observe a profile of alteration of the coagulation factors very similar to those who suffer from chronic liver damage; however, clinically, they may not present with coagulopathy, but rather a hemostatic dysfunction associated with the typical inflammation of sepsis. Hence, there is no documented benefit of transfusing plasma or platelets to individuals with altered clotting times or thrombocytopenia[30],[31].
Clotting times, then, have low or no correlation with hemostatic capacity, requiring a clinical definition for coagulopathy that includes situations such as severe thrombocytopenia (platelets < 20,000/μl), severe hypofibrinogenemia (< 100 mg/dl), and for the use of coumadin and/or NOAC (new oral anticoagulants)—circumstances that warrant prophylactic management, even in low-risk procedures. Other conditions such as thrombocytopenia <50,000/μl and the performance of invasive procedures should consider using platelet transfusion to prophylactically reduce the risk of clinically significant bleeding or achieve hemostasis in the face of active bleeding (Table 1)[27],[1]. Finally, there is no evidence of the benefit of using transfusions in antiplatelet users, so it is only recommended to use tranexamic acid or desmopressin in high-risk situations[32],[33].
Evidence-based recommendations for reversal of the effect of coumadin by fresh frozen plasma or vitamin K
In patients without bleeding who will not undergo an invasive procedure, an INR >3 is infrequently corrected (except when exceeding 7%). Vitamin K is the most widely used therapeutic agent to correct prolonged INR, used in 85% of cases, followed by fresh frozen plasma (43%) and prothrombin complex (35%)[5],[33]. Fresh frozen plasma is an allogeneic derivative that contains all plasma coagulation factors, including labile factors (Factor V and Factor VIII), albumin, and immunoglobulins[27]; the recommended dose of which varies between 10 to 15 mL/kg (providing a volume of 200 to 300 mL per unit) to reverse the effect of coumadin overuse.
Studies show that reaching an INR <1.5 and reversing this effect takes between 11 and 30 hours[34],[35], so it does not have an immediate effect. Fresh frozen plasma transfusions do not correct mildly abnormal coagulation tests and are associated with worse clinical outcomes in patients with bleeding that is not massive (Table 1)[36]. Although in the absence of bleeding, plasma is prophylactically transfused before surgical or invasive procedures in subjects at increased risk of bleeding[37], its usefulness in terms of prophylaxis remains uncertain since systematic reviews have shown no evidence in favor of its use in a variety of clinically important scenarios (including in critically ill patients)[38]; this has led to not having a posture as to whether or not to recommend its use in clinical practice, since there is no conclusive evidence[37].
On the other hand, the use of vitamin K to reverse the anticoagulant effect in cases of excessive anticoagulation would be enough to achieve an immediate partial correction[33],[5], without requiring the joint contribution of fresh frozen plasma, since it does not interfere with the correction speed of the INR[39]. The oral or intravenous route can be used, but the latter produces a faster initial response[33]. Anaphylactoid infusion reactions are extremely rare and can occur despite the recommended infusion time; on the other hand, documented thrombotic events are rare and bleeding complications are similar or only marginally reduced[40].
Administration of fresh frozen plasma is an intervention that requires a variable time of action and has an oscillating reversal efficiency. Given that its administration requires an infusion of large volumes, it is important to evaluate its use in subjects with significant risk for circulation overload, such as elderly patients with cardiovascular disease (Table 1). In bleeding situations due to excessive anticoagulation, it is advisable to administer vitamin K to achieve a partial correction[33],[40]. Consequently, the use of fresh frozen plasma is contraindicated to manage a patient with excessive anticoagulation and who is not bleeding since the probability of complications is greater[36], making the use of vitamin K preferable[33],[40].
Physiologic triggers for transfusion
Physiologic transfusion triggers are based on the measurement of clinical elements that globally assess the indications for transfusion of blood components, which could more effectively determine the optimal moment for transfusion to displace the current variables based on Hb levels[41]. These triggers include measurement of serum lactate, central venous oxygen saturation (SvO2 or ScvO2), abnormalities in the ST segment of the electrocardiogram (as a measure of regional tissue oxygenation), and simple hemodynamic variables such as heart rate and blood pressure (mean blood pressure or systolic blood pressure)[41],[42]. However, the most widely used variable has been SvcO2, with a nadir of 70% as a physiological indicator of oxygen tissue deficit[41], allowing the physician to evaluate the patient’s tolerance to anemia during blood loss since this variable involves the relationship between the flow of oxygen and oxygen consumption throughout the body[41].
Conclusions
Transfusion medicine is an area in constant progress, which develops and distributes guidelines that state the optimal conditions for transfusing blood components. It is based on the balance between the benefits and possible adverse outcomes that need to be avoided, making it a costly and complex therapeutic intervention since there is not strong evidence to define the safety profile for its use. Today there is a controversy between two trends to address the practice of red blood cell transfusion: a liberal strategy and a restrictive strategy. The latter was proposed as a safer strategy in most cases, even reducing the mortality of patients in specific subpopulations. However, in critical conditions such as ACS and cardiac or oncological surgery, the liberal strategy has shown fewer complications, even if used in the perioperative and in geriatric patients, which has led to the conclusion that this strategy can produce better results after its administration.
Despite this controversy, it has been observed that restrictive strategies do not increase or reduce the risk of mortality at 30 days compared to liberal strategies, which leads to an uncertain risk/benefit balance when transfusing at Hb values of 7.0 to 9.0 g/dl.
In regard to coagulopathies, coagulation times do not reflect patients’ true ability to clot since these variables have low or no correlation with hemostatic capacity, making their correction difficult. On the other hand, for the reversal of the effect of coumadin, the administration of vitamin K should suffice for an immediate partial correction in situations of bleeding due to excessive anticoagulation, preferring the intravenous route due to its rapid initial effect. The use of fresh frozen plasma is an intervention that requires a variable time for action and has oscillating reversal effectiveness. As it is associated with a greater probability of complications, its use has been displaced.
Finally, the use of physiologic triggers has been introduced to assess the optimal moment for transfusion in an attempt to displace the current arbitrary criteria based on Hb levels, of which the most widely used variable is SvcO2.
Notes
Roles of authorship and contribution
BAR: Investigation, conceptualization, writing of the article, critical review of its intellectual aspects and editing, general supervision and final approval of the full version. JVU: writing of the article and editing. PDM, JWI: writing of the article. MMR: Investigation, critical review of its intellectual aspects.
Ethicals
No requests or permits from an ethics committee were required to create this article.
Funding
The authors declare that there were no external sources of funding.
Conflicts of Interest
The authors have completed the declaration of conflicts of interest form of the ICMJE, and declare not having received financing for the realization of the report; not having financial relationships with organizations that could have interests in the published article in the last three years; and not having other relationships or activities that could influence the published article. The forms can be requested by contacting the responsible author or the editorial direction of the Journal.
From the editors
The original version of this manuscript was submitted in Spanish. This English version was submitted by the authors and has been copyedited by the Journal.

