Artículo de revisión
← vista completaPublicado el 28 de abril de 2020 | http://doi.org/10.5867/medwave.2020.03.7891
¿Conocemos las propiedades diagnósticas de las pruebas usadas en COVID-19? Una revisión rápida de la literatura recientemente publicada
Do we know the diagnostic properties of the tests used in COVID-19? A rapid review of recently published literature
Abstract
COVID-19 has brought death and disease to large parts of the world. Governments must deploy strategies to screen the population and subsequently isolate the suspect cases. Diagnostic testing is critical for epidemiological surveillance, but the accuracy (sensitivity and specificity) and clinical utility (impact on health outcomes) of the current diagnostic methods used for SARS-CoV-2 detection are not known. I ran a quick search in PubMed/MEDLINE to find studies on laboratory diagnostic tests and rapid viral diagnosis. After running the search strategies, I found 47 eligible articles that I discuss in this review, commenting on test characteristics and limitations. I did not find any papers that report on the clinical utility of the tests currently used for COVID-19 detection, meaning that we are fighting a battle without proper knowledge of the proportion of false negatives that current testing is resulting in. This shortcoming should not be overlooked as it might hamper national efforts to contain the pandemic through testing community-based suspect cases.
Introduction
At the end of 2019, the world was made aware of a lethal new strain of coronavirus—later to be called SARS-CoV-2—that was causing death and disease in large segments of the Chinese population, mainly in the city of Wuhan. By March 11, 2020, the World Health Organization was declaring that the disease caused by this novel virus, COVID-19, was a pandemic. At the time this article is being written, nearly three million cases of COVID-19 and over 200 000 deaths have been reported worldwide. A systematic review found that for 656 patients, the main manifestations of COVID-19 include fever, cough, and dyspnea, and 32.8% present acute respiratory distress syndrome, 20.3% of cases require intensive care unit, and 6.2% will develop shock[1].
This enormous burden on our hospital systems has led to aggressive strategies aimed at mitigating or suppressing the spread of the virus in the general population, the intensity of which has been strikingly disparate among the affected countries[2],[3]. Regardless of the strategies deployed by national and local governments, the more successful ones rely on laboratory testing and subsequent isolation of suspect cases. According to the World Health Organization, laboratory “testing for COVID-19 is critical to tracking the virus, understanding epidemiology, informing case management, and to suppressing transmission” (see Technical Guidance). However, information on which tests the different countries are using to detect cases and conduct epidemiological surveillance is not readily available. Even less information is available on the properties of the diagnostic tests currently deployed in the field, and press reports have referred to the problem of false-negative results[4].
We are still in the process of understanding SARS-CoV-2. Long incubation time may be responsible for the rapid dissemination and infectivity of this strain of coronavirus[5]. However, this was rebutted by a recent analysis on a larger dataset of patients that found no statistically significant differences in the mean incubation time for SARS-CoV, MERS-CoV, and SARS-CoV-2[6]. Also, many asymptomatic individuals have tested positive for SARS-CoV-2[7]. Statistical modeling on the Diamond Princess cruise ship found that 17.9% (95% confidence interval: 15.2% to 20.2%) of individuals who tested positive for SARS-CoV-2 were asymptomatic, but this could be an underestimation given that not all passengers were tested[8]. Conversely, a high false-negative rate of nucleic acid test for SARS-CoV-2 has been reported for the most used diagnostic tool for COVID-19 screening—the reverse-transcription polymerase chain reaction (RT-PCR) assay using oropharyngeal swab samples[9],[10],[11],[12]. In a letter to the editor, an author describes a case of three consecutive samples negative for the SARS-CoV-2 nucleic acid, which was finally confirmed as COVID-19 pneumonia based on the chest computed tomography scan showing the typical ground-glass opacification and a fourth RT-PCR test with a positive result[13]. Thus, many reports are now advising that the diagnosis of COVID-19 should include computed tomography images together with PCR testing in highly suspect cases[14],[15].
Sampling methods to detect viral nucleic acid in the upper airway have also been called into question due to the purported high rate of false negatives[7],[9]. A literature review published in Chinese based on the prior experiences of severe acute respiratory syndrome coronavirus, middle east respiratory syndrome coronavirus, and influenza A, pointed to the lack of uniform recommendations on the method to collect the upper respiratory tract specimen and found that the nasopharyngeal aspirate had a higher positive rate within two weeks of symptom onset, while combined nasal and oropharyngeal swabs were the least harmful to medical staff during sampling[16]. Some suggest that samples for testing viral infection should be taken from the lower respiratory tract of the patients, including sputum and bronchoalveolar lavage fluid[9],[17].
Laboratory methods to detect the presence of SARS-CoV-2 in a biological sample have advantages and disadvantages. Isolation of the virus can be achieved from cell cultures; rapid antigen tests, serology, and molecular assays are all either actively deployed in epidemiological surveillance or are being currently tested for point-of-care use[17],[18]. Considering the need to have reliable data on the test properties of the different methods that are being introduced to control the COVID-19 pandemic, I decided to undertake a literature review to know the accuracy and clinical utility of the current screening methods used for SARS-CoV-2 detection in suspect cases.
Methods
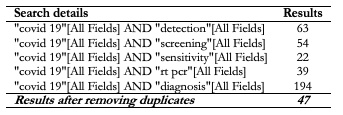
I searched in PubMed/MEDLINE with keywords “covid 19”, “sensitivity”, “screening”, and “detection” (see Table) up to March 26, 2020. I used the following MeSH terms to build the searches: “covid 19”, “detection”, “screening”, “sensitivity”, “rt pcr”, and “diagnosis”. I then searched the references of the selected articles to find primary references to diagnostic test properties.
The inclusion criteria were articles reporting on laboratory diagnostic tests and rapid viral diagnosis.
The exclusion criteria were case reports, opinion pieces, letters to the editor, articles reporting clinical findings, surveillance strategies, imaging techniques, epidemiology, mitigation strategies, articles addressing population subgroups (e.g., pediatrics, pregnant women) or non-diagnostic outcomes (e.g., mental health), treatment strategies, and guidelines. Articles in Chinese were also excluded if a reasonable translation was not possible to obtain. For this rapid review, I also excluded preprints because of their preliminary nature and lack of peer validation.
Results
After running the search strategies and screening the titles, 47 articles were found eligible for abstract screening (Table 1). After assessing the eligible articles for inclusion and exclusion criteria, I selected 13 papers for full-text review. All these papers were published in the first quarter of 2020, and only eight complied with the inclusion and exclusion criteria[15],[19],[20],[21],[22],[23],[24],[25]. All 47 articles were used for the preparation of this review, plus further references that were found during the writing of the review. The main search was done on March 26.
 Full size
Full size Analysis of the findings
The purpose of this review is to know the sensitivity and specificity of the tests that are currently in use for the detection of SARS-CoV-2 throughout the world. These tests are in vitro diagnostics that analyze samples taken from the human body (some examples are serum, sputum, saliva, blood, urine, and feces). Decisions are made based on the results. Thus, front-line healthcare professionals should know what the probabilities are for false negatives and false positives, in other words, the accuracy of the test. A test will give us a correct result to the extent that it is positive in the presence of disease (true positive) and negative in the absence of disease (true negative); both false positives and false negatives will provide misleading information[26]. Screening tests, which are used in the asymptomatic populations, should be easy to administer, quick to deliver results, low-cost, and, most importantly, highly sensitive. Currently, the gold standard for the detection of the SARS-CoV-2 is RT-PCR because when the sample picks up a virus or viral fragment, even in minimal quantities, it should provide a 100% sensitivity. However, due to a variety of shortcomings that I comment further on, our current forms of testing for the novel coronavirus may be falling short.
Virus nucleic acid RT-PCR tests
Various forms of RT-PCR testing are the predominant diagnostic method for COVID-19. While it can detect the presence or absence of viral nucleic acid and thus directly confirm viral infection in a human sample, it is prone to several limitations. These tests can only be processed in certified laboratories, which means that in most countries, test results are coming out with detrimental delays to patients, and healthcare and surveillance systems. Furthermore, there are preanalytical and analytical factors that can compromise the quality of RT-PCR testing for detecting SARS-CoV-2, thus reducing the diagnostic accuracy of the test[27].
Chan et al. in Hong Kong report the development of a new assay that targets a different region of the SARS-CoV-2 genome (RdRp/Hel, S, and N genes) using both in vitro and clinical specimens[22]. Two hundred seventy-three specimens were collected from 15 Hong Kongese patients (8 males, 7 females; age range 37 to 75 years) with laboratory-confirmed COVID-19. The authors report that the assay was highly sensitive and specific for the detection of SARS-CoV-2 RNA in vitro but it was not tested in non-COVID-19 patients. The clinical utility of this new test is not known.
Korean authors developed an easy specimen collection via a self-collected pharyngeal swab to perform an RT-PCR and Trizol-based RNA purification that they tested in 12 mostly asymptomatic human volunteers[24]. The authors provide detailed instructions on how to collect the throat swab. The positive control with SARS-CoV-2 viral RNAs was extracted from Vero cells infected with a viral clone. The purpose of this study was to create a highly sensitive detection protocol to identify true negatives for SARS-CoV-2, but the limited scope of the validation hampers any possibility of generalizability for this study.
Liu et al. conducted a retrospective analysis of RT-PCR based viral nucleic acid test from 4880 suspect cases for COVID-19 occurring from late January to mid-February in the Renmin Hospital of Wuhan University[20] based on nasal and pharyngeal swabs, and bronchoalveolar lavage fluid and sputum. The study’s main result was a 38% positive finding for SARS-CoV-2 for that population, which increased to 57% in the population from the fever clinics. This study only allows us to determine, for this population, the proportion of positive tests in a population with a high likelihood of having COVID-19 based on the presence of respiratory infection symptoms or close contact with COVID-19 patients. There was no follow-up on cases to determine whether all positive tests were COVID-19 patients, nor whether the negative tests were truly disease-free. In other words, this study does not provide the necessary data to calculate sensitivity and specificity for the test in this disease-prevalent population.
Another group in Korea developed and evaluated Loop-Mediated Isothermal Amplification (LAMP) assays to detect genomic RNA of SARS-CoV-2 and found that RT-LAMP assays can detect as low as 100 copies of SARS-CoV-2 RNA, thus providing very high technical accuracy[28]. However, the clinical applicability of this technique has not yet been studied for SARS-CoV-2.
Immunoassays
Immunoassays test specific antibodies in patient blood. Li et al. developed a point-of-care lateral flow immunoassay test that can detect IgM and IgG in human blood in 15 minutes[25]. Interestingly, the test was applied in eight Chinese sites from six provinces, in both infected and non-infected patients, totaling 522 cases, of which 397 were previously COVID-19 confirmed with PCR test, and 128 were non-infected patients. Three hundred fifty-two tested positive, resulting in a sensitivity of 88.66%. The specificity was 90.63% (12 false positives). The spectrum of patients is not reported, and neither is the independence of testing with the gold standard.
Another study sought to describe the time kinetics of the anti-SARS-CoV-2 IgA, IgM, and IgG antibodies using an ELISA based assay on 208 plasma samples collected from two cohorts of patients: 82 confirmed and 58 probable cases from Wuhan and Beijing hospitals[19]. The median duration of IgM and IgA detection was five days (range, 3 to 6), while IgG was detected 14 days after symptom onset (range, 10 to 18), with a positive rate of 85.4%, 92.7%, and 77.9%, respectively. This study helps to understand the humoral responses to the virus and thus to situate the immunoassay’s capability to detect any response in a COVID-19 patient.
Limitations of diagnostic test studies
The included studies were all carried out during the COVID-19 epidemic, later defined as a pandemic. It is not the same when these tests are done for screening purposes (in asymptomatic population) rather than for diagnostic purposes (to confirm or rule out when there is a high pretest probability of disease). Establishing the sensitivity or specificity of a test is not necessarily independent of prevalence, insofar as the methods by which sampling is done (e.g., sputum or nasopharyngeal swabs) may determine the greater or lesser likelihood of picking up the virus, which will differ if the population that is being sampled has more or less advanced disease[26].
Many reports refer to the analytical evaluations of tests to detect SARS-CoV-2 and workflows[23],[29],[30],[31], but these are not useful for the clinical and epidemiological decision-making process and do not report results in the field with real patients. Most of the published papers on COVID-19 and diagnosis are not studies conducted in community-based suspect cases, which could provide pragmatic results on sensitivity and specificity.
Conclusion and final remarks
Front-line professionals battling the SARS-CoV-2 pandemic should be aware of the risk of misclassification given the consequences of missing the disease in infected people. When we know that a screening test is highly sensitive, then we could confidently rule out the disease if the test is negative. Do we need to further work up a positive test result in an asymptomatic person to confirm that it is a true positive? Probably not, as the central management indication will be to maintain quarantine if other elements in the history give us a high pre-test probability for the patient having contracted COVID-19, such as having traveled to a high-risk country, having had contact with a known SARS-CoV-2 positive person, or having attended a crowded and enclosed gathering in the previous days or weeks. Nonetheless, China has reported that computed tomography scans are more sensitive for COVID-19 than the RT-PCR tests and, until recently, it was used as standard practice in diagnosing the disease[32]. While several papers describe the molecular diagnostics for this novel virus[9],[33],[34], my review did not find any that report on the clinical utility of the tests currently used for COVID-19 screening.
There is yet no clear consensus on testing. While RT-PCR testing is widespread, its limitations include the need for higher-level laboratory facilities, proper swab sample techniques, and error-free patient sample to laboratory result pathways. Likewise, there is a wide variety of strategies on when to test, with some countries deploying outreach detection programs that seek to pick up as many cases as possible, including the asymptomatic ones, to countries that only test in the hospital. Some countries are even considering handing out COVID-19 discharge cards based on antibody testing[35], which sparked controversy after the World Health Organization stated that “There is currently no evidence that people who have recovered from COVID-19 and have antibodies are protected from a second infection”[36]. Of course, by the time this article is published, many countries that were following a screening strategy may have switched over to another one. To the date of my literature review, there were no large population studies that included diseased and healthy persons to provide us with property statistics for positives in disease and negatives in health. More research must be done on diagnostic testing for COVID-19 in the general population as we are still beset by reasonable uncertainty.
The world is presently in a race to find the solutions that humankind requires for the diagnosis, prevention, and therapy of this novel coronavirus. New papers are coming out each day on any of these critical questions, many published in high-profile journals. We must not let ourselves be swayed by an understandable expectation for a quick success that opens the way for an acritical assessment of the interventions that are being proposed. There have been reports on treatments in small groups without proper controls[37], and many new diagnostic tests for SARS-CoV-2 are being explored and deployed. Each day, news articles tout university efforts to mass-produce ventilators and any new press release is avidly picked up by the mass media and, regrettably, by high-level authorities as well. Many of these experiments will not stand the test of time, and there might not be enough evidence to support the continuing use of the tests or interventions. The research and academic community must insist on following proper methods and proper reporting even in these times of pain and suffering, for we must not repeat the mistakes of the past[38]. The policymakers and political leaders of this time are called upon to make decisions for the benefit of their peoples and communities based on the best available evidence.

