Artículo de revisión
← vista completaPublicado el 27 de octubre de 2025 | http://doi.org/10.5867/medwave.2025.09.3096
Cambio climático y salud: trayectorias de vulnerabilidad y políticas de resiliencia
Climate Change and health: vulnerability pathways and resilience policies
Abstract
Climate change is a serious threat to public health. The intensity and devastation of 21st-century climate events exacerbate the vulnerability of certain social groups that already face historical disadvantages. The objective of this article is to examine various dimensions of health vulnerability in the context of anthropogenic climate change. A narrative review was conducted based on articles published in the last five years from the Scopus, Medline/PubMed, LILACS databases, and an intentional search of current publications by international organizations and commissions focused on the topic. The review identified and characterized four types of health vulnerability dimensions: social, economic, geographic, and health infrastructure; it also presents multiple intersectionalities that converge at the interface of climate change and health which increase the risk of physical and mental illnesses. Based on the proposed discussion, public policy guidelines are suggested for resilient health systems and effective information structures for timely decision-making.
Main messages
- Climate crises intensify risk scenarios for the spread of physical and mental illnesses.
- Climate change accentuates pre-existing conditions of vulnerability that are configured in social, economic, geographic and health infrastructure dimensions. These health vulnerabilities are intensified in the multiple intersectionalities of class, gender, ethnicity and population mobility.
- This work provides evidence for health systems and their professionals to anticipate and respond promptly to current and future climate crises, prioritizing groups particularly affected by aggravated trajectories of inequity.
Introduction
Climate change represents one of the greatest global health challenges of the 21st century [1,2]. Although the Earth has shown warming and cooling patterns over hundreds of thousands of years between glacial and interglacial periods, the Anthropocene marks a turning point in temperature increase. This is mainly due to greenhouse gas emissions intensified by the preponderant production, distribution and consumption model since the middle of the 20th century, in which the burning of fossil fuels and changes in land use stand out [1,3,4]. Thus, global temperature has reached levels not recorded in at least the last 2000 years [5]. In 2024, the annual average temperature of the Earth’s surface broke a record with 1.45 degrees Celsius more than in pre-industrial times [6], dangerously approaching the incremental limit of 1.5 degrees Celsius. This is the threshold for irreversible damage to ecosystems and human health [7,8,9].
The anthropogenic influence on global warming is associated with increased intensity and frequency of atmospheric phenomena that become extremes [10] manifested in heat waves, prolonged and multi-year droughts, hurricanes and torrential storms, continuous rainfall, sea level rise and severe flooding [5,6,11,12,13,14]. These events have the potential to reconfigure the ecosocial relationships of urban, rural and coastal territories, generating impacts on human health and aggravating pre-existing vulnerabilities or installing new ones [15,16,17].
Although the impacts of climate change on the physical and mental health of human beings have been widely documented, there is a knowledge gap regarding how these impacts are distributed among vulnerable populations. These include children and adolescents, women, indigenous peoples or ethnic minorities, people with pre-existing diseases, people living in poverty, migrants and refugees [18]. To understand this complexity and its relationships, health and environmental approaches [19,20,21], as well as the ecosocial perspective of epidemiology [22], are fundamental.
This review aims to explore different dimensions of health vulnerability to anthropogenic-influenced 21st-century climate change. The work contributes to the understanding of health and disease processes related to global warming, emphasizing vulnerabilities. In addition, it provides evidence for health systems and their professionals to anticipate and respond promptly to current and future climate crises, prioritizing groups especially affected by aggravated inequity trajectories.
Methods
For this review, publications from 2020 to 2025 were considered. In the first instance, the search was conducted through Scopus, MEDLINE/PubMed and LILACS, using the following combination of English and Spanish descriptors: climate change and health vulnerability. We included open-access full-text published articles, human studies and publications in English, Spanish and Portuguese. The study designs selected were systematic reviews, meta-analyses, prospective and retrospective longitudinal studies, interdisciplinary and collaborative global monitoring, narrative and literature reviews. The reasons for exclusion were mainly secondary approaches to the category of climate change, focused case studies, analysis of risk to a single disease, analysis focused on a specific city, analysis of environmental problems unrelated to anthropogenically influenced climate change, articles without evidence of risk in vulnerable groups, and repeated articles.
Secondly, an intentional search was carried out for reports, books and documents from international organizations and commissions related to the analysis of climate change and health that might have been excluded in the initial search. A total of 10 additional documents were incorporated.
Results
Before presenting dimensions of health vulnerability to anthropogenic conditions of climate change, the first section of results specifically showed the relationships of some extreme climatic events with the risk of disease in humans. It should be noted that these relationships are immersed in a broader complexity of causal chains, derived from the current economic model anchored on fossil fuels. This model has generated serious environmental and social externalities as well as patterns of inequity, especially since the second half of the 20th century [10,23].
Climate change and human health risk scenarios
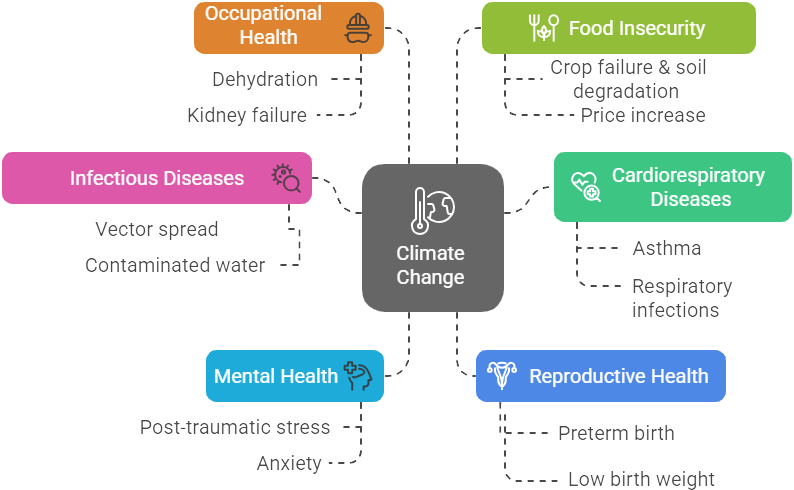
The associations between climate change and the physical and mental health of human beings are indisputable. Extreme changes in temperature, humidity of the environment and air toxicity derived from fires are the pathways for cardiorespiratory diseases, infectious diseases, skin diseases and allergies [6,12]. Heat stress leads to complications in fertility, pregnancy and perinatal outcomes, increases the risk of preterm birth and affects maternal mental health [1,4,9]. Extreme heat exacerbates the physical conditions and resistance of those workers whose work is performed outdoors (construction workers, farmers, street traders), who may present cases of dehydration and renal failure [6,24]. Intense heat causes sleep disorders, as some houses retain heat indoors [6,12]. Climate change is also a driver of food insecurity [25,26]. During 2022, compared with the period from 1981 to 2010, an additional 121 million people were reported to be moderately or severely food insecure, associated with droughts and floods attributed to climate change [6,12]. On the mental health level, heat waves and extreme weather events are triggers of post-traumatic stress and anxiety disorders [17].
Anthropogenic global warming has contributed to an increase in atmospheric humidity and precipitation intensity [5]. These generate floods and stagnant water deposits, which are favorable for the proliferation of dengue, vibriosis, leptospirosis or cholera [25]. Temperature variations, together with intensive agriculture, land use change and accelerated urbanization processes, favor the survival and geographic expansion of some vectors [27,28]. Thus, the average annual transmission risk of Aedes Albopictus and Aedes aegypti increased by 46 and 11%, respectively, in the period from 2014 to 2023 in relation to the period from 1951 to 1960; intensifying diseases such as dengue, zika and chikungunya. The extension of spaces suitable for the reproduction of the Plasmodium Falciparum vector increased by 17% from 2014 to 2023, compared to 1951 to 1960, and by 28% for the transmission of Plasmodium Vivax that generates malaria [6] (Figure 1).
Climate change and human health risk scenarios.
Dimensions of climate change and health vulnerability
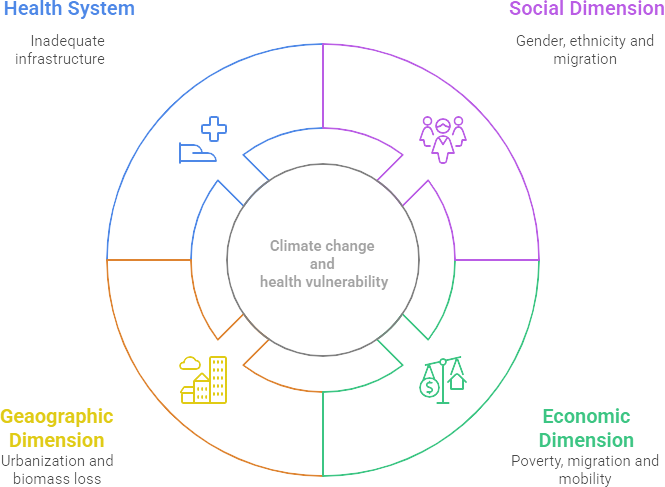
The impacts of climate change on health are not linear, nor are their trajectories of equal magnitude. The dynamics of climate change accentuate pre-existing structures of inequity and vulnerability of certain populations [29]. In this sense, this review made it possible to identify four dimensions of vulnerability that shape the conditions of disease distribution in the context of climate crises. The proposed dimensions are of a social, economic, geographical and health infrastructure nature.
Social dimension
Approximately 70% of people living below the poverty line are women and climate change is an aggravating factor in this situation [1]. The results show biologically and socially produced gender pathologies due to climate change. That is, by their social condition, gender or by the same female physiology and metabolism in the face of heat adaptation [16]. In pregnant women, evidence shows that exposure to excessive heat negatively impacts maternal health. In addition, there is a significant association between heat exposure and reduced gestational age, increased risk of preterm delivery and low birth weight of the newborn [30,31,32,33]. On the other hand, mortality and morbidity due to excessive heat is higher in women older than 65 years compared to men [34]. In Europe, between May and September 2022, 61 672 heat-related deaths were recorded in 35 countries. Among these, 56% more deaths were evident in women than in men [35].
Women in low-income countries and rural territories are particularly affected by global warming. According to the United Nations, UN Women, 158 million women and girls could be impoverished by 2050 in the worst-case scenario of climate change [36]. Women who depend on agricultural activities are particularly vulnerable to climate change, accounting for 49% in low-income countries. Intensified droughts and floods modify agricultural cycles and destroy crops. In this sense, climate change is related to food insecurity and the loss of female sovereignty in food production and consumption [37,38].
Exposure to extreme climatic phenomena, in addition to other political and economic determinants or those related to internal conflicts, would increase the probability of the occurrence of forced or voluntary displacement [6]. Migration processes and their conditions could increase the health vulnerability of migrant populations, given that natural disasters are associated with outbreaks of diseases aggravated by the collapse of health infrastructure. These pathologies include malnutrition, infectious diseases and morbidity and mortality linked to heat stress and mental health problems [39].
Economic dimension
Poverty is the most potent lever of disease, as it generates processes that destroy the health and well-being of human beings [40]. Impoverished populations that experience greater adversity due to historical processes of inequity in the distribution of basic resources and systematic racial segregation are at greater risk of harm. Similarly, they face serious challenges in addressing global warming and associated extreme weather events [10,41].
Outdoor workers suffer directly from the effects of heat waves. They are generally a marginalized and vulnerable population: migrant farmers, street vendors or construction workers who, with no alternative in the formal labor market, are directly exposed to high temperatures [42]. Occupational mortality related to intense heat is 35 times higher among agricultural workers compared to workers in other industries. Longitudinal studies in the United States showed that 20% of heat-related deaths among non-US citizens occurred in agricultural fields where a majority of the migrant population worked [41].
Fragile housing infrastructure is another vulnerability factor. Precarious building materials, such as thin or tin roofs and a lack of equipment to condition the air during heat shocks, generate thermal accumulation, which leads to stress and sleep disorders [42]. The fact that low-income people cannot afford the costs of adapting the temperature of their homes means a situation of energy poverty that leads to physical and mental health risks [43,44].
The economic impacts attributable to climate change affect people’s livelihoods, especially those linked to agriculture, forestry, fisheries, energy and tourism. In the face of extreme weather events, abrupt losses of infrastructure, housing, water and food systems also increase health risks [10,45].
Some articles emphasize climate injustice. Low-income countries emit less greenhouse gas than developed countries. However, they are particularly impacted by climate change [46,47]. Latin America is responsible for 8.3% of total greenhouse gas emissions [23]. However, due to its conditions of social and environmental inequity, added to the global impacts of anthropogenic climate change, it is a region of disproportionate vulnerability. This raises a fundamental asymmetric issue in the economic dimension of adaptation and mitigation [10].
Geographic dimension
By 2050, it is estimated that 70% of the world’s population will live in cities [40]. The health of populations is strongly influenced by their urban processes and wealth distribution mechanisms [48]. Cities with disordered growth and historical socio-spatial segregation mark processes of health inequity and undermine opportunities to improve well-being between generations. In the complexity of climate change, cities with deficient, obsolete or unmaintained basic services are a time bomb that can trigger disasters and, consequently, the distribution of diseases and mortality among vulnerable populations settled in cities [40]. This geographical determination of some segregated neighborhoods and coastal areas exposed to sea level rise, hurricanes or floods, generates the displacement of people. They are unlikely to return to their destroyed territories and livelihoods, and face a pilgrimage of violence, family breakdown and trauma [1].
The destruction of green spaces due to the growth of cities enhances the effects of climate disasters. Deforested territories and eroded soils increase the vulnerability of their inhabitants when matter that moves through space after flooding is not retained [49]. The peri-urban areas at greatest risk for their inhabitants are usually hillside settlements with poor basic service infrastructure and access to health centers, or those peripheries of tropical and subtropical regions that are exposed to sea level rise [50].
Health infrastructure dimension
Climate events destroy, disrupt and collapse the infrastructure and response capacity of hospitals and health services [11,49]. These are dynamics that can occur if the infrastructure of hospitals is previously deteriorated, their capacity to function depends on an obsolete basic services materiality or due to the inoperability of some governments [51]. With Hurricane Maria in Puerto Rico in September 2017, most hospitals abruptly collapsed due to a lack of electricity and water. People with pre-existing diseases, especially diabetics, patients who needed dialysis or asthmatics who depended on nebulizations, could not be attended. After Maria, up to December of that year, the mortality rate increased by 62% over the previous year. An additional 4645 people died [15] and thousands of families were left without their homes and property, in darkness for almost a year and with limited access to drinking water and food [52].
On the other hand, there is still insufficient training of health professionals in climate change issues. In addition, there is weak intersectoral planning to face climate crises, and the lack of information systems for monitoring and immediate actions (the aftermath of disasters). This is not a minor situation, since this absence is the main barrier to the design and implementation of public policies related to climate change and health, as well as the creation of systems that are resilient to their crises [17,53] (Figure 2).
Dimensions of climate change and health vulnerability.
Multiple intersectionality of health vulnerabilities
We propose to address the perspective of multiple intersectionality of vulnerabilities in the context of climate change, in order to understand how various dimensions converge during climatic events, increasing the risk of morbidity and mortality in populations historically conditioned by their economic situation, ethnicity, gender or migratory status. Hurricane Katrina, which occurred in 2005, is a documented case of multiple intersectionality. Its category five intensity was related to the rise in sea level and temperature [15,54]. A total of 400 000 people were permanently displaced [55]. Among these, 60% were women of African descent heads of households with children under 18 years of age, who did not return to New Orleans due to the loss of employment and the costs involved in rebuilding their homes [55,56].
Among the 105 000 inhabitants who did not own a car to evacuate before Katrina hit, two-thirds were African-American. Eighty percent of the neighborhoods most affected by levee breaches and flooding were those of residents of African descent [54]. Forty percent of other ethnicities, such as Vietnamese-Americans, lost access to health services and medication even a year after the hurricane, aggravating their health situation or leading to deaths [41]. More category five hurricanes occurred after Katrina, such as Hurricane Maria in Puerto Rico in 2017 or Hurricane Dorian in 2019. In the latter, for example, the Haitian migrant community lost 70% of their homes in Abaco Islands, northeastern Bahamas [57].
In Guatemala, it has become evident that the indigenous Mayan communities of Alta Verapaz are exposed to increasing health risks due to intense rainfall, floods and increasingly frequent landslides. However, they are considered marginalized by the State and receive minimal response to emergencies. Proof of this is that 311,000 people were forced to evacuate during the last tropical storms in 2020 [58].
The coastal communities of the Dominican Republic, composed mainly of Afro-descendant and mestizo populations, have faced in recent years an increase in hurricanes, storms and floods, as well as rising sea levels. All of these effects have had social impacts, such as food insecurity and increased risk of infectious diseases. The community of Cristo Rey is a territory of overcrowding, unemployment and fragile housing, a situation that worsens with the occurrence of extreme weather events. Despite this, it has a limited response from the State even with the National Climate Change Policy that has not been integrated into health planning and budgets [59].
During the heat waves recorded in Rio de Janeiro, Brazil, in November 2023 [60], an excess mortality of 1 392 people was estimated, comparable to the mortality rate in 2020 and 2021 during the COVID-19 pandemic. This climatic event, rated as extreme in the month of november when compared to temperature records from 2012 to 2023, especially affected older adults and women with a significant number of deaths within dwellings [60]. The flooding of Rio Grande do Sul in 2024 affected 48 674 agricultural producers and 21 000 dependent workers. The education of girls and boys was suspended due to the destruction of 1064 schools [61]. This event, attributed to anthropogenic climate change, displaced 581,638 people, including Venezuelan and Haitian migrants, and aggravated impacts on indigenous and Afro-descendant communities, as well as poor populations settled in at-risk areas, were considered [62].
Public policy perspectives on health and climate change
The connection between climate change and health has gained relevance in international diplomacy. During the XXVIII Conference of the Parties to the United Nations Framework Convention on Climate Change (COP 28) in December 2023, the Health Day and the Climate and Health Declaration were held for the first time. This declaration was adhered to by 140 countries that recognized the importance of the interactions between climate change and health, as well as the urgency of adopting resilience measures [63]. The challenges posed by the COVID-19 pandemic for the health sector were a wake-up call for health planning and management in the face of climate crises [56,64]. One of the lessons that requires attention is the exponential cost of delays by local governments and health systems in dealing with precipitous crises, such as environmental disasters. According to a meta-analysis of 16 integrated modeling studies, a 10-year delay increases the cost of mitigation and health actions by 37-50% [6,64].
The appropriate approach should be comprehensive, considering complex and articulated health systems, intersectoral and with a territorial approach. Likewise, gender perspectives and community participation, their knowledge and survival priorities are also necessary [17,41,42,56,65]. Beyond a focus on biological adaptation and natural selection in the face of climate change, transformative responses are needed that allow for full human prosperity, not a diminished survival.
Information systems on health and climate change must be strengthened. The information should be visible and analyzed by socioeconomic variables, gender, typology of territories and age groups [45,66]. It is also necessary to ensure its georeferencing. In addition, populations with pre-existing diseases that could be aggravated during and after climate disasters should be identified [17]. Indicators should be comparable at the regional level, since national health and climate change agendas are part of the international debate and participation [64].
Finally, training of health professionals in climate change is necessary [67]. In 2021, the World Health Organization reported in the Global Health and Climate Change Survey that approximately 50% of countries have insufficient professional competencies for the design and implementation of resilient health policies and systems. This is the main barrier to the implementation of health and environment planning [68]. Figure 3 provides an orientation towards resilient health systems.
Health systems resilient to climate shocks.

Discussion
The impacts of climate change on physical and mental health are widely evidenced [1,6,12,17,24,49]. The unique contribution of this review is to go beyond purely biological approaches and delve into broader dimensions that allow us to approach the causal chain and the socioeconomic conditions that shape these impacts. These intensify pre-existing health vulnerabilities or create new ones. In the face of extreme climate change events, these structuring dimensions of a social, economic, geographic and health nature generate asymmetrical trajectories of disease risk according to gender, ethnicity, age, migratory situation or social status of populations affected by historical processes of inequity and racial segregation. These dimensions are developed within the framework of a production and consumption model dependent on fossil fuels and extractivism.
From a social dimension, it highlights the need for a gender perspective in addressing climate change and health. This work shows the impacts of extreme temperatures on maternal health and perinatal outcomes [30,31,32,69,70], a higher risk of morbidity and mortality in adult women exposed to heat stress [35], and the increased vulnerability of women and girls who depend on agricultural activities and have been exposed to extreme climate phenomena. These facts are a warning that points to specialized health care for women and girls during and after climatic crises, the implementation of a system of safe shelters with psychological and obstetric first aid, the prevention of gender-based violence, and dignified access to feminine hygiene. Subsequently, local governments could design and implement economic reintegration programs for women heads of household who, due to these disasters, lost their source of livelihood.
During and after these climactic collapses, full access to welfare opportunities for minority ethnic groups is drastically limited. Some of them are forced to move and the living conditions of migrants deteriorate [6,7,39], many of them without full access to health services. This issue means a risk in the multiple intersections of a migrant person with a pre-existing disease [49]. Such a situation should remove the health practice, framing it as a vital and universal human right for all social groups that suffer in a differentiated way and with greater intensity in climate emergencies.
Climate change, linked to the economic dimension, exposes poor populations to the loss of their fragile means of livelihood and housing, due to the destruction of territories and crops [24]. It also confronts them with a lack of energy, deprivation of clean water, difficulties in access to health services and food [1,41,42,49]. The future implications of these facts border on the problems of inequity, together with physical and mental health, which result in the need for intersectoral work and renewal of health systems for the care of victims of climate crises. The geographic dimension and its urban dynamics point to the growth of cities and climate threats intensified in the 21st century. Coastal cities, islands and populations settled near oceans and rivers directly face rising sea levels and floods resulting from prolonged rainfall [15,54].
Related to this geographic and urban dimension is the health dimension and its infrastructure. It is linked to the training of professionals to ensure effective and timely health services, with special attention to people with pre-existing diseases whose lives depend on permanent treatment, drugs and recurrent use of hospital equipment [15,55]. These facts imply an interrelated work between the health sector, risk management in cities and urban planning, as well as the consequent design of health systems resilient to climate crises.
The implications of aggravated vulnerability after climate events require public health systems that contemplate resilient and multilevel planning, interdisciplinary, national and local work, integrated with other ministries. Rapid and timely decentralized actions should flow with community participation and monitoring and disaggregated information on social, geographic and gender variables. The integration of the biological into the economic and social [71], is the missing link in the debates on climate change and in the processes of health and disease.
Future lines of research could demand comparative analyses between regions and the contrast of public policies on health and climate change, in order to evaluate their effectiveness and scope. It is necessary to evaluate the resilience of existing health systems in the context of climate hazards and the capacities for intersectoral work. Another line of research merits the analysis of morbidity and mortality after extreme climate disasters. These lines of work should address the problem of aggravation of disease and death due to lack of treatment and medical supplies that are interrupted by the collapse of health services, together with the political and financial inability to resume them. This is especially relevant in low-income countries.
Conclusions
The integration of findings in this review allowed for an in-depth understanding of different dimensions of health vulnerability in the context of anthropogenic-influenced climate change. The results allowed a deeper understanding of the social, economic, geographic and health dimensions that, crossed by the current climate crisis, reproduce differentiated trajectories of physical and mental illness risks. All of them can be aggravated in the multiple intersectionality of gender, ethnicity, migration, age and social class. This is especially true in territories of inequity, historical marginalization and excessive extractivism of natural resources.
This review reinforces the need for greater involvement and budget of the health sector in climate action. Public health policy must urgently consider national systems that are resilient to climate crises, beyond the merely adaptive approach to human survival. To this end, it is proposed to address the dimensions described here and information systems with data disaggregated by socioeconomic, geographic and health variables. Health actions should be multilevel, intersectoral in scope, with a focus on gender, participation and integration of community knowledge.

