Comunicaciones breves
← vista completaPublicado el 6 de diciembre de 2022 | http://doi.org/10.5867/medwave.2022.11.2618
Experiencia en la implementación de un sistema informático para la gestión de camas hospitalarias
Implementation experience of an informatic system for the management of hospital beds
Abstract
The management of beds within healthcare centers is essential for meeting the health needs of the population. Currently, in Chile there are few computer tools that streamline the functions performed by the Bed Management Units of healthcare centers. The objective of this article is to describe the implementation of a bed management computer system in three hospitals of medium (Modular-La Serena) and high complexity (San José del Carmen-Copiapó y San Juan de Dios-La Serena) of the Chilean public health network. The process used the Framework of dissemination and implementation, which allowed for a consistent flow of bed management, namely: request, allocation of bed, transfer, hospitalization and patient discharge. Likewise, the relevant actors and the minimum variables for the adequate process were identified. The implementation of the system was carried out in stages of validation and configuration of the platform in each healthcare center, user training and follow-up of the start-up. To date, the three hospitals have an operational computer system for managing hospital beds, reporting no difficulties in its use. The next challenge is to carry out a comprehensive evaluation of the impact of the platform, using the indicators agreed upon with the clinical/administrative teams of the health centers.
Main messages
- Hospital bed management is relevant for resource optimization and better care delivery to patients in healthcare facilities.
- Implementing a computerized bed management system should integrate the perspectives of both clinical and administrative stakeholders.
- Implementing a computerized bed management system is an alternative to solve some problems in hospital administration and facilitate patient care.
Introduction
Current global health needs have caused states and institutions to adjust to new forms of healthcare. These increasingly complex dynamics produce a series of challenges for the rational use of resources, particularly in low to middle-income countries [1]. In order to address these new requirements, health systems have adopted a series of measures that facilitate decision-making in the health field. One of them is to have systems that enable a permanent analysis of the resources that support the health system and the relevant processes for its management [2].
The role of informatics systems in healthcare is highly relevant since they allow the capture of helpful information for decision-making, the clinical traceability of the people attended, the improvement of care, the efficiency of resources, and the overall management of healthcare centers [3]. On the contrary, evidence shows that centers with poorly developed information systems have more errors in decision-making, delayed clinical care, and, in some cases, more patient deaths [4]. Another relevant phenomenon is the impact on emergency care units. One study pointed out the impossibility of detecting incomplete tasks in patients' admission, transfer, and discharge due to the lack of computer systems [5].
Chile’s public health system has adopted different strategies to address the lack of technological platforms [6]. However, the development and implementation of information systems have not been uniform across health services. As Lobos and Olivares point out, the health network lacks information systems, and the data gathered are of low quality [7]. In addition to the lack of integration with other technological platforms, there is a phenomenon of low adherence to health information records by clinical teams [8].
One of the critical processes in the administration of the public health system is the management of hospital beds. In Chile, according to data from the Department of Health Statistics and Information (DEIS), by 2021, the public health system had 26 595 beds distributed in low, medium, and high-complexity hospitals [9]. In the international context, Chile is one of the countries of the Organization for Economic Cooperation and Development (OECD) with the lowest number of hospital beds per thousand inhabitants (two per thousand inhabitants) [10]. In particular, the situation in the regions of Atacama and Coquimbo is critical, with 1.74 and 1.75 beds per thousand inhabitants, respectively [9].
Given the shortage of hospital beds and the need for computerized systems that allow better management of this resource, this manuscript aims to describe the implementation of a computerized bed management system in three medium and high-complexity hospitals of the Chilean public health network.
Development
Hospital bed management is a relevant process for the Chilean health system. Due to the importance of optimal management, the Ministry of Health (MINSAL) created the centralized bed management unit (UGCC) in the country’s health services [11]. Currently, this unit is responsible for "managing hospital beds within the public-private health network throughout the country" [11].
The centralized bed management unit works with a national computer platform, in which local units report the situation of each healthcare center with an emphasis on available and occupied critical beds, days of stay, and patient diagnosis [11]. However, the system does not provide real-time information on the flow of patients' admissions and discharges to improve the management of hospital beds.
An alternative to improve the bed management process
The information system for hospital bed management (SIGICAM) was developed at the Universidad de Valparaíso with the support of the Fondo de Fomento al Desarrollo Científico y Tecnológico (FONDEF ID16i20449). The platform had the primary goal of the research group of the Laboratory of Research, Development and Innovation (LABITEC), whose main objective was to create a computer system that would reduce waiting times, particularly in emergency units, through systematic administration during the entire bed management process, as well as providing key information for decision making by the health authorities.
Based on dissemination science for clinical interventions, the implementation and dissemination (I&D) framework was used to develop and implement the hospital bed management information system [12,13]. Implementation and dissemination science is an interdisciplinary knowledge framework that seeks to understand the processes and variables involved in the use of scientific evidence to design and implement policies, programs, and interventions in health services and other contexts.
The Implementation and Dissemination Framework defines the composition of a panel made up of the different agents (information technology (IT) professionals, administrative, managerial, and clinical) to identify the clinical priorities that could be addressed by an informatics system [12,13]. Then, the design and development team converts the clinical priorities into implementation strategies, and finally, the dissemination agents accompany the system implementation process in the health care centers. In this way, the implementation of informatics systems is efficient and effective, as it relies on the feedback and perception of the clinical and administrative teams.
System development process
The platform development process was approached through the collection of information to identify the following:
-
Bed management flow.
-
Actors or professionals involved in the flows.
-
Relevant variables in this process.
To this end, interviews were conducted with key agents in the clinical, administrative, and directive management areas under participatory methodologies [14,15]. These interviews addressed topics related to management processes and further needs to be included in the new hospital bed management system. Regarding the latter, aspects associated with the flow of information among the different professionals and reports required by the Ministry of Health were included. To conduct an adequate triangulation process, a documentary analysis of the national regulations of the Ministry of Health regarding the management of hospital beds was carried out (Table 1).
Consequently, the research team developed the hospital bed management information system based on a coherent flow of bed requests, assignments, transfers, hospitalization, and patient discharge (Figure 1).
Bed management process in the hospital bed management information system platform.
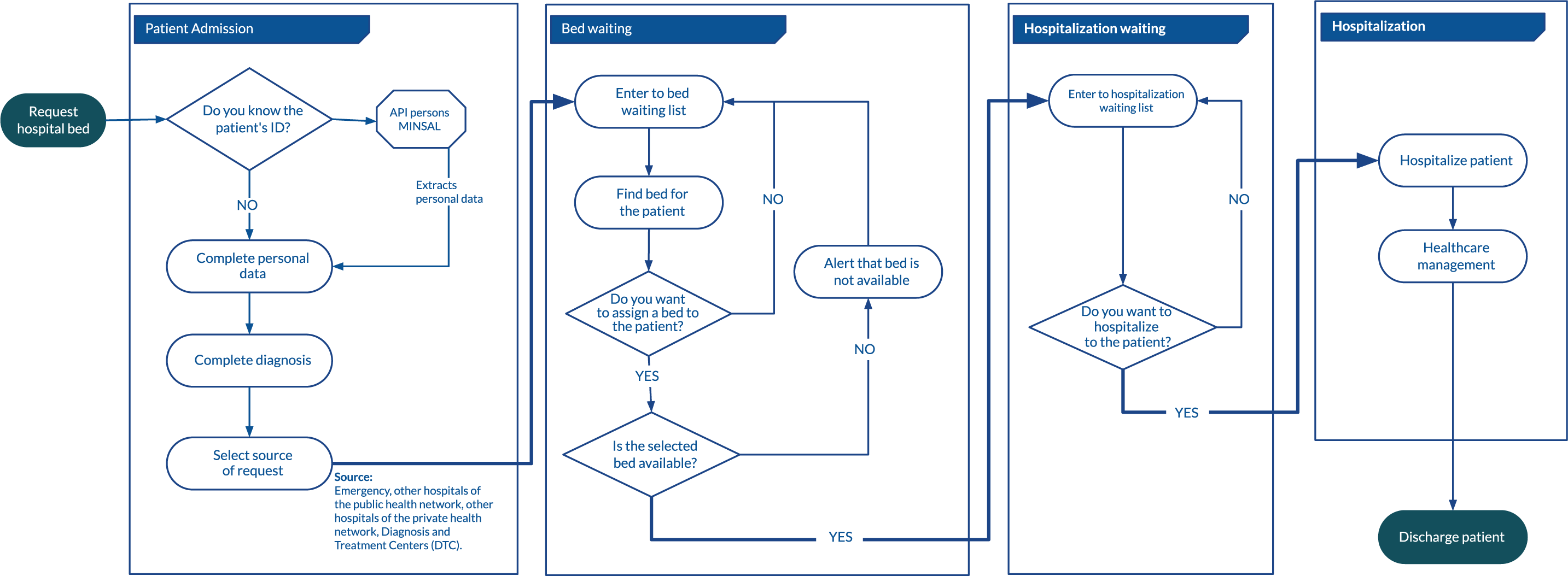
The process flow was specifically defined using the following sub-processes:
Subprocess where health personnel (preferably nurses) make the bed request through the hospital bed management information system, using a form with basic (sociodemographic) and specific data related to the patient’s clinical condition. Given the computer integration between the hospital bed management information system, the Ministry of Health, and the Chilean Civil Registry, the sociodemographic variables are automatically completed using each patient’s identifier (unique tax number, Rut). On average, the bed request form takes two minutes per patient. Once the request subprocess is completed, the information is sent to the bed management unit for the assignment phase.
The subprocess in which bed management teams assign the best available option for the patient, using the clinical and sociodemographic data from the request. The allocation time depends on the number of bed requests, patient turnover, and the rate of hospital discharges per day, among other variables. The computerized bed assignment process takes, on average, 30 seconds. Once the assignment process is completed, the requesting team is alerted through the platform to begin the patient’s hospitalization phase.
Sub-process related to the patient’s arrival at the clinical unit where a bed has been assigned. It is usually the responsibility of the nursing professionals to perform the hospitalization action in the hospital bed management information system, which takes about 30 seconds. During the hospitalization process, this system makes it possible to identify the patient’s traceability through the length of hospital stay, internal transfers to other units of lesser or greater complexity, and the health status of each patient through risk/dependency categorization, falls risk scale, among other measurements.
Subprocess related to the end of the patient’s hospitalization. It is placed when physicians indicate the patient’s discharge according to their health condition. It is the responsibility of the clinical unit nurse to enter administrative data, the date and time of discharge, and the name of the physician responsible for the patient’s discharge. The average time of the discharge subprocess is one minute.
The variables incorporated into the information system for the management of hospital beds were:
-
Sociodemographics (patient identifier, age, gender, country of origin, belonging to a native population, social name, type of social security, and address).
-
Clinical: medical diagnosis, diagnosis in the International Classification of Diseases, 10th edition (ICD-10), risk/dependency categorization, examinations, notification of healthcare-associated infections, among others.
-
Temporality: date and time of bed request, assignment, hospitalization, transfers between units, and patient discharges.
-
Bed characteristics: bed identifier, complexity, bed type. Type of clinical service, type of functional area, among others.
-
User: user identifier, type of user, facility, type and date of action taken.
-
Management: hospital identifier, complexity of the care center, type of clinical unit, type of medical specialty, type of referral, type of visit made, and patient data editing, among others.
With the above, an initial prototype was developed and tested in a virtual and simulated environment of the bed management process. IT aspects were harmonized regarding information backup and user visualization in this instance.
Implementation process
After the platform development and simulation test, a validation process was carried out with the hospital bed management teams of three medium and high-complexity healthcare centers. This stage was relevant because it gave key agents feedback on whether the system developed meets the needs of its users [16], which is an essential step given the magnitude of the intervention in healthcare processes [17]. To review the hospital bed management information system, 12 staff members completed a checklist of the bed management flow and related variables. Strengths and opportunities for improvement of the system were identified.
As a result of the improvement opportunities, the system was adjusted to these new requirements, which were oriented to integrate home hospitalization and healthcare-associated infections units. Including these units established a greater framework of variables, resulting in less room for error in the bed allocation process.
Subsequently, a pilot field test was carried out for validation in two high-complexity healthcare centers in the Atacama and Valparaíso Regions, namely the San José del Carmen Hospital in Copiapó and the Carlos Van Buren Hospital. The validation conducted at the San José del Carmen Hospital in Copiapó was carried out in the adult, pediatrics, and gynecology-obstetrics services, in November 2018, with the participation of 311 staff members. At the Carlos Van Buren Hospital, the field test was executed in October 2019 and had the participation of 329 staff members from clinical (neonatology, pediatrics, and adult) and administrative units. It is important to mention that both healthcare centers required integration with other IT systems related to resource management and clinical records monitoring systems.
Once a stable system was obtained, the massification process was carried out in agreement with the San José del Carmen Hospital in Copiapó, the Modular Hospital in La Serena, and the San Juan de Dios Hospital in La Serena (Table 2). This process was carried out with the referral teams of each healthcare center through the following phases:
The platform was presented to each hospital’s clinical unit related to bed management. System adjustments were established regarding users and responsibilities during the bed management process.
The IT team of the hospital bed management information system installed the bed management platform on the servers of each healthcare center to use the security standards of the Ministry of Health’s computer network. This phase included the creation of credentials for each user of the system.
This consisted of teaching and training clinical/administrative personnel in the proper use of the platform. The training was theoretical-practical and face-to-face at the staff’s units during day and night shifts.
At the end of the training process, along with the reference teams, a date was set for the platform’s implementation. This considered the system’s adoption level during the training and on a day when there was no high demand for hospital beds. Once the start-up was carried out, the team that trained the hospital bed management information system remained present in the healthcare centers to assist with the system’s implementation, doubt resolution, employee re-training and training for those who were absent during the training process, creation of credentials for those who did not have access and to raise new requirements or adjustments to the platform.
The implementation and ease of use of the system were reported as positive by the bed management teams of the three hospitals. This qualitative evaluation was also confirmed during the monitoring process carried out by the hospital bed management information system training teams. The number of follow-up visits decreased as no usability, integration, or system error problems were reported. Once the monitoring process was completed, a meeting was held with the referral team of each care center to establish communication mechanisms in case of system errors or new requirements for the platform’s expansion. Finally, a comprehensive evaluation framework for the hospital bed management information system was co-constructed with the referral teams to measure its impact in different dimensions (Table 3).
Final considerations
The implementation process of the bed management system was successful in the three healthcare centers. The implementation and dissemination framework allowed us to deepen and ensure an adequate set-up by recognizing the key actors and emphasizing the clinical and administrative teams' follow-up in using the platform. In this sense, the information system for hospital bed management, as a tool jointly built with the teams of each hospital, is an active and representative system of the hospital’s dynamism.
Among the challenges of the hospital bed management information system are the comprehensive evaluation of the platform and the widespread use of it in other healthcare centers. Regarding the last point, we expect to involve more healthcare centers, which could generate a macrosystem for bed management in the public healthcare network. This could positively impact decision-making at a higher level in the public health system, making it possible to establish more efficient strategies for managing healthcare networks.
Conclusions
In summary, this experience of collaboration between public institutions demonstrates a successful intervention in implementing an information system that can be replicated in other healthcare centers to strengthen public health in the country.

