Estudios originales
← vista completaPublicado el 9 de mayo de 2024 | http://doi.org/10.5867/medwave.2024.04.2795
Cumplimiento diario del bundle ABCDEF de liberación de los pacientes de cuidados intensivos: estudio descriptivo retrospectivo
Daily compliance of the ABCDEF liberation bundle for patients in the intensive care unit: A retrospective descriptive study
Abstract
Introduction Implementing the ABCDEF bundle has demonstrated improved outcomes in patients with critical illness. This study aims to describe the daily compliance of the ABCDEF bundle in a Chilean intensive care unit.
Methods Retrospective observational study of electronic clinical records of nursing, physiotherapy, and medical professionals who cared for patients over 18 years of age, admitted to an intensive care unit for at least 24 hours, with or without mechanical ventilation. Daily bundle compliance was determined by considering the daily records for each element: Assess pain (element A), both spontaneous awakening trials (element B1) and spontaneous breathing trials (element B2), choice of sedation (element C), delirium assessment (element D), early mobilization (element E), and family engagement (element F).
Results 4165 registered bundle elements were obtained from nursing (47%), physiotherapy (44%), and physicians (7%), including 1134 patient/days (from 133 patients). Elements E and C showed 67 and 40% compliance, while D, A, and B2 showed 24, 14 and 11%, respectively. For B1 and F, 0% compliance was achieved. Compliance was higher in patients without mechanical ventilation for A and E, while it was similar for D.
Conclusions Early mobilization had the highest compliance, while spontaneous awakening trials and family engagement had absolute non-compliance. Future studies should explore the reasons for the different degrees of compliance per bundle element in clinical practice.
Main messages
- Implementing the ABCDEF bundle improves outcomes in patients with critical illness.
- Assessing compliance with recording the ABCDEF bundle is key to designing strategies for improving its implementation.
- This is the first retrospective study with an interdisciplinary approach measuring compliance of recording the ABCDEF bundle.
- Some of the weaknesses of this study are the lack of clarity on the size and direction of the reporting bias due to using electronic clinical records to determine bundle compliance, the single-center data extraction, and the lack of a standardized data entering method based on the bundle criteria.
Introduction
Surviving critical illness is not free from cognitive [1], physical [2], or mental [3,4] complications, which may be present up to five years after discharge from an intensive care unit [5]. This set of complications is known as post-intensive care syndrome [6]. To mitigate this syndrome, a set of seven practices based on the best available scientific evidence called the "intensive care unit ABCDEF liberation bundle was developed:
-
A: Assess, Prevent, and Manage Pain.
-
B: Both Spontaneous Awakening Trials (SAT) and Spontaneous Breathing Trials (SBT).
-
C: Choice of Analgesia and Sedation.
-
D: Delirium, Assess, Prevent and Manage.
-
E: Early Mobility and Exercise.
-
F: Family Engagement and Empowerment [7].
Bundle compliance in more than 6000 patients has been independently associated with an increased likelihood of survival and more days without delirium and coma, even after adjusting for age, illness severity, and mechanical ventilation duration [8]. Another similar study with more than 15 000 patients showed that implementation of all elements had clinically significant improvements in survival, use of mechanical ventilation, coma, delirium, and use of physical restraints, among others [9]. It has been shown that for every 10% increase in total bundle compliance, patients are 7% more likely to survive a hospital stay [8].
Compliance per bundle element varies between 7% and 92%, assessed mainly through surveys [10,11,12,13,14]. So far, only one study has been prospectively performed [9]. In Latin America, there are only reports from Argentina based on surveys of different clinicians [13,14]. In Chile, compliance with some bundle elements is only known from the national practices on sedation, analgesia, and delirium published in 2021 [15], providing an incomplete implementation baseline. However, compliance with the elements of the ABCDEF bundle in an intensive care unit that has not implemented it into its care process is unknown. Therefore, the objective was to retrospectively identify the daily compliance of each element of the ABCDEF bundle based on electronic clinical records in an intensive care unit of an academic center in Chile.
Methods
Design
Retrospective descriptive observational study. We reviewed the electronic clinical records of an eight-bed adult clinical-surgical intensive care unit of an academic center in Chile between March and August 2019 to identify compliance with the elements of the bundle. The clinical record of the subjects was used, assuming the legal framework of Decree No. 41 within the Law 20.584, which establishes in Article 2 that "the clinical record is the mandatory instrument in which the information concerning the different areas related to the health and care of a person is recorded [16]", which has not only a judicial value but also a value for research and quality control of care in healthcare facilities [17]. The standards of the Declaration of Helsinki were followed for this study [18]. This study was reviewed and approved on June 25th, 2020, by the Ethics Committees of the Faculty of Medicine Clínica Alemana Universidad del Desarrollo (No. 2020-40) and the Critical Patient Centre at Clínica INDISA. Due to the retrospective nature of the study, a patient's informed consent waiver was approved. The results are reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for observational studies[19].
Participants
All electronic clinical records of patients meeting inclusion and exclusion criteria were obtained retrospectively following the same protocol as Pun et al. [9]. We included patients aged 18 years and older treated in the intensive care unit for at least 24 hours, with or without mechanical ventilation requirements. Records of patients who died or were transferred and those who required end-of-life care in the first 24 hours were excluded.
Procedure
Data extraction was carried out between May and August 2020. The period between March 1st and August 31st, 2019 (six months) was analyzed retrospectively, considering "one day" from 00:00 to 23:59 hours. One reseracher (FM-M) checked the electronic clinical records each day of stay in the unit to extract clinical, socio-demographic, and bundle-related variables, which were entered into an Excel spreadsheet on the researcher’s computer. Patients who were still in the intensive care unit on August 31st were followed-up until they were transferred, died, or up to 30 days after that day.
Nursing, physiotherapy, and medical professionals could write clinical notes on a given day. The researcher extracting the data registered the number of times per day when bundle elements had been recorded, and therefore, it was possible that a clinical note could contribute to more than one bundle element. For example, if a nursing clinical note referred to having assessed pain (element A) and the level of agitation-sedation (element C), this was counted as two records (one for each element).
Local context
In the participating site of this study, the ABCDEF bundle has not been implemented as part of the clinical and care processes. However, some elements were implemented according to the predecessor bundle (ABCDE) [20] through local protocols for early mobilization (implemented by physiotherapists in charge of providing neuromuscular and cardiorespiratory care with active collaboration in mechanical ventilation [21]), administration of sedation-analgesia (implemented by nurses and physicians) and weaning from mechanical ventilation (implemented by physiotherapists and physicians). The team consisted of one physician per 24-hour shift, three nurses, one physiotherapist, and three healthcare assistants per 12-hour shift, with a professional/patient ratio of 1:8, 1:3, 1:8, and 1:3, respectively. All procedures recorded by the professionals in the electronic clinical records were analyzed.
Operational definitions of the ABCDEF bundle
The elements of the ABCDEF bundle were defined based on Pun et al. [9] protocol. We defined compliance with the ABCDEF bundle as compliance with recording the elements of this bundle in the electronic clinical record. We did not determine full or partial compliance with the bundle, defining compliance as:
-
Element A: recording of at least one pain assessment using a valid and reliable instrument (visual analog scale, numerical analog scale, Behavioral Pain Scale, or Critical Care Observation Tool).
-
Element B was subdivided into:
-
B1 (Spontaneous Awakening Trials) is the recording of at least one sedation interruption trial.
-
B2 (Spontaneous Breathing Trials) is the recording of at least one spontaneous breathing trial.
-
-
Element C: recording of at least one assessment of agitation-sedation using a valid and reliable instrument (i.e., Richmond Agitation Sedation Scale, Sedation Agitation Scale, or other).
-
Element D: recording of at least one delirium assessment using a valid and reliable instrument (e.g., the Confusion Assessment Method for the ICU, the Intensive Care Delirium Screening Checklist, or other).
-
Element E: recording of at least one early mobilization modality (e.g., passive bed mobility, active bed mobility, sitting at the edge of the bed, standing, walking, transfering to an chair, tilt-table, or neuro muscular electrostimulation).
-
Element F: recording of at least one of the following activities performed with a family member/caregiver who has been educated or participated in rounds, lectures, care plans, or bundle-related care.
Eligibility criteria varied according to each element. All days were considered eligible for elements A, C, D, and F. For element B1, only days in which patients received continuous or intermittent sedation infusions were considered, while for element B2, only days in which patients received mechanical ventilation were considered. Only days with a physician’s indication for early mobilization, documented in the electronic clinical record, were eligible for element E. For elements B1 and B2, the outcome of the trial was considered as success or failure, while for the latter, the type of trial used (e.g., T-tube or pressure support) was also identified.
Statistical analysis
Clinical, socio-demographic, and bundle compliance-related continous variables are presented as median and interquartile range, while categorical variables are presented as absolute and relative frequency. The unit of analysis was the patient/day, and bundle compliance was established as the percentage of the number of patient/day where the defined element was present divided by the total number of patient/day eligible. Because the eligibility criteria differ per bundle element, the number of eligible patient/day per element varies. Results are presented separately for patients receiving mechanical ventilation and patients without mechanical ventilation patient/days. Data were analyzed using Microsoft Excel© 2018.
Results
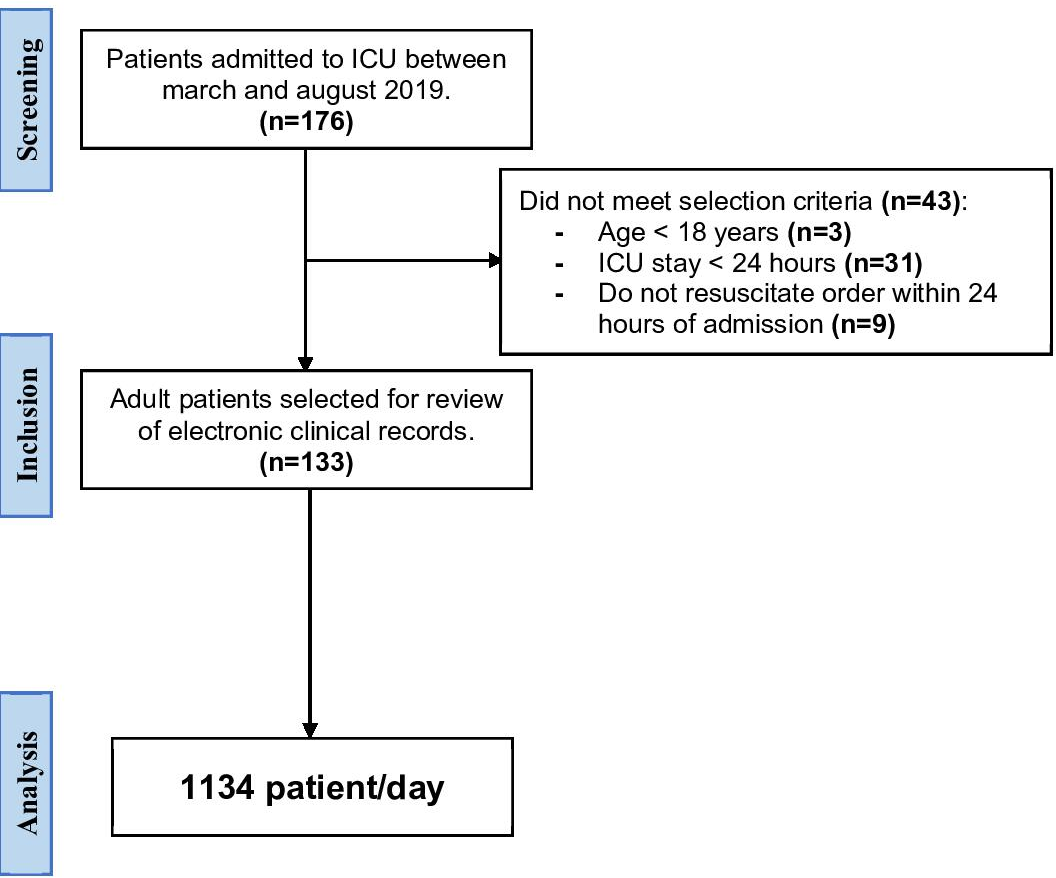
During the recruitment period, 176 patients were admitted, of which 133 were included in the analysis (Figure 1). Of the 133 patients included (Table 1), 1134 patient/days were obtained, comprising 4165 bundle element records, of which 1944 (47%) were from nurses, 1851 (44%) from physiotherapy, and 297 (7%) from physicians (Table 2).
Flow chart of selection of patient/days.
Daily compliance with the ABCDEF bundle
Daily compliance per bundle element was determined from the 4165 records obtained in the 1134 patient/days, presented comparatively in patient/days with and without mechanical ventilation (Table 3). For elements A, C, D, and F, compliance was 14, 41, 24 and 0%, respectively. For element B1, 51% of the patient/days were eligible, and 0% compliance was obtained, while for B2, 35% of the patient/days were eligible, and 11% compliance was obtained. Element E obtained a compliance rate of 67%, considering 79% of the patient/days eligible. Details regarding the information used to determine compliance for each bundle element are presented in Table 4.
Discussion
In this retrospective study, compliance with recording the ABCDEF bundle elements was heterogeneous. Early mobilization (E) and choice of sedation (C) were the most recorded, while spontaneous awakening trials (B1) and family engagement were the least recorded (F). Nurses and physiotherapists records were the main source of information on bundle compliance. The retrospective nature of our study provides a genuine approach by not modifying or preempting the recording behavior of the healthcare professionals.
This is the first retrospective study measuring the compliance with recording the bundle including the F element. Compliance with the bundle elements varies as reported in the literature between 7 and 92% [9,10,11,12,13,14]; five of the studies mentioned above correspond to surveys, two were directed only to physicians [11,12], another to nurses [10] and the other two were answered by an interdisciplinary team [13,14]. In contrast, our work is longitudinal and using an interdisciplinary approach to bundle compliance. The only prospective study to date is Pun et al. [9], which included more than 15 000 patients. Our study had a similar structure for data extraction, and, in general, we found lower compliance with recording. In our study, compliance with recording seems to be as expected for a unit that has not implemented the bundle into its care processes and only has experience with some of the elements through internal protocols. On the contrary, the Intensive Care Unit Liberation Collaborative provided expert support for a year and a half in more than 68 intensive care units [22,23], which could explain the better results they found.
In Chile, the experience implementing the bundle is recent and limited. In 2019, recommendations for analgesia, sedation, and neuromuscular blockade in adult patients with critical illness were published [24]. Subsequently, a national multiprofessional survey was conducted with the aim of identifying the national practices of the health care team concerning this topic [15]. For this reason, only the results of elements B1 (31%), C (97%), and D (48%) can be compared at the local level. We found that compliance was less than half of what was reported in the national study for all three elements. This may be associated with a reporting bias where practitioners indicate the behavior they consider optimal, but this does not necessarily reflect what occurs in clinical practice. There is also the possibility that the professionals' reporting is in line with what they do in practice, but their recording in the clinical record is substandard.
There is a positive attitude among both family and healthcare professionals toward the inclusion of family members in the care of their loved ones in the intensive care unit. However, it is still unknown how this process should be structured and the potential outcomes for patients [25]. Therefore, the lack of administrative structure that promotes the inclusion of family members and/or the lack of recording could explain the 0% compliance in our study. This is consistent with the result of an international survey, where 77% of physicians in South America reported that they do not have a 24-hour open visitation policy for family members [11], similar to the 93% reported in Argentina [13]. Therefore, strategies involving family members should be developed to understand their impact on patient outcomes.
Although element E obtained higher compliance than the 29% reported by Pun et al. [9], only 14% of the physiotherapy modalities recorded were in patient/days with mechanical ventilation, with bed mobility records predominating and only in one patient/day walking was recorded (Table 4). Our results are consistent with what has been described in the literature since patients in the intensive care unit spend more than 90% of their time inactive [26,27,28,29]. Similar is the case for element D, which obtained 24% compliance. Currently, there is a large difference in the incidence of delirium reported in the literature. Ten percent of the recorded assessments were reported as positive for the Confusion Assessment Method for the ICU (CAM-ICU), with this incidence being 12.3% in patient/days on invasive mechanical ventilation (Table 4). However, the reported incidence is 87%, and delirium in patients with critical illness is associated with increased mortality [30]. A late evaluation could explain the underestimation of delirium since 66.2% of the records were made in patient/days who did not receive mechanical ventilation (Table 4), which decreases the chances of detecting the condition when patients were ventilated and could have developed the condition [31].
This study has several limitations that should be mentioned. First, the size and direction of the reporting bias associated with the use of electronic clinical records to determine bundle compliance is unclear. Second, the findings are not generalizable as they represent the reality of a single center. Nevertheless, we believe that the methodology used can be replicated in other centers to determine baseline bundle compliance and establish quantifiable goals to improve implementation. Third, since we did not have a standardized database according to the bundle criteria, we excluded records that were not explicit in recording compliance with the bundle elements in order to maintain rigor in data extraction. This procedure was performed only by the principal investigator (FM-M).
Future research should consider the professional roles of intensive care unit teams implementing the bundle to explore its relationship with compliance and patient outcomes, as in the ongoing randomized clinical trial by Sosnowski et al. [32]. In addition, future studies should analyze bundle compliance and its impact on patients, considering centers that do not perform sedation interruption trials and have light sedation protocols. As in elements A, C, and D, the rest of the elements should define compliance according to the use of measurement instruments, such as peripheral muscle strength or mobility in element E [33]. Finally, to improve knowledge translation, human behavioral assessment models, such as the behavioral model of capability, opportunity, and motivation [34] would help explore the potential reasons clinicians do or do not implement the bundle using mixed-methods research.
Conclusions
Based on the electronic clinical records, elements E and C were identified as having a higher compliance with recording, followed by elements D, A, and B2. No recording of compliance with elements B1 and F was identified. Nursing and physiotherapy staff contributed the most to recording compliance with the bundle. The results of this study establish a baseline for improvements in the implementation of the bundle in intensive care units where it has not been implemented as standard of care.

