Research papers
← vista completaPublished on June 23, 2020 | http://doi.org/10.5867/medwave.2020.05.7939
Incidence, risk factors and case fatality rate for hip fracture in Chile: A cross-sectional study based on 2017 national registries
Incidencia, factores de riesgo y letalidad de la fractura de cadera en Chile: estudio transversal sobre registros nacionales de 2017
Abstract
Purpose To describe the incidence of hip fracture in Chile during 2017, identify risk factors for in-hospital mortality, and estimate annual case fatality rate.
Method The study design was cross-sectional and analytical. We obtained the registries of all patients from the Chilean Ministry of Health who were treated for hip fracture between January 1, 2017, and December 31, 2017. We used multivariate logistic regression to estimate the risk factors for in-hospital mortality. The annual case fatality rate was calculated using the probabilities obtained by estimating a logistic regression model in previous work. The estimated crude mortality rate per 100 000 persons was compared with that of cancer, as reported by the Ministry of Health.
Results During 2017, 7421 hip fractures occurred, resulting in an incidence of 40 per 100 000 persons. Of these, 1574 (21.21%) cases did not undergo surgery. In-hospital mortality was found to be associated with no surgery (odds ratio 8.32, 6.20 to 11.17), and being treated in a public hospital (odds ratio 1.62, 1.00 to 2.68). The estimated annual case fatality rate was 0.30 (0.27 to 0.33), and the crude mortality rate per 100 000 persons was 10.78 (9.66 to 11.71).
Conclusion Hip fractures mainly affect the population over 60 years old and women. Chile has an excessively high rate of non-operated patients compared to international reports. There is a significant difference between care in a public hospital compared to private clinics in terms of volume, access to surgery, hospital stay, in-hospital mortality, and estimated case fatality rate.
Main messages
|
Introduction
Hip fracture is a frequent event, especially in patients older than 60, and requires an interdisciplinary approach[1]. Chile is no stranger to the realities of an aging population; therefore, an increase in the occurrence of hip fractures can be expected.
The first step for intervention in health problems is to know the magnitude[2]. The proportion of patients who died one year after the event, known as the case fatality rate, is one of the leading health indicators of hip fracture, which has traditionally been reported as one-third of the population. Most recent reports show a case fatality rate of 23.3% in Europe and 24.9% in the United States[3], while in Asia, countries have managed to decrease this rate to less than 15%[4].
In Chile, two types of health institutions coexist—health-care centers belonging to the public network and private centers. Citizens can sign up to a public insurer called the National Health Fund (FONASA, in Spanish), or private insurers, known as ISAPREs (Instituciones de Seguridad Previsional). Patients affiliated with the National Health Fund can be treated in the public health-care sector or choose to receive medical attention in a private health-care center if they can afford it. Patients affiliated with ISAPREs are cared for in the private system most of the time, yet in some cases, especially outside the capital, patients are bound to seek medical care in the public sector. Between 75% and 80% of the inhabitants in Chile are affiliated with the National Health Fund[5].
The purpose of this study is to describe the incidence of hip fracture in Chile during 2017, to identify risk factors for in-hospital mortality, and to estimate the case fatality rate. The analysis focused on patients over 60.
Methods
An analytical cross-sectional study was designed and approved by our institution’s ethics committee. The Chilean Health Ministry was queried through the Freedom of Information Act, to report all the patients who had been treated for hip fractures between January 1, 2017, and December 31, 2017. The request included every patient’s date of birth, sex, date of admission, date of discharge, date of surgery, institution that granted treatment, in-hospital death, if the patient was alive as of July 30, 2019, and, if diseased, the date of death. The information was received, except for the date of surgery and if the patient was alive as of July 30, 2019. We were not able to obtain this information despite several formal attempts to retrieve it. Only the data on whether or not the patient underwent surgery was informed. The search was conducted for codes: s72.0 (head and neck fracture of the femur), s72.1 (pertrochanteric fracture), and s72.2 (subtrochanteric fracture of the femur), according to the 10th International Classification of Diseases. The information was provided using a unique code per patient to identify cases that were transferred from one center to another for the same event, avoiding double registration.
Continuous variables are summarized in median, range, and interquartile range. In the categorical variables, absolute and percentage frequency were used. The nonparametric medians comparison test was used to compare continuous variables, while the Fisher test was used to compare categorical variables. A p-value < 0.05 was interpreted as significant.
The general population data to estimate the incidence were obtained from the 2017 statistical compendium published by the National Statistics Institute of Chile[5].
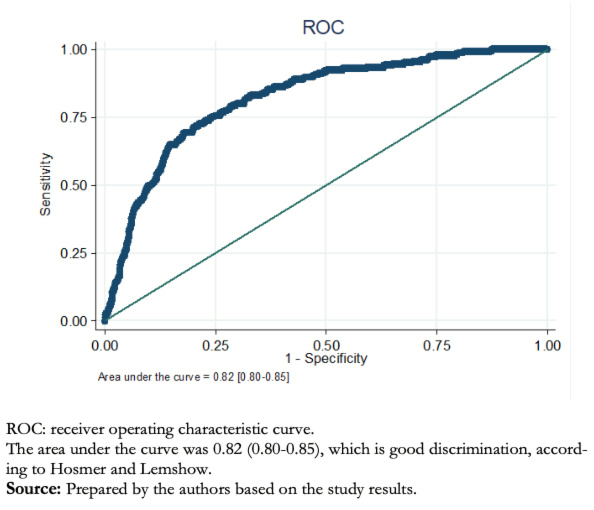
Multivariate logistic regression was estimated to assess the risk factors for in-hospital mortality. Variables were included in the model if they reached a probability of less than 0.05. The Hosmer-Lemeshow goodness of fit test was used to validate the model. Receiver Operating Characteristic curve was constructed to estimate discrimination capacity.
To estimate the one-year case fatality rate, the probabilities reported in a previous study were used, in which mortality was compared between a public and a private center in Chile. This study shows that the probability of dying at one-year after a hip fracture treated in a public center is 0.21 (95% confidence interval: 0.19 to 0.23) if the patient underwent surgery and 0.61 (95% confidence interval: 0.54 to 0.68) if the patient did not undergo surgical treatment. While in a private center the probability is 0.14 (95% confidence interval: 0.12 to 0.16) if the patient underwent surgery and 0.49 (95% confidence interval: 0.41 to 0.58) if the patient was not treated with surgery[6].
The crude death rate per 100 000 inhabitants was calculated using the estimated number of deaths in patients older than 60 divided by the total population of Chile, as reported by the Chilean National Statistics Institute[5].
Finally, the estimated total number of deaths is compared to the total number of deaths by cancer that occurred in Chile during 2016, according to the Ministry of Health[7]. Also, the crude death rate estimated per 100 000 habitants is compared to that reported by the Ministry of Health for each type of cancer[8]. 95% confidence intervals were determined, and the Stata version 15 program (StataCorp LP, College Station, Texas, USA) was used.
Results
General data
A total of 7421 hip fractures were treated in Chile in 2017, of which 6542 (88.15%) were patients older than 60. The median age was 81 (range, 1 to 106; interquartile range, 72 and 88). Women are the most affected with 5393 cases (72.67%). Table 1 summarizes the variables studied by age group.
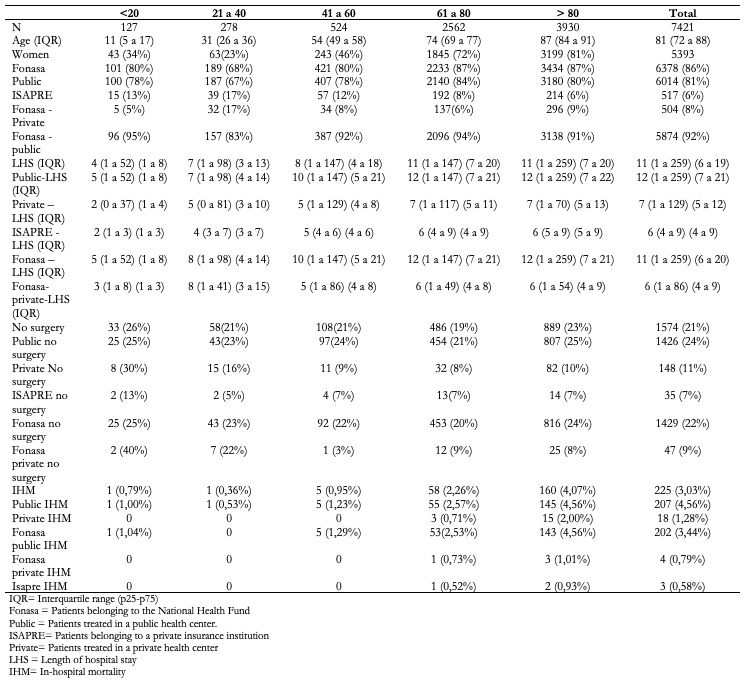 Full size
Full size Incidence
An incidence of 40 cases per 100 000 inhabitants was estimated for the general population, while in those over 60, the incidence was 224 per 100 000 inhabitants. In women, the incidence was 57 per 100 000 women, and 316 per 100 000 women older than 60, while men had an incidence of 16 per 100 000 and 112 per 100 000 older than 60. The incidence of hip fracture is higher in patients belonging to the National Health Fund in those over 60 and in the female population, as shown in Table 2. The incidence by region in patients over 60 is shown in Table 3; the highest incidence was found in the Metropolitan (XIII) and Valparaíso (V) regions.
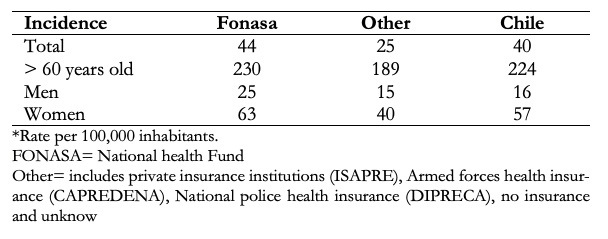 Full size
Full size Length of hospital stay
The median length of hospital stay was 11 days (range, 1 to 259; interquartile range, 6 to 19). In patients older than 60, the median length of hospital stay was 11 days (range, 1 to 159; interquartile range, 7 to 20). Patients older than 60 affiliated with the National Health Fund have a median hospital stay length of 12 days (range, 1 to 259; interquartile range, 7 to 21), while patients older than 60 affiliated with private insurance institutions have a median length of hospital stay of 6 days (range, 1 to 117; interquartile range, 5 to 9); this difference was statistically significant (p < 0.000). When comparing patients older than 60 who were affiliated with the National Health Fund and who were treated in a public health center (n = 5271) with those over 60 who were affiliated with the National Health Fund but treated in private centers (n = 436), the length of hospital stay was 12 days (range, 1 to 259; interquartile range, 7 to 22) and six days (range, 1 to 54; interquartile range, 4 to 9) respectively. This difference was significant (p < 0.000) (Table1).
Surgical treatment
A total of 5847 patients (78.79%) underwent surgery, while 1574 (21.21%) did not undergo surgery. The number of patients older than 60 without surgical intervention affiliated with the National Health Fund was 1280 (22.41%), while 27 patients (6.60%) affiliated with private insurance institutions did not undergo surgery. This difference was statistically significant (p < 0.000).
When patients are over 60 and affiliated with the National Health Fund, the odds ratio of not receiving surgery was 4.09 (2.75 to 6.07). The risk remains significant if the patient is affiliated with the National Health Fund and is between 60 and 80 years old (odds ratio, 3.5; 95% confidence interval, 1.98 to 6.21) or is over 80 years old (odds ratio, 4.45; 95% confidence interval, 2.57 to 7.70).
Patients affiliated with the National Health Fund and over 60 years old treated in a private health center have an odds ratio of 3.33 ( 95% confidence interval, 2.36 to 4.70) to undergo surgery compared with patients affiliated with the National Health Fund and over 60 but treated in a public health center. The I and XV regions have a proportion of patients with a hip fracture that underwent surgery greater than 90%, while regions II and IV have above 40% of non-surgical treatment for hip fracture. The proportion of patients treated with surgery by region in Chile is shown in Table 3.
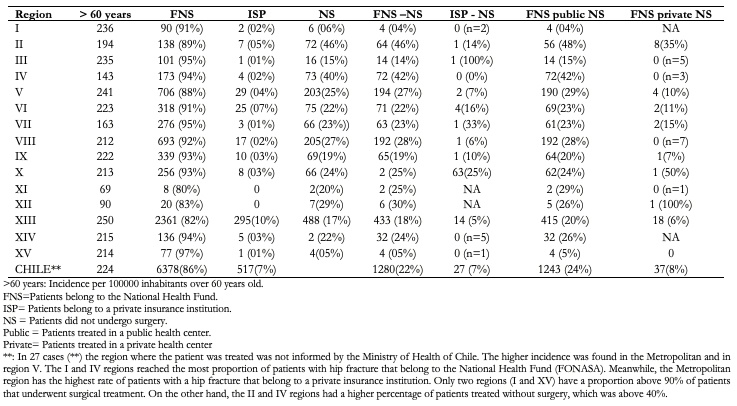 Full size
Full size In-hospital mortality
The number of patients who died during hospitalization was 225 (3.03%), of whom 219 (97.4%) were older than 60. Three patients (0.73%) older than 60 affiliated to a private insurance institution died in the hospital, while the number of patients older than 60 affiliated to the National Health Fund who died in the hospital was 201 (3.52%). The odds ratio to die for a patient older than 60 who was affiliated with the National Health Fund, was 5.72 (95% confidence interval, 1.82 to 17.94) compared to a patient over 60 who was affiliated with ISAPRE. The number of patients affiliated with the National Health Fund older than 60 and treated in a public health care center who died in the hospital was 197 (3.74%), while the number of in-hospital deaths of patients older than 60 belonging to the National Health Fund treated in a private health care center was 4 (0.92%). The estimated odds ratio was 4.20 (95% confidence interval, 1.55 to 11.35).
The estimated multivariate logistic model for in-hospital mortality shows that the significant risk factors were not performing surgery (odds ratio, 8.32; 95% confidence interval, 6.20 to 11.17), being male (odds ratio, 1.55; 95% confidence interval, 1.14 to 2.10), age (odds ratio, 1.05; 95% confidence interval, 1.03 to 1.06), being treated at a public health center (odds ratio, 1.62; 95% confidence interval, 1.00 to 2.68) and the length of hospital stay (odds ratio, 1.01; 95% confidence interval, 1.00 to 1.02). The estimated Receiver Operating Characteristic curve has an area under the curve of 0.82 (95% confidence interval, 0.80 to 0.85) (Figure 1), and probability in the goodness of fit test was 0.40. Therefore, the leading risk factor for in-hospital mortality adjusted for age, sex, type of facility, and hospital stay is not to undergo surgery (Figure 2).
 Full size
Full size 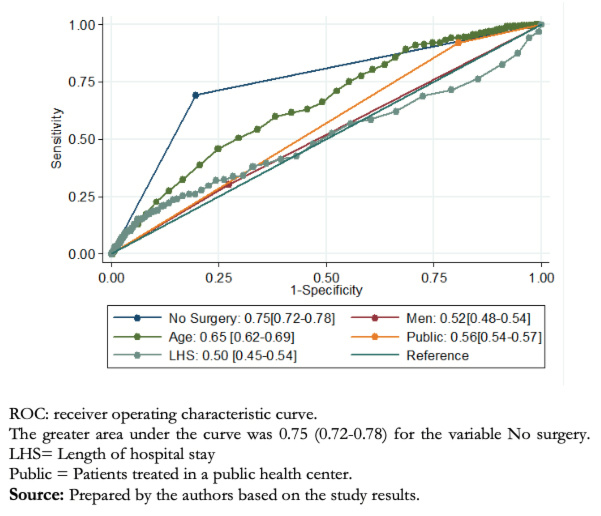 Full size
Full size Estimation of one-year case fatality rate
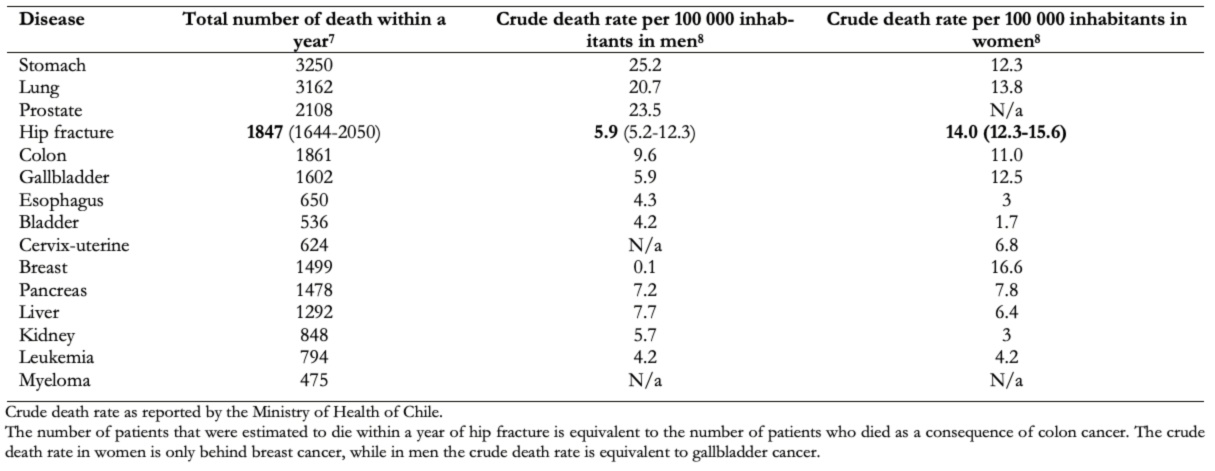
The estimated one-year case fatality rate was 0.28 (95% confidence interval, 0.25 to 0.34), accounting for 1847 (95% confidence interval, 1644 to 2050) patients who died within one year after a hip fracture. The crude death rate per 100 000 inhabitants was 5.9 (95% confidence interval, 5.2 to 12.3) in male patients and 14.0 (95% confidence interval, 12.3 to 15.6) in female patients. The estimated case fatality rate of patients treated in private institutions was 0.17 (95% confidence interval, 0.15 to 0.19) and 0.30 (95% confidence interval, 0.27 to 0.34) for patients treated in public health-care centers. Table 4 compares the number of deaths and the crude death rate per 100 000 inhabitants to cancer deaths in Chile by type, as reported by the Ministry of Health.
 Full size
Full size Discussion
The incidence of hip fracture in Chile in 2017 was 40 per 100 000 inhabitants, exceeding the reported global incidence for gastric cancer (15.7), lung cancer (31.5), and prostate cancer (29.3)[7]. A linear increase in the incidence of hip fracture is expected worldwide, mainly due to an aging population, and Chile is not an exception[9].
The incidence of hip fracture in the population that is affiliated to the National Health Fund is higher than the population that is affiliated to private insurance institutions, resulting in higher demand for the public health care sector. This is reflected in the longer length of hospital stay reported in this study, which doubles the length of hospital stay in private health care centers. Even though the waiting time for surgery could not be obtained from the Ministry of Health, it has been previously reported that the waiting time for surgery is approximately two-thirds of the hospital stay[6]. It must be highlighted that waiting time for surgery is a parameter that significantly influences the one-year case fatality rate in hip fracture[10],[11],[12]. The international standard recommends that patients undergo surgery within three days of admission[13].
The standard treatment for a hip fracture is surgery[14]. We found an excessive number of patients who do not receive surgical procedures (22%) compared to international publications. In Northern Ireland, a study covering 15 years found that 1.3% of the patients did not undergo surgery[9]. In our study, the proportion of patients who did not undergo surgery was significantly higher in the public health care sector (24%) compared to the private sector (11%); however, both proportions are higher than the international reported standards.
In-hospital mortality in Europe ranges from 3.39% in Sweden to 7% in the United Kingdom[3], while in our study, it was 3.35%. Although it is lower than the reported in European countries, we consider that this was mainly confounded by the high number of patients who do not undergo surgery. On the other hand, once more, there is a significant difference between in-hospital mortality in the public sector compared to the in-hospital mortality of the private sector.
The estimated one-year mortality is excessive, especially in public health care centers. In China, the one-year case fatality rate after hip fracture in patients between 95 and 100 years of age is 0.28[4], which is less than the estimated for the Chilean population over 60 years old treated in a public health care center. Likewise, when compared to European countries, the estimated one-year case fatality rate in the Chilean public facilities would be in penultimate place, only surpassing the 0.34 one-year case fatality rate reported by Hungary[3]. We consider that the main factors that can explain this are the high proportion of patients who do not receive surgery and the waiting time for surgery[15]. The magnitude of the problem is evident when comparing the estimate of the total number of deaths and the crude death rate per 100 000 with specific cancers.
If Chile had a preventive and curative program for hip fracture as it does for cancer care, the probability of dying a year after a hip fracture could be cut in half. The estimated total number of deaths is equivalent to the number of deaths from colon cancer, which ranks fourth by type of cancer[7]. Furthermore, the crude mortality rate per 100 000 population in women is only surpassed by breast cancer[8].
Hip fracture management must be interdisciplinary. It must begin with a screening for osteoporosis, a silent epidemic for which there are no incidence data in our country[16]. Moreover, sarcopenia is another risk factor that increases the fragility of patients due to a higher risk of falls[17]. Finally, approximately half of the patients who suffer a hip fracture have already consulted in the emergency room for a fall, so it is a specific group of patients that require a focused effort to prevent hip fractures[18].
Once the hip fracture has occurred, the patient should be admitted to the hospital, surgical treatment should be performed as soon as possible, and only be postponed if the patient requires an intervention that exceeds the risk of delaying the surgery[12]. Non-surgical treatment should only be used in a limited number of patients when the surgical risk is excessive[13]. A patient undergoing surgery for hip fracture grade IV according to the anesthetic risk classification by the American Association of Anesthesia has a probability of dying in the first three days post-surgery less than 0.02[19]. This risk must be compared to the one-year mortality of patients that do not receive surgical treatment, which reaches 60%[20]. The echocardiogram is a scarce resource in the public health sector of Chile, so its use in patients that require surgical treatment for fracture must not delay the surgery and should be reserved for selected cases. The main indication for echocardiogram according to the perioperative cardiovascular guidelines for evaluating patients undergoing noncardiac surgery of 2014 is decompensation in the prior month due to a known cardiac condition or if a new condition arises[21]. Additionally, there is an increasing interest in echocardiogram training from anesthesiologists; this must be encouraged to avoid delaying surgery. Finally, interdisciplinary treatment must include geriatricians who should be responsible for prevention to in-hospital and post-discharge care. A pathway involving geriatric care has been shown to improve the outcomes in hip fracture[1].
There is an important gap between the public health sector and the private health care sector in Chile in terms of volume, length of hospital stays, the proportion of surgical treatment, and in-hospital mortality. Furthermore, the estimated one-year case fatality rate increases the problem. Inequity has been a crucial issue in Chile in recent decades, with the quality of public health care representative of this inequality[22]. As recently as 2019, there have been intense protests about these inequities, and the quality of public health care is a central issue[23].
The Explicit Health Guarantees—a set of benefits guaranteed by law that guarantee access, opportunity, financial protection and quality of care in a limited list of diseases—was the major reform in Chilean public health in the last 20 years. For example, after acute myocardial infarction was included, the annual mortality decreased significantly[24]. We consider that our study presents solid arguments to include hip fracture in the Explicit Health Guarantees, including screening and treatment of osteoporosis, access to exercise programs to prevent falls, and access to surgical treatment as soon as possible. Scotland was able to decrease the one-year case fatality rate from hip fractures only by systematically auditing, monitoring, and registering all cases[25]. The Society of Orthopedics and Traumatology of Chile, as well as other scientific societies, should be actively involved in developing national guidelines for the treatment of hip fracture, as adherence to national guidelines has had a positive impact on hip fracture mortality[26].
The main limitation of this study is the refusal by public institutions to provide information about the date of surgery and date of death of patients; this prevented knowing the full reality of the 2017 cohort. However, we consider that the estimations included in this report are reliable; notwithstanding, this is also another argument for insisting on the need to have national registers that allow planning, especially in health conditions with high incidence and mortality rates.
Conclusions
In conclusion, hip fracture in Chile mainly affects the general population over 60 and women. A high proportion of patients that did not receive surgical treatment was found, of which the majority were patients belonging to the public health care sector. There is a significant difference between patients treated in a public or a private health care center in terms of volume, hospital stay, in-hospital mortality, and access to surgery. The estimated one-year case fatality rate was higher in the public health care sector compared to the private sector. Hip fracture is a strong candidate to be part of the Explicit Health Guarantees.
Notes
Authorship contributions
MB: Conceptualization, methodology, formal analysis, research, writing manuscript, project administration. AM: Methodology, resources, supervision, project administration. JB: Validation, research, writing and revising manuscripts, project administration. DR: Validation, writing and revising manuscript, project administration. CB: formal analysis, resources, writing and revising the manuscript, visualization and administration of the project.
Acknowledgments
The first author acknowledges the support of Leonel Barahona.
Competing interests
The authors declare that they have no conflicts of interest.
Funding
The authors did not receive funding to complete this study.
Ethics
On June 19, 2019, the ethics committee of the Hospital Clinic of Universidad de Chile approved this research.
Data access
According to the ethics committee of our institution, the data repository can be accessed if an accredited researcher makes a formal request for access to the ethics committee through the corresponding author.
From the editors
The original version of this manuscript was submitted in Spanish. This English version was submitted by the authors and has been copyedited by the Journal.

