Artículo de revisión
← vista completaPublicado el 16 de enero de 2025 | http://doi.org/10.5867/medwave.2025.01.3014
Un análisis sistemático de la literatura sobre la condición post-COVID-19 en América Latina centrado en la epidemiología, las características clínicas y el riesgo de sesgo
A systematic analysis of the literature on the post-COVID-19 condition in Latin America focusing on epidemiology, clinical characteristics, and risk of bias
Abstract
This analysis article aimed to identify and analyze all articles published on the post-COVID-19 condition in Latin America and the Caribbean, focusing on epidemiology, clinical characteristics, and risk of bias. We did a systematic survey of the literature with broad inclusion criteria. The only exclusion criteria were articles referring to post-acute COVID-19 sequelae after an intensive care unit stay, which we distinguish from the post-COVID-19 condition. We searched MEDLINE/PubMed, LILACS, SciELO, Scopus, Web of Science, and Epistemonikos. We included 55 records, of which 48 were original articles (44 were observational research, 29 of which had a comparison group; and four reviews). Various definitions for long COVID were reported, or none, and few used the World Health Organization criteria. None of the included studies reported prevalence rates for the region. We extracted the reported signs and symptoms of long COVID for our region. Using the Johanna Briggs Institute critical appraisal tools for observational analytic research, we found that most included studies were prone to limitations and biases. We conclude that more research should be done on the post-COVID-19 condition in Latin America and the Caribbean, using rigorous study designs to inform public health strategies.
Main messages
- Ours is the first study to comprehensively search and assess any report on the post-COVID-19 condition in the Latin American region.
- We found that most studies lacked robust epidemiological designs.
- The true prevalence and incidence of long COVID-19 is still unknown in the region.
Background
According to the WHO COVID-19 dashboard, over 775 million cases of COVID-19 have been reported worldwide at the time of writing this article. Latin America and the Caribbean are among the regions with the highest excess deaths per 100,000 population. Throughout the pandemic, differences have been observed between countries and regions concerning incidence and case-fatality rates, partly due to the different response strategies deployed by governments, differences in health system capacity and quality, and the robustness of national health statistics. With this large number of cases and a high rate of undetected and underreported cases, any sequelae or persistence of symptoms will burden already strained health systems. Additionally, there are still many unknowns regarding this new disease’s medium- and long-term consequences.
Most patients overcome acute COVID-19 and return to their baseline pre-COVID-19 state, but an unknown proportion continues to report health problems. This altered health status after COVID-19 has been referred to by the World Health Organization (WHO) as a post-COVID-19 condition and, as of September 2020, has been listed in the ICD-10. The Pan American Health Organization calls for recognizing this condition, rehabilitating patients suffering from it and conducting research to close knowledge gaps.
In 2021, the WHO convened a panel to agree on a definition of this morbidity and concluded that post-COVID-19 is a condition that occurs in adults with a probable or confirmed history of SARS-CoV-2 infection, in which symptoms persist beyond three months after the first symptoms of COVID-19, lasting for at least two months and cannot be explained by any alternative diagnosis [1]. Another feature of persistent COVID-19, also called long COVID, is that it can have a fluctuating course (with changes over time in quantity or quality) and with relapses and remissions (symptoms returning after a period of improvement) [1,2]. This definition does not consider post-acute sequelae of severe COVID-19.
The frequency, characteristics, and duration of persistent COVID-19 symptoms are unknown, a knowledge gap that must be addressed. Good-quality evidence is required to understand the prognosis, validate and adjust individual treatments, and develop public policies to address this problem. Since the first cases were identified in 2020, several efforts have been made to estimate the proportion of patients with COVID-19 who might develop prolonged symptomatology and the prevalence of this condition in a given population.
In any case, the results of the studies that have evaluated the prevalence of long COVID-19 in different populations are markedly heterogeneous. Consequently, the current available empirical evidence makes it impossible to estimate the true disease prevalence. The populations studied so far are mainly case series of hospitalized patients followed up after discharge, and few studies have been conducted in the community. Finally, the dynamics of waves, variants and vaccination also affect the clinical outcomes of COVID-19, including its persistent condition and the sequelae it may leave.
Given this landscape, we deemed it important to survey the literature on the post-COVID-19 condition in Latin America and the Caribbean. We aimed to identify and characterize the articles published on this condition, focusing on research regarding epidemiology and clinical characteristics. The scope of this analysis paper is broad as it is intended to further our understanding of the gaps in the literature and the methodological shortcomings of the research designs used to study this condition.
Methods
Using broad inclusion criteria, we systematically surveyed the published literature on the post-COVID-19 condition referring to Latin America and the Caribbean. The inclusion criteria were any article type published either in local, regional or international journals from the inception of the pandemic to the date of the last search. The only exclusion criteria were articles referring to post-acute COVID-19 sequelae after an intensive care unit (ICU) stay.
We searched the following databases with a cut-off date of 17 March 2024: MEDLINE/PubMed, LILACS, SciELO, Scopus, Web of Science, and Epistemonikos. We used the plain text terms "Long COVID" and "Latin America". For these terms, PubMed created the following search strategy with synonyms and MeSH terms:
("post acute covid 19 syndrome"[MeSH Terms] OR ("post acute"[All Fields] AND "covid 19"[All Fields] AND "syndrome"[All Fields]) OR "post acute covid 19 syndrome"[All Fields] OR ("long"[All Fields] AND "covid"[All Fields]) OR "long covid"[All Fields]) AND ("latin america"[MeSH Terms] OR ("latin"[All Fields] AND "america"[All Fields]) OR "latin america"[All Fields])
We did not limit our search by field, time intervals, or language to increase the sensitivity and comprehensiveness of our search. We manually searched the contents of Latin American medical journals indexed in MEDLINE according to a list of journals previously published by Bachelet et al. [3]. Additionally, we included medical journals from Brazil. The manual search was done with the terms' Long Covid,' 'Covid prolongado', and 'Covid persistente' in the search box of each journal’s website. We identified articles mentioning these terms in any section—title, abstract, or full-text—for subsequent screening and inclusion. To increase the sensitivity of our search, we also perused the references of the included articles.
We added all the identified articles to Zotero (Corporation for Digital Scholarship, USA) for screening, selection, and removal of duplicates. One of the authors (BC) screened the identified documents for eligibility. When it was unclear whether a document should be included in this survey, BC consulted with VCB, and a consensus was reached.
BC and BM extracted the following items from the included documents: author’s last name, year of publication, the title of publication, country of the first author, country of the corresponding author, whether the authors were part of an international collaboration, journal name, whether the journal was regional, language of publication or if available in more than one language, and article type (commentary, original article, letter to the editor).
Original articles were further extracted to know whether they were primary studies or review articles. Primary studies were categorized as having an analytical or descriptive design. Analytical studies were further classified as cross-sectional, cohort, or case-control following the Schulz and Grimes classification of types of clinical research [4]. We extracted the aim, the definition of long COVID-19 (none, own, WHO [1], NICE [5]), population characteristics, context (time, place), data sources used, whether patients had a history of hospitalization due to COVID-19, sample size, symptoms (grouped and classified by organ systems per Natarajan et al. [6]), and main results. We noted prevalence rates when reported. Meetings were held where VCB reviewed the extraction process, resolved doubts, and checked for errors or possible misinterpretations.
We assessed the quality of the included primary studies using the Johanna Briggs Institute Critical Appraisal Tools [7]. Specifically, we used the cohort, case-control and cross-sectional checklists. BC and BM independently assessed each primary study and reached a consensus and, when this was not possible, VCB resolved discrepancies.
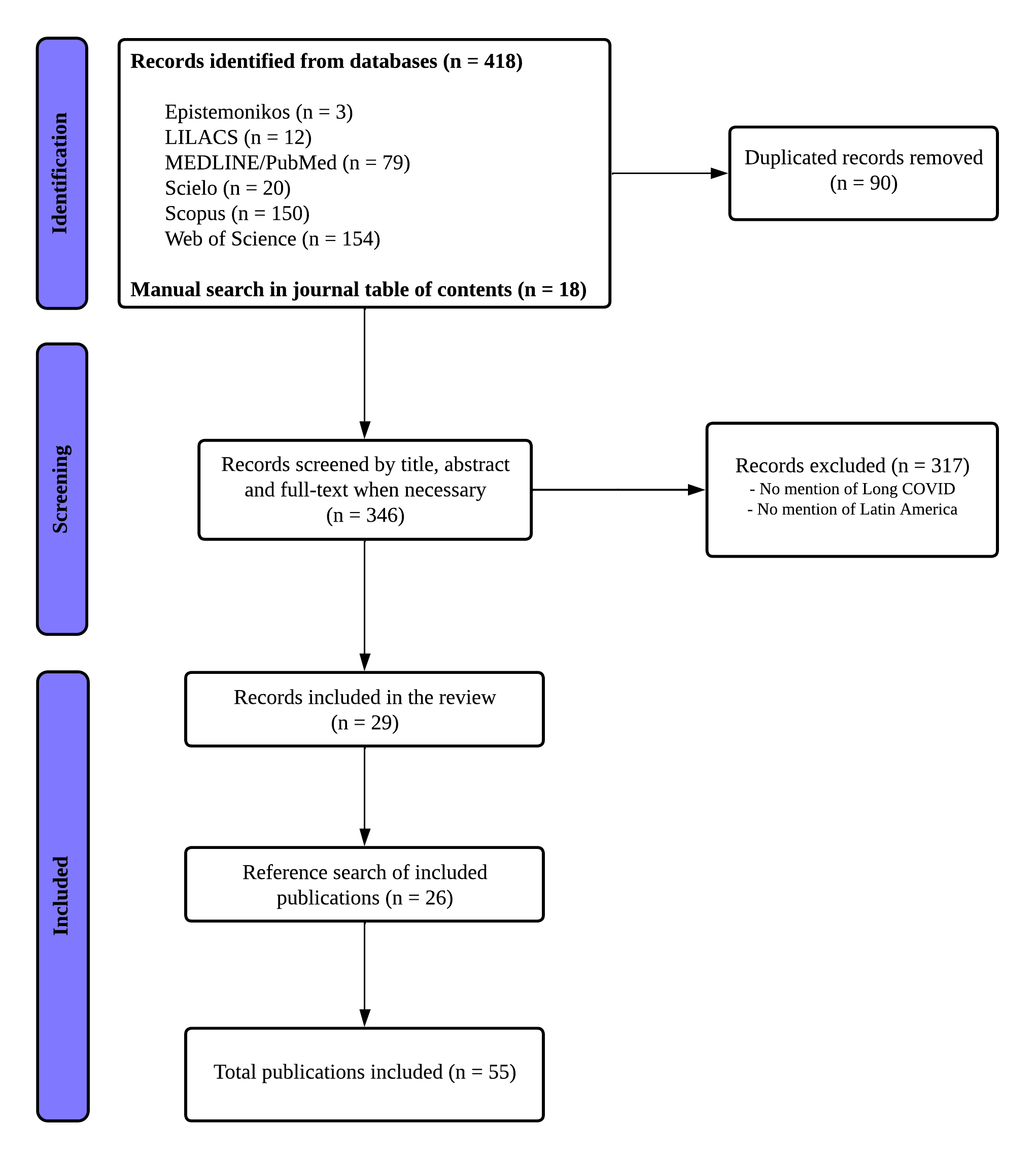
A PRISMA flowchart was done to present the identification, selection and inclusion process. Evidence synthesis was done narratively, and summary tables were created to characterize the population of included documents.
Synthesis of findings
Figure 1 shows the PRISMA flowchart for identifying, screening and selecting the included articles. After searching the databases and journals and identifying 346 eligible studies, we screened for mention of long COVID and Latin America, resulting in 29 studies wherein we searched the references of each article, which allowed us to identify another 26 articles, thus totaling 55 studies included for this review (for a list of included articles, please refer to online supplementary file ). The 55 finally included articles are described in Table 1, and the complete data extraction Table 1 also available in supplementary files.
PRISMA flowchart.
Regarding the risk of bias, we found that, in general, cross-sectional studies had shortcomings with practically all of the JBI domains for critical appraisal (Table 2). Conversely, the small sample of cohort studies showed mainly selection bias, attrition, and insufficient follow-up (Table 3).
Of the 29 analytical observational studies, only five explicitly stated that the study aimed to estimate the prevalence of post-COVID-19 symptoms, cognitive decline, or epidemiology and to associate with age, pre-existing comorbidities, and possible risk factors. Two of these five were cross-sectional, and three were reported as cohort studies. The remaining studies focused on describing patient characteristics and symptoms by age or sex, evaluating functional capacity, impact and sequelae, investigating central nervous system manifestations, and exploring other associations.
Nine studies included their own definition of long COVID-19, seven did not report a definition, four used the WHO definition, and two used the NICE definition.
None of the studies included in this survey reported prevalence rates, although some did provide percentages of patients with symptom persistence after variable periods of SARS-CoV-2 infection confirmation.
The reported symptoms were diverse, with varying terminology used to describe similar manifestations. A total of 57 symptoms were identified across the included analytical studies (Figure 2).
Ring diagram representing persistent COVID-19 symptoms reported in the included articles grouped by organ systems.

Brain fog includes thinking, memory and concentration impairments; Cognitive impairment includes language, visuospatial temporospatial and verbal fluency impairments; Sleep disturbances includes sleep latency, daytime sleepiness, sleep efficiency, sleep apnea and insomnia; Fatigue englobes asthenia, extreme fatigue, fatigability, persistent fatigue; Arthralgia includes joint pain and joint discomfort; Myalgia includes muscle pain and muscle discomfort; Movement disorders includes gait impairment, difficulty walking, exercise intolerance, physical capacity, difficulty with movement, difficulty exercising; Alopecia includes hair loss and telogen effluvium; Rhinorrea includes congestion and runny nose; Edema includes generalized, limbs and palpebral; Sking problems include skin problems not specificated, skin rashes and urticaria; General pain includes abdominal pain, chest pain, facial pain, muscle cramps and odynophagia; Sexual disturbances include erectile dysfunction, decreased libido, menopause alterations; Anxiety include anxiety disorders, agoraphobia, generalized anxiety, panic disorder, social phobia; Otolaryngological disturbances include hoarseness, dysphonia, aphonia, tinnitus and vertigo
Source: Prepared by the authors based on study results.
Analysis
With a cut-off date of 17 March 2024, we found 55 published reports on long COVID-19 in Latin America and the Caribbean, of which 29 were observational studies with a comparison group. None reported prevalence rates. Two studies on the Mexican population were published after our search cut-off date. The first reported a 20.9% prevalence of long COVID-19 in a sample of 804 participants after a first COVID-19 infection [63]. Using the NICE definition and a robust probabilistic sampling strategy to estimate prevalence rates in a representative sample of the Mexican population, the second one reported an overall prevalence of 4.67% (95% confidence interval, 4.32 to 5.02) [64].
Overall, there is a paucity of epidemiological research estimating the impact of the post-COVID-19 condition in the Latin American region. Given that testing has dropped to a minimum, it is becoming increasingly difficult to estimate the burden of disease carried over from the pandemic years, as well as detecting which current cases of COVID-19 are resulting in prolonged symptomatology. Since this condition is ultimately a diagnosis of exclusion, there is a reasonable case to be made for patients with indeterminate symptoms who contact health systems and might not be diagnosed or treated for this new condition.
Efforts are being made in other higher-resourced settings to understand the full spectrum and impact of the post-COVID-19 condition. Australia [65], France [66], India [67], Japan [68], Netherlands [69], Scotland [70], and the United States [71,72,73,74,75,76] have carried out cross-sectional, population-based estimations of prevalence and associated risk factors. Some of these studies [71,72,77], as well as one from Mexico [63], have also looked into the interesting implications of high vaccination rates on the occurrence of post-COVID-19 symptoms, mostly finding that the proportion of patients who report having a COVID-19 infection or reinfection and who subsequently report prolonged symptoms, drops significantly when fully vaccinated.
While clustering symptoms facilitates a more structured understanding, this approach may result in a loss of specificity [78]. Nonetheless, in our study, we grouped signs and symptoms using a classification similar to that of Natarajan et al. [6] to enhance comparability. The signs and symptoms reported in our included studies are consistent with findings from previous research [6], where fatigue, pain, and cognitive dysfunction (commonly referred to as “brain fog”) were the predominant symptoms.
Our research has important implications regarding the methodological limitations of many of the included studies. We found that observational analytical research was prone to bias. This is consistent with a methodological umbrella review of systematic reviews that assessed biases and limitations in observational studies of long COVID-19 prevalence and risk factors [79]. In the reviews that reported risk of bias assessment for the included primary studies, this overview found that the quality of outcome ascertainment and selection bias were the most frequently ranked biases, followed by deficiencies in adjustment for confounders, attrition and representative sampling. The authors offer recommendations for mitigating biases in persistent COVID-19 studies regarding confounding (controlling for common confounders, using electronic health records and ongoing prospective cohort studies, including comparator cohorts), selection bias (doing representative sampling or consecutive recruitment strategies, reporting response rates or attrition, using statistical methods for matching cases), measurement bias (documenting time zero and duration of follow-up, using confirmatory testing for SARS-CoV-2, avoiding self-reporting), and outcomes selection (using validated symptom and impact scales, referring to consensus definitions).
Our analysis has limitations. Comprehensiveness came at the cost of including many reports that did not report research results, given that we aimed to gauge the extent to which post-COVID-19 condition is being addressed in the scientific literature of our region. Ongoing research means that more and more reports are now being published with increasingly interesting results that emerge from more robust methods than those used in the early years of the pandemic. We did not attempt to report prevalence rates for the region because of the heterogeneity of the article types, research designs, and definitions used for long COVID. We were also limited by the conflation between sequelae stemming from ICU stays and symptom persistence, which made the study selection process more difficult. The absence of specific confirmatory diagnostic tests and a lack of validated scales to follow up on potential cases of long COVID-19 also create a confusing scenario that underscores the case for more research to be conducted on the aftermath of a SARS-CoV-2 infection.
Conclusions
Understanding the post-COVID-19 condition better is needed, especially regarding its epidemiology in Latin America and the Caribbean. Among the studies included in our review, we found heterogeneity of research designs, inconsistent definitions, and overall methodological limitations, highlighting the challenges of accurately characterizing this condition.
We found no reports on prevalence rates in the included articles, although this is likely to change as further research is conducted and published. Since prevalence rates reflect the disease burden, the absence of quality data presents a significant challenge for health systems. Understanding the impact of this condition on the population is crucial for effective health service planning. Future studies in the region should prioritize employing robust and representative sampling strategies to address these gaps.

