Artículo de revisión
← vista completaPublicado el 15 de abril de 2025 | http://doi.org/10.5867/medwave.2025.03.3003
Dimensiones asociadas a competencias en telemedicina y telesalud en profesionales de la salud: revisión exploratoria
Dimensions related to telemedicine and telehealth competencies of health professionals: A scoping review
Abstract
Introduction Telehealth and telemedicine have proven to be useful in complementing face-to-face care, especially when long distances exist or when it is difficult to access specialists. New competencies are required to implement telehealth and telemedicine, not only in the use of technologies, but also in areas such as communication and ethics.
Objective To identify the dimensions associated with competencies in telemedicine and telehealth from the perspective of professionals in the area based on research developed in the last ten years.
Methods A Scoping Review was carried out by reviewing the WoS, Scopus, PubMed, and Scielo databases. The selection of publications included only original articles in both Spanish and English available under Open Access between the years 2013 and 2023.
Results The review identified twelve key dimensions in telemedicine and telehealth, highlighting “Technological knowledge in general and in telehealth technologies”, present in 25 papers. Seventeen papers addressed the dimensions of “coordination, cooperation and management”, highlighting the effective integration of multidisciplinary teams. Ethical competencies, professionalism and legal aspects, essential to guarantee privacy, informed consent and safety in telehealth, were also highlighted. Professionalism includes effective communication, technical skills and clinical reasoning, while safety encompasses data protection, promoting ethical and patient-centered care.
Interpretation The dimensions identified can guide researchers to better understand the competencies needed in the field of telehealth. Moreover, they can provide key elements for the development of a contextualized training framework leading to quality, flexible and more equitable remote care, responding to the needs of a society that is changing and adapting daily.
Main messages
- Identifying the dimensions of telehealth and telemedicine allows us to guide the definitions of the competencies that health professionals should have.
- Some limitations of this work are the lack of an in-depth study of specific aspects of technological implementation and the fact that the studies do not address the technical specificities or barriers associated with adopting certain technologies in different contexts.
- Identifying dimensions in competencies and the competencies themselves is a dynamic process requiring periodic review.
Introduction
Implementing telehealth and telemedicine is essential to expand access to health services, especially in remote areas where traditional medical care is limited. Information and communication technologies (ICT) also facilitate connecting and communicating between patients and health professionals, overcoming geographical barriers and improving accessibility to quality medical care [1,2]. Adopting telehealth has proven to be especially beneficial in emergencies and pandemics by safely providing continuous care, transforming the healthcare paradigm, and promoting a more flexible and patient-centered model. In this way, the health care of the face-to-face model can be complemented with virtual care [3], redefining the relationship between health professionals and patients. The evolution of telehealth highlights its positive impact on daily service delivery and the ability to provide continuous and accessible care, especially at critical times of global health [4,5,6].
Despite the many advantages and benefits of telemedicine and telehealth, they also face significant challenges related to access to technology, connectivity, digital literacy, and standards in safeguarding and transmitting clinical information. All these aspects are associated with data security, privacy, and confidentiality. In this context, the technological challenge and the acquisition of digital competencies represent one of the great challenges for the population, both for health officials and for adults and rural or isolated residents in particular [7,8]. These limitations highlight the need to address technological and social aspects to ensure a successful and equitable implementation of telehealth in diverse contexts and communities. This is not only from the patient’s perspective but also the health professionals' perspective [9].
To date, there is a gap concerning the areas of knowledge associated with the competencies that a health professional should have in telemedicine and telehealth. The objective of this review is to analyze and delineate the dimensions linked to telemedicine and telehealth competencies, according to the perspective of health professionals, based on the collection and evaluation of research conducted in the last decade.
Methods
This research corresponded to a systematic exploratory review of information, which followed the recommendations for exploratory reviews or Scoping Reviews [10,11].
The WoS, Scopus, PubMed, and SciELO databases were consulted for the information search.
The search was restricted to original articles. The publications' language was English and Spanish from 2013 to 2023.
The search algorithm used for the search was: [telehealth OR telemedicine] AND competence AND [health professionals OR health personnel OR medical personnel OR medical professional OR health care personnel].
In the case of the SciELO search, the same terms were used in Spanish since this database uses this language preferentially.
Any article that does not correspond to original research and that complies with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Scoping Reviews (PRISMA SCR) recommendations [12] was excluded from this study. Narrative reviews, systematic reviews, conference presentations, academic essays, books, and chapters were omitted. In addition, any article that was not under the Open Access modality was excluded from the research.
Repeated articles were eliminated from the works identified in the first stage due to the search algorithm. Then, we read the titles and abstracts to perform the first filter according to their relevance to the subject of this research. In the second stage, the inclusion and exclusion criteria were applied.
Results and discussion
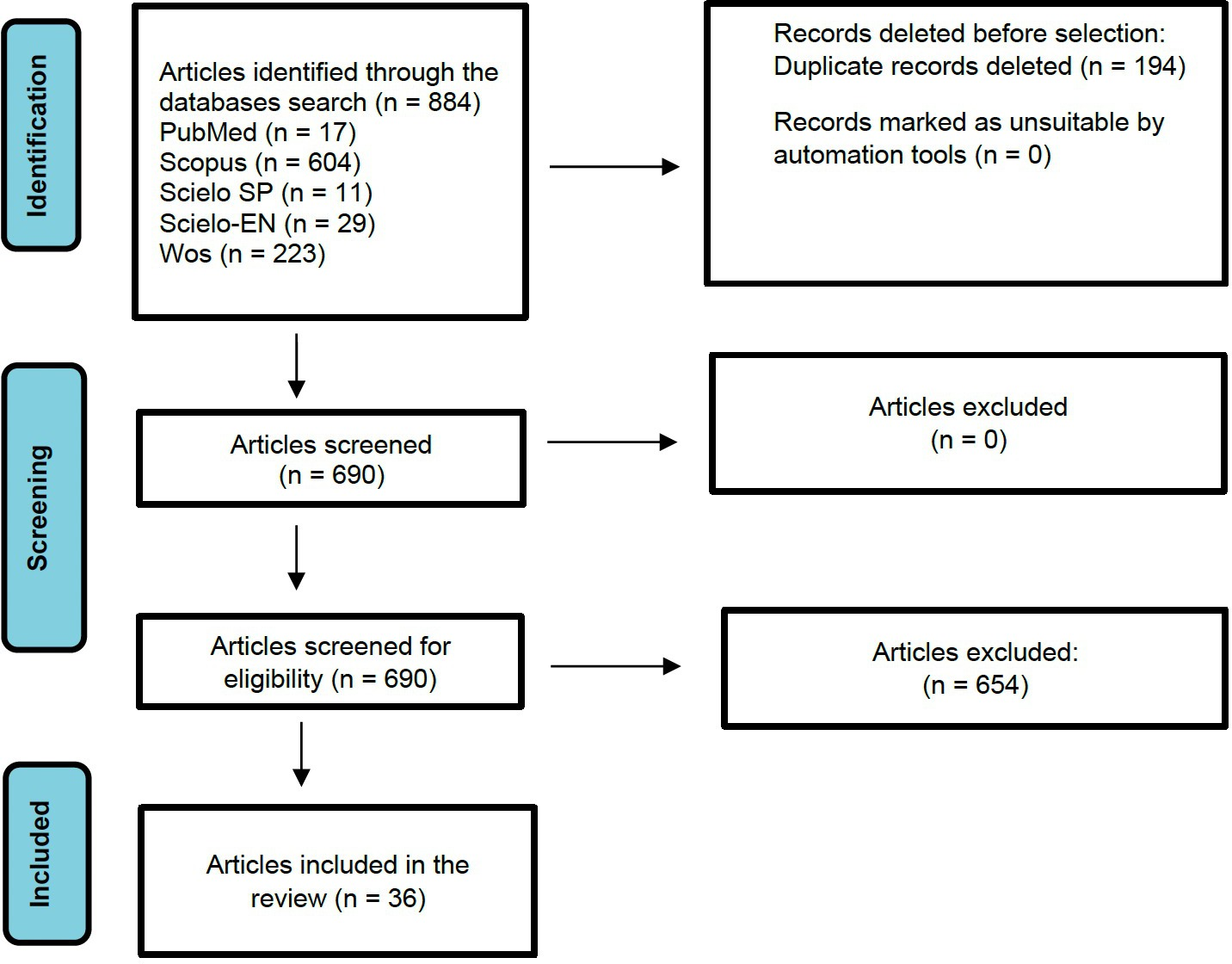
A total of 884 publications were identified from the database search. Of these, 36 articles were chosen based on the inclusion criteria of this study. Figure 1 summarizes the identification process, eligibility understood as originality, methodology and relevance, and inclusion of articles.
PRISMA flowchart.
The dimensions derived from the analysis of the articles reviewed are described below. These dimensions are associated with telehealth and telemedicine competencies (Table 1). A single article can contribute information to more than one dimension.
Technological knowledge in general and in the telehealth technologies dimension
The items associated with this dimension are 25. These allude to knowledge about informatics in general [13,14,15,16] and health informatics [14,15,16,17,18,19,20,21,22], of telemedicine modalities, knowledge of telemedicine platforms or virtual health care applications [15,16,18,22,23,24,25,26,27,28,29,30,31,32,33,34], as well as the ability to use them to provide health care effectively [17,20,29,30,31,33,35,36], and to solve problems related to their use in real-time [13,37]. Among the uses identified, working with electronic health records [16,21,26,28,28,36,38,39,40,41], participating in videoconferences for telemedicine [26,28,35,41], and using remote monitoring [26,28] stand out.
Coordination, cooperation, and management dimension
The review was associated with 17 articles that refer to coordination and cooperation as integrating health services of different types, including multidisciplinary health care teams. This allows interdisciplinary teams to work effectively, sharing competencies and knowledge, which makes it possible to better understand the health needs of users, together with managing available resources to provide comprehensive care [14,15,17,18,20,21,26,27,31,32,35,37,42,43,44]. In addition, management is mentioned as an important part of this area, where time management [27] and workload [27,43]; project and change management in health care [22]; data management, that is, the collection, evaluation, and analysis of data for decision making [15,32,33].
Ethical dimension, professionalism, legal aspects, and safety
The exploration was associated with 17 articles that identified ethics, professionalism [38], and legal and safety aspects as dimensions of competence development. It is required to consider knowledge, understanding, and respect for the legal, ethical, and political norms of privacy, consent, confidentiality, and information security associated with the practice of telehealth [13,14,18,21,23,24,25,26,27,31,41,42,43]. In addition to the above, professionalism is closely related to ethical behavior [45] and refers to the judicious use of communication, knowledge, technical skills, clinical reasoning, emotions, and values in the daily practice of telemedicine and telehealth [27,42].
Finally, these issues are closely linked to two aspects. First, security refers to safeguarding patient information in telemedicine [17,42]. Secondly, it is related to the need to have the knowledge and skills to ensure patient safety during online consultations concerning the management of emergency situations [27,46].
Education, training, and research dimension
The 15 articles were reviewed and associated with this dimension report the importance of education, training, and research. The authors indicate that this area refers to developing skills to train, educate, and develop a workforce for telehealth [16,35,47]. They also point to the value of updating knowledge about new technologies, approaches, and emerging practices in digital health care and the willingness to participate in training programs on the subject [15,17,21,23,36,40,41,43,48].
Research refers to the capacity and ability to develop research on telehealth services by collecting and analyzing electronic health data [15,22,30,37]. These data enable informed clinical decision-making and the generation of new knowledge from the analyzed data [30,47].
Virtual communication dimension
The study found 14 articles mentioning that virtual communication involves skills, abilities, and techniques associated with effective communication. It also relates to the practical, clear, understandable, consistent, and continuous interaction and exchange of information with patients, families, caregivers and/or members of the healthcare team through remote video and telephone platforms [13,14,17,19,20,23,25,26,27,38,42,45,46,47].
Some authors suggest that this exchange of information should involve eye contact techniques, facial expressions, and words of understanding and empathy [13,17,17,20,42]. They also mention that other strategies, such as recapitulation of key points, should be considered, as well as providing education and resources according to the patient’s literacy level. Likewise, adaptation to the patient’s communication style and establishing a trusting relationship characterized by listening and responding to the user’s needs [26,27,46] and responding to difficult or conflictive situations should also be considered. In addition, it is important to establish agreements with the patient [46], allowing users to make informed decisions about their medical care [47] and facilitating record-keeping of interactions [40].
Evaluation and improvement dimension
The characterization of this dimension reached 11 reviewed articles that identify evaluation and improvement as the development of skills for data collection and analysis focused on quality of care and treatment outcomes [35]. Likewise, they are oriented to the continuous evaluation of the effectiveness of care, analyzing the results of telemedicine interventions [25,26,32], the efficacy of such interventions [13,36], and the challenges and concerns associated with telehealth [17].
The goal of evaluation is stated as contributing to the adjustment of telehealth benefits [2] and to the improvement of the quality of medical care [22,32,36]. In addition, improvement is closely associated with understanding healthcare systems. Meanwhile, policies and regulations are linked to telehealth [22]. Identifying challenges is linked to telemedicine and telehealth, developing suggestions and recommendations [40], and establishing leadership systems that ensure quality care and patient safety [21].
Health care dimension
According to the literature review, health care is described in 10 articles as an aspect composed of several domains, such as the establishment of the patient/health care provider relationship [13], assessment in the clinical setting [19,23,24,46], patient capabilities [24,26], patient eligibility [24,26,27] and remote physical examination [46]; to these are added the exploration of treatment options and the negotiation of these with the patient [46]. Establishing the patient/healthcare provider relationship includes maintaining that relationship and addressing patient concerns, particularly among those with little experience in the use of technology [13].
Evaluation in the clinical setting refers to obtaining and managing clinical information remotely to evaluate patients based on the data provided and subsequent decision-making [19,23,24,46]. The above allows for planning treatments and interventions that consider the well-being of patients when using technology [24]. In addition, the importance of assessing the patient’s ability to use the technologies to participate in telemedicine care was identified [24,26] to adapt the interventions to the patient’s abilities. Similarly, the assessment of patient eligibility is also considered. That is, identifying which patients are suitable for telemedicine and telehealth and which require face-to-face care, according to the severity of the disease, technological capacity [24,26,27], and specific care needs [27].
Another aspect to consider associated with care is the performance of the remote physical examination. In this regard, it is necessary to evaluate the feasibility and effectiveness of remote physical examination techniques and guiding patients in self-examinations in a teleconsultation [46]. In addition, the need to explore treatment options and negotiate them with the patient was identified [41,46] in defining and guiding treatment decisions through telemedicine. Finally, as part of care, the ability to record and document remote clinical encounters and their management was identified [15,46].
Adaptability dimension
The review found 10 articles mentioning that the implementation of telehealth involves different environments, settings, and resources. In this sense, adaptability is related to how health professionals are linked to change, which is necessary for the willingness and ability to adapt to it [17,23]. On the other hand, it is considered necessary to adapt the preparation of the consultation environment and the provision of care through telemedicine and telehealth to provide care in virtual environments [24,38,46]. This, in turn requires consideration of local contexts [25], in dimensions such as patient assessment [18,19], as well as communication skills, due to limited nonverbal cues [42].
According to the review, multiple situations could affect the implementation of telemedicine and telehealth. In this context, identifying and addressing the barriers and limitations that may arise from remote clinical practice to resolve and adapt to what is required is identified as relevant [25]. Similarly, a willingness to adapt to new technologies is required [26] to learn and adjust practices with innovative telemedicine and telehealth technological tools [17,23,26,40].
Telehealth knowledge dimension in general
From the review, six articles mention that telehealth knowledge is related to the principles, concepts, and practices of telemedicine and telehealth. This knowledge is linked to the use of technologies as well as procedures. The latter include diagnosis, remote communication, care policies and protocols, treatment, registration, remote patient registration, monitoring, follow-up, and other related services [21,27,37,39,43,46].
The reviewed literature associated five articles mentioning digital and health literacy in two aspects. First is individuals' ability to understand, evaluate, and use health information to make informed decisions and promote health [47]. Second, it refers to the ability to help others understand and use telemedicine technology and health information effectively [26,31], as well as the ability to teach. This involves transmitting acquired knowledge and skills to healthcare workers [25]. This knowledge includes telemedicine concepts, digital health applications, and digital medical record management [17].
Four articles describe culturally competent care as delivering culturally effective care. This should involve understanding, awareness, sensitivity, respect, ability to adapt and be responsive to the health needs of the diverse local cultures that may be present in the population being served [18,35,41,43]. This is linked to consideration of the social determinants of health specific to each community and may influence healthcare needs [18]. Culturally competent care considers the beliefs, knowledge systems, resources, medicinal practices, and disposition toward technology that diverse cultures have [18], as well as social class, sexual orientation, ethnicity, age, religion, and nationality [43].
The review identified four articles that point out that awareness and attitude toward telemedicine refers, on the one hand, to health professionals' knowledge regarding the existence and benefits of telemedicine [29]. In addition to understanding what telemedicine is, one must understand its scope, regulations [40], and challenges [25,29].
On the other hand, it includes a positive attitude towards telemedicine and telehealth and the recognition and acceptance of its importance in certain contexts, such as the COVID-19 pandemic and health care in general [29,40]. This is relevant to improving efficiency [16,29], quality [16], and safety in health care delivery [29].
Some limitations refer to the lack of in-depth study of specific aspects of technological implementation. Although the importance of technological adaptability is highlighted, the studies do not address the technical specificities or barriers associated with adopting certain technologies in different contexts.
Conclusions
The successful implementation of telemedicine and telehealth implies the adoption of specific technologies and the continuous training of health personnel in using these tools. The flexibility of health systems and the ability to adapt to users' changing demands and needs are essential to providing quality care and improving the patient experience in the digital environment.
The findings of this review show an evolution and multidimensionality in terms of the skills and knowledge required to carry out telemedicine and telehealth care, suggesting the importance of continuing education in this area. The dimensions derived from the areas of knowledge analyzed in this review help us understand that the reality in the field of telehealth and telemedicine is diverse and complex. Likewise, identifying the twelve dimensions leads us to conclude that a broad vision is required to see the integral panorama of the areas where new competencies need to be developed. This highlights the importance of a contextualized framework to ensure quality remote care that reflects society’s changing needs.
In summary, for telehealth and telemedicine to be effective and sustainable, a comprehensive approach that encompasses technological adaptability, effective communication, continuous education, ethical compliance, cultural competence, appropriate coordination, and a positive attitude toward innovation is needed. These combined elements ensure that telehealth is a viable alternative to face-to-face care and improves the accessibility and quality of overall healthcare.

