Artículo de revisión
← vista completaPublicado el 20 de noviembre de 2025 | http://doi.org/10.5867/medwave.2025.10.3120
Inteligencia artificial para la clasificación y el diagnóstico de lesiones cutáneas en dermatología: una revisión narrativa
Artificial intelligence for skin lesion classification and diagnosis in dermatology: A narrative review
Abstract
Introduction Artificial intelligence (AI) is increasingly present in dermatology, demonstrating accuracy levels comparable to, or even superior to, those of dermatologists in diagnosing skin lesions from clinical and dermoscopic images. This review provides an overview of AI’s role in the automated classification and monitoring of skin lesions.
Objective To explore and map the existing literature on the use and benefits of AI in dermatology.
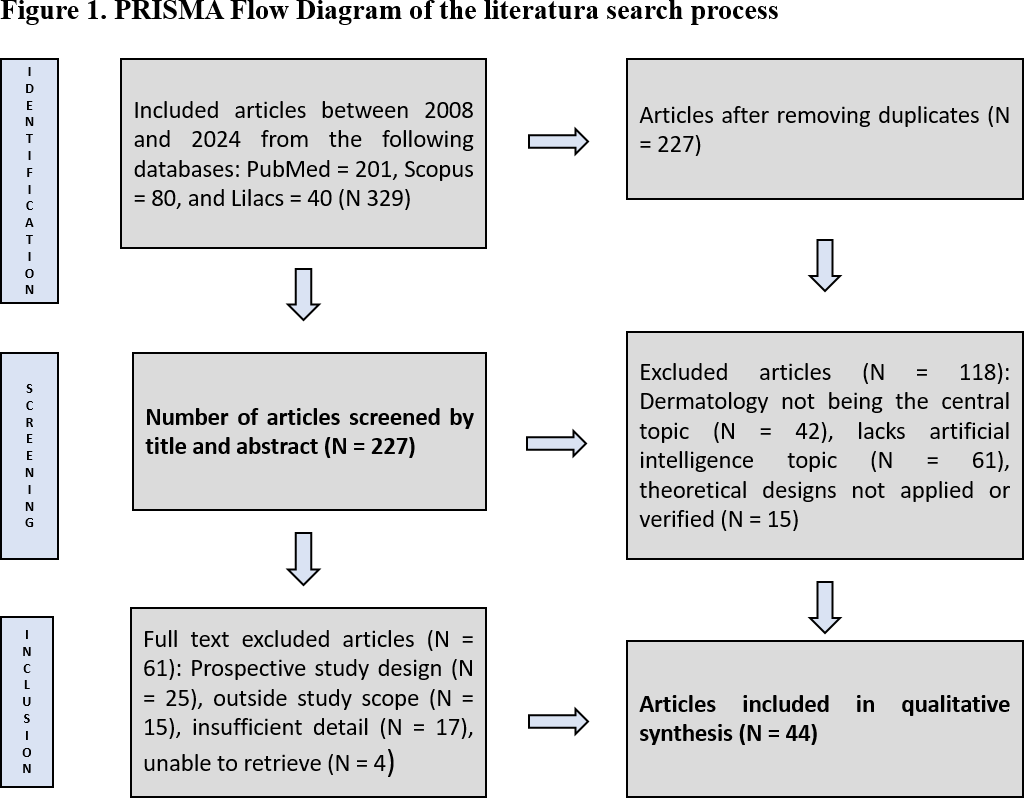
Methods This narrative review focused on exploring the use and benefits of AI in dermatology, utilizing MeSH/DeCS terms such as "Dermatology," "Artificial Intelligence," "Diagnosis," and "Computer Aided Diagnosis." Three databases (PubMed, Lillacs, and Scopus) from 2008 to 2024. We excluded articles that did not focus on dermatology, lacked the topic of Artificial Intelligence, or presented theoretical designs without practical application or evidence, resulting in a final selection of forty-four articles.
Results The results strongly support AI’s effectiveness, displaying its precision in diagnosis, comparable to or exceeding that of human dermatologists across diverse tasks. The evolution of AI in dermatology implies a substantial transformation in care, extending its applications from skin cancer to various dermatological pathologies. While emphasizing the vital collaboration between AI and healthcare professionals, a critical gap remains in the real-world clinical validation of AI. Ethical considerations, especially in automated decision-making, need careful attention.
Conclusions This narrative review highlights the crucial role of AI in dermatology, emphasizing its potential to enhance diagnostic accuracy for skin lesions.
Main messages
- Artificial intelligence (AI) is revolutionizing dermatology by offering accurate diagnoses of skin lesions, comparable to or superior to those of dermatologists.
- This review highlights the growing applicability of AI beyond skin cancer, including multiple dermatological pathologies.
- There is a significant limitation in clinical validation in real-life settings, which restricts its widespread implementation.
- The main finding shows that AI improves diagnostic accuracy and could optimize dermatological care in the future.
- Greater attention is needed to the ethical implications of automated decision-making in healthcare.
Introduction
Artificial intelligence (AI) is transforming dermatology, achieving accuracy comparable to or exceeding dermatologists in diagnosing skin lesions from clinical and dermoscopic images. Despite these advances, a gap remains in real-world clinical validation. This narrative review explores AI applications in dermatological image analysis, assessing capabilities, challenges, failure modes, and performance evaluation metrics. AI has the potential to enhance access and quality of care, with studies showing it can match or surpass experts in diagnosing multiple skin conditions, highlighting its transformative potential [1,2,3,4].
Dermatology faces increasing complexity and a need for rapid, accurate decisions. AI has evolved to create multimodal models integrating medical records, lab reports, and dermoscopic images. While early research focused on skin cancer, especially melanoma, current efforts aim to improve diagnostic efficiency across various conditions and support therapeutic recommendations [5,6].
In parallel, the increasing burden of skin diseases in primary care has generated notable interest in the application of machine learning models as collaborative tools. Statistics reveal that dermatological consultations account for around 20% of total annual visits to primary care, with around 35% being referred to dermatology specialists [7]. Machine learning models, with their ability to analyze and optimize complex datasets [8] as shown in Table 1, are presented as an effective way to improve efficiency in the detection and classification of skin diseases in this environment. The convergence of these technological developments highlights the importance of a comprehensive vision ranging from primary to specialized care, integrating the application of artificial intelligence in dermatology with the growing need to optimize the management of skin pathologies [9].
Objetive
The objective of this review is to comprehensively explore and map the existing literature on the use and benefits of artificial intelligence (AI) in the field of dermatology. We aim to identify and synthesize the diverse research and approaches that have addressed the integration of AI in the diagnosis, treatment, and management of skin diseases. In this way, it provides an overview that serves as an essential reference for future research and development in the application of artificial intelligence in dermatology.
Methods
This review was conducted following the guidelines from the Preferred Reporting Items for Systematic Review and Meta-Analysis adapted from Arksey for narrative reviews (PRISMA-ScR) [10] and refined by Levac et al [11], a systematic review was conducted following these steps: 1) identifying the research question; 2) searching and identifying relevant studies; 3) selecting studies; 4) data analysis; 5) summarizing and reporting results. We adhered to the reporting guidelines for systematic reviews and meta-analyses tailored for narrative reviews (PRISMA-ScR) [12]. We searched three databases (PubMed, Lilacs and Scopus). To review the available evidence on the use and benefits of artificial intelligence in dermatology.
For the above, MeSH/DeCS terms such as "Dermatology", "Artificial Intelligence", "Diagnosis", and "Computer Aided Diagnosis" were used, in their translation into English, Portuguese, and Spanish, limiting the publication date from January 1st, 2008. It was filtered by articles that were reflective texts or research studies including topics such as the application of AI in dermatology and the comparison at the time of diagnosis between AI and dermatologists.
The eligibility criteria included publications with empirical and observational data that studied or discussed the use of artificial intelligence in dermatology, in English, Portuguese, and Spanish, between 2008 and 2024. We excluded articles with theoretical data, clinical management guidelines, protocols, and publications without access to abstracts and full documents. For data extraction, four independent authors reviewed and selected titles and abstracts of candidate publications. Regular meetings were held with all authors to resolve discrepancies and reach a consensus on the articles to be included in the review.Two additional independent researchers resolved further disagreements. Duplicates were removed, and the selected documents in full text were obtained through the University of La Sabana library. Following the final selection of documents, the following data were extracted from eligible studies: authors, document type, population characteristics, objective, year of publication, authors' country, main findings, and limitations, presented in Table 2.
Results
Of 329 articles that were found in databases, 102 duplicates were discarded. By title and abstract, 118 were discarded because dermatology was not the central topic, did not include the topic Artificial Intelligence, or featured theoretical designs without application or evidence. The remaining 109 were downloaded and stored in PDF format for complete review by the research group. Subsequently, 64 articles were discarded for not meeting the inclusion criteria after review, leaving a total of 44 articles, as shown in Figure 1. This figure summarizes the identification process, including the understanding of eligibility criteria based on originality, methodology, and relevance, as well as the inclusion of articles.
PRISMA Flow Diagram of the literature search process.
The selected studies included several types of articles, which allowed us to obtain a spectrum of various aspects that must be evaluated in the study of artificial intelligence in dermatology. Among these, the vast majority are experimental studies where tests on sensitivity and specificity are carried out. When making diagnoses of the machines in front of diverse types of people (general practitioners not trained in dermatology, in some cases, and other dermatologists with vast experience). The study type was primarily experimental, with 22 articles in total; followed by seven observational studies, five cross-sectional analyses, two systematic reviews & meta-analyses, two retrospective studies, two reviews and perspectives, two comparative studies, and two literature/narrative reviews.
Evaluating the performance of artificial intelligence in dermatology
In evaluating the performance of AI in dermatology, a critical aspect is comparing its effectiveness to that of human professionals' diagnostic capacity. Numerous studies consistently demonstrate that AI models exhibit a classification accuracy for skin lesions comparable to, and in some cases, superior to that of dermatologists. This marks a significant milestone in dermatological diagnosis, suggesting a transformative potential for enhancing efficiency in clinical decision-making. For instance, an experimental study conducted in 2020 assessed the diagnostic performance of a convolutional neural network in differentiating between combined naevi and melanomas, comparing dermatologists' results with those of the convolutional neural network. The results revealed notable outcomes: the convolutional neural network's sensitivity was 97.1%, its specificity was 78.8%, dermatologists' sensitivity was 90.6%, and dermatologists' specificity was 71.0%. Notably, a particular benefit was observed in 'beginners' when aided by convolutional neural network verification, with a diagnostic odds ratio of 98, indicating improved diagnostic performance. This highlights the potential of AI, particularly in assisting less experienced dermatologists in accurately differentiating lesions [16].
The remarkable advancements in AI’s diagnostic accuracy in dermatology are not confined to recent breakthroughs. The roots of this progress can be traced back to 2009, when Rajpara et al. conducted a study evaluating the diagnostic accuracy of dermoscopy and digital dermoscopy/artificial intelligence in melanoma diagnosis. In this study, various dermoscopic algorithms were compared with each other and with digital dermoscopy/artificial intelligence for melanoma detection. The findings revealed a pooled sensitivity for artificial intelligence that slightly surpassed that of dermoscopy performed by dermatologists (91% vs. 88%, p = 0.076). Although dermoscopy demonstrated significantly better pooled specificity compared to artificial intelligence (86% vs. 79%, p < 0.001), the pooled diagnostic odds ratio showed no significant difference (51.5 for dermoscopy and 57.8 for artificial intelligence, p = 0.783). This historical perspective highlights the continuous evolution and validation of AI in dermatological diagnostics over the years. In contrast to these advancements, novel investigations reveal a clear progression [55].
Implications for clinical decision making
The rapid advancement of technology has enabled the integration of multimodal data, including clinical information, laboratory reports, and visual data, into AI models in dermatology [49]. This opens the door to more complete and accurate decision-making, supported by comprehensive data evaluation. However, there arises a need to carefully address the ethical implications and responsibility in automated decision-making in the medical field. The study by Hekler et al. states that during the clinical examination, the doctor has additional data to make the diagnosis that goes beyond the simple visual examination of the area of skin explored, such as the data obtained in interrogation [19]. Therefore, the study by Birkner et al. concludes that comparing artificial intelligence and visual diagnoses from human experts may be perceived as unequal, given that, in clinical practice, skin specialists tend to consider non-visual information when formulating a diagnosis [27].
Current applications and challenges in dermatopathology
As artificial intelligence advances, its application in dermatopathology has expanded beyond the initial focus on skin cancer, encompassing a range of dermatological pathologies. It is imperative to emphasize that AI aims to complement, not replace, the expertise and clinical judgment of dermatologists. Collaboration between AI and healthcare professionals is pivotal for the effective development of deep learning algorithms in dermatopathology. In 2017 study, the top-ranked computer algorithm demonstrated an area under the receiver operating characteristic curve of 0.87, surpassing dermatologists (0.74) and residents (0.66) significantly (p < 0.001 for all comparisons) but demonstrated that integrating computer algorithm classifications into dermatologist evaluations elevated dermatologist sensitivity and specificity from 76.0% to 80.8% and specificity from 72.6% to 72.8% as shown in Figure 2. The mounting evidence suggests that deep neural networks hold the potential to accurately classify skin images of melanoma and its benign mimickers, offering a promising avenue to enhance human performance [56].
Human-machine collaboration effect.
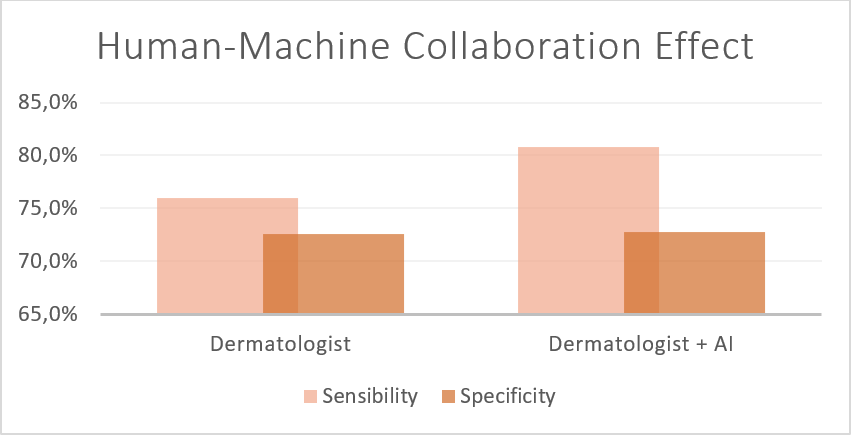
Source: Prepared by the authors based on the results of the study.
Artificial intelIigence´s performance in primary care
Using AI in primary care can accelerate the diagnosis process, contribute to earlier and more effective care, and reduce the care burden and improve the quality of dermatological care in primary care. In a study conducted by Jain et al. in 2021, which involved primary care physicians without dermatology experience and nurse practitioners, it was found that AI assistance was significantly compared to higher performance at diagnosis, in the case of physicians, the increase in diagnostic agreement was 10% (95% CI, 8% to 11%; p < 0.001), from 48% to 58%; for nurses, the increase was 12% (95% CI, 10% to 14%; p < 0.001), from 46% to 58%. In this way, the desire rates for biopsies and referrals to a dermatologist are expected to decrease with the use of AI [48].
Similarly, in the study conducted by Samaran et al. in 2021 in France, which surveyed 147 general practitioners, 98% said they had difficulty diagnosing non-pigmented skin tumors, and 86% agreed that an AI diagnostic tool could be useful in a general practice setting; however, 68% would not be willing to pay for this type of software [45]. Finally, a study conducted by Han et al. in 2022, which evaluated the use of AI in medical students and dermatology residents, showed that the accuracy of the AI-assisted group was significantly higher than that of the unassisted group, particularly benefiting non-dermatology students [54].
Areas for improvement
It is crucial to acknowledge the current limitations of AI in dermatology as identified within the reviewed articles. A considerable number of studies highlight a major limitation – the lack of research on real-world applications [14,17,26,31,32,46,47,53]. Additionally, there is a call for broader studies, as the evaluated algorithms show potential in small groups [3,49]. Similarly, several articles mention that the performance of studies was assessed on specific datasets, which could limit the generalizability of the findings. Therefore, there is a need to expand the characteristics of datasets and clinical scenarios [25].
Another noteworthy limitation is the variability in dermatologists' performance, which is based on their experience and familiarity with technology in assisting convolutional neural networks [24]. Furthermore, practical algorithm training requires high-quality photos for result interpretation [13]. Lastly, ethical concerns, particularly in clinical decision-making, must be taken into consideration [34]. Identifying these limitations guides future research towards areas focused on enhancing AI models.
Discussion
The narrative review highlights the critical role that artificial intelligence (AI) plays in improving diagnostic capacities while illuminating the changing landscape of AI applications in dermatology. The results provide a strong body of data in favor of AI’s ability to diagnose skin lesions as accurately as human dermatologists, if not surpassing them. Noteworthy meta-analyses and studies consistently highlight AI’s effectiveness in various diagnostic tasks, marking a transformative milestone in dermatological care. The exploration of AI’s applications extends beyond its initial focus on skin cancer, encompassing diverse dermatological pathologies. The study underscores the collaborative nature of AI integration, emphasizing its role as a complementary tool to enhance rather than replace the clinical judgment of dermatologists.
The narrative review highlights the critical role that artificial intelligence (AI) plays in enhancing diagnostic capabilities while shedding light on the evolving landscape of AI applications in dermatology. The results provide a substantial body of data in favor of AI’s ability to diagnose skin lesions as accurately as human dermatologists, if not surpassing them. Noteworthy meta-analyses and studies consistently highlight the effectiveness of AI in various diagnostic tasks, marking a transformative milestone in dermatological care. The exploration of AI’s applications extends beyond its initial focus on skin cancer, encompassing a diverse range of dermatological pathologies. The study highlights the collaborative nature of AI integration, emphasizing its role as a complementary tool to enhance, rather than replace, the clinical judgment of dermatologists.
The evaluation of AI’s performance in dermatology demonstrates its effectiveness in lesion classification, with several studies showing accuracy comparable to, and in some cases superior to, that of human dermatologists. The narrative review delves into historical perspectives, highlighting the continuous evolution and validation of AI in dermatological diagnostics since 2009. The comparison of diagnostic accuracy between AI and dermoscopy, as performed by dermatologists, reveals a nuanced landscape, with AI showing slightly higher sensitivity but, in some cases, lower specificity. The discussion acknowledges the ethical implications of automated decision-making, emphasizing the importance of considering additional non-visual information during clinical examinations. The integration of multimodal data into AI models presents opportunities for more comprehensive decision-making, but ethical considerations and responsibilities must be carefully addressed.
Faced with the notable advances in the implementation of artificial intelligence in the medical field, various tools have been developed to ensure transparency and reproducibility in research that evaluates its application. A notable example is the APPRAISE-AI tool, which is responsible for evaluating methodological quality to support clinical decisions. This tool, composed of 24 items, analyzes in detail the methods, results, and transparency of the studies, providing researchers with the ability to generate higher-quality evidence to support their research in the field of artificial intelligence in medicine [57]. The use of this tool is recommended, given its usefulness in strengthening the methodological foundation and enhancing transparency in studies related to artificial intelligence in dermatology.
Furthermore, the narrative review addresses the current applications and challenges in dermatopathology, emphasizing the role of AI in complementing dermatologists' expertise. The collaboration between AI and healthcare professionals is highlighted as pivotal for the effective development of algorithms. Notable advancements in diagnostic accuracy, as evidenced by a 2017 study, underscore the potential of AI to classify skin images and enhance human performance accurately. The main topic encompasses the implications of AI in primary care, highlighting its potential to accelerate diagnosis, improve care quality, and alleviate the burden on healthcare providers. Insights from studies involving primary care physicians and medical students underscore the positive impact of AI assistance in diagnosis. Overall, the narrative review provides a comprehensive overview of AI’s current standing in dermatology, acknowledging its transformative potential while recognizing the need for ethical considerations and ongoing collaboration between AI and healthcare professionals.
The World Health Organization’s recent guidance on AI in healthcare, developed collaboratively by the Health Ethics and Governance unit and the Department of Digital Health and Innovation, provides key ethical principles for the use of AI in health. These principles include protecting human autonomy, promoting human well-being and safety, ensuring transparency, explainability, and intelligibility, fostering responsibility and accountability, ensuring inclusiveness and equity, and promoting AI that is responsive and sustainable. The guidance underscores the importance of avoiding harm, maintaining transparency in AI technologies, and holding stakeholders accountable for the responsible development and deployment of AI in healthcare. The document emphasizes the ethical use of AI to benefit public health and addresses challenges related to privacy, autonomy, and the need for valid informed consent. Additionally, it highlights the importance of inclusiveness and equity in AI applications, emphasizing the need to avoid biases that could disproportionately affect marginalized groups. As the use of AI in healthcare continues to evolve, these principles aim to guide governments, technology developers, companies, and other stakeholders in adopting ethical approaches for the responsible integration of AI in health systems worldwide [58].
The comprehensive responsibility for making a diagnosis falls on the health professional, establishing a fundamental bond that covers professional, ethical, and legal aspects with the patient. This approach differs significantly from the contribution of artificial intelligence (AI), which offers a valuable diagnostic approach but does not replace the significant role of the medical professional. In the dermatological context, the gold standard continues to be the biopsy, since, for example, although the lesions may be highly suggestive of carcinoma or melanoma, it is the biopsy that definitively determines the malignant or benign nature of the lesion.
The comprehensive responsibility for making a diagnosis rests with the health professional, establishing a fundamental bond that encompasses professional, ethical, and legal aspects with the patient. This approach differs significantly from the contribution of artificial intelligence (AI), which offers a valuable diagnostic approach but does not replace the significant role of the medical professional. In the dermatological context, the gold standard remains the biopsy, as it is the definitive determination of the malignant or benign nature of the lesion, even when lesions are highly suggestive of carcinoma or melanoma.
In scenarios where dermatological care is not readily available, AI emerges as a promising tool for providing early guidance to care teams. This AI capability is crucial for patient prioritization, thereby mitigating costs associated with complications and delayed care. Although artificial intelligence can facilitate an initial approach, we emphasize that confirmation and exhaustive evaluation through biopsy remain the undisputed standard in dermatology.
Limitations
The limitation of this narrative review lies in the variability and lack of standardization among the included studies. Despite the growing interest in the application of artificial intelligence in dermatology over the past few years, a notable dearth of standardized methodologies and consensus remains in the field. The studies encompassed a range of AI models; each was developed independently with distinct characteristics and methods. This lack of uniformity poses challenges in assessing the reproducibility and generalizability of findings across different studies. The absence of standardized rules or a consensus framework introduces potential bias, as the quality and performance of AI models can vary significantly. This limitation highlights the need for future research efforts to establish standardized guidelines and a consensus on the application of artificial intelligence in dermatology, thereby ensuring a more robust and reliable foundation for the field.
Conclusions
In conclusion, the narrative review underscores the pivotal role of artificial intelligence (AI) in dermatology, emphasizing its ability to enhance diagnostic capabilities for skin lesions. The findings robustly support the effectiveness of AI, demonstrating its precision in diagnosis, comparable to or surpassing that of human dermatologists across various tasks. As AI evolves, a notable transformation in dermatological care is evident, with applications extending beyond skin cancer to diverse dermatological pathologies. While emphasizing the essential collaboration between AI and healthcare professionals, there is a recognition of the need to carefully address ethical implications, particularly in automated decision-making.
In conclusion, this narrative review highlights the fundamental role of artificial intelligence (AI) in dermatology, emphasizing its potential to enhance the diagnosis of skin lesions. The results strongly support the effectiveness of AI, demonstrating its diagnostic accuracy, which is comparable to or superior to that of human dermatologists in various tasks. As AI evolves, a remarkable transformation in dermatological care is becoming apparent, with applications extending beyond skin cancer to encompass various pathologies. While the essential collaboration between AI and healthcare professionals is highlighted, the need to carefully address the ethical implications of automated decision-making is recognized.
Overall, this review provides an overview of the current state of AI in dermatology, highlighting its transformative potential and underscoring the importance of ethical and collaborative integration in the future development of these technologies in the medical field.

