Systematic reviews
← vista completaPublished on December 10, 2020 | http://doi.org/10.5867/medwave.2020.11.8080
Remdesivir for the treatment of COVID-19: a living systematic review
Remdesivir para el tratamiento de COVID-19: una revisión sistemática viva
Abstract
Objective Provide a timely, rigorous and continuously updated summary of the evidence on the role of remdesivir in the treatment of patients with COVID-19.
Methods Eligible studies were randomized trials evaluating the effect of remdesivir versus placebo or no treatment. We conducted searches in the special L·OVE (Living OVerview of Evidence) platform for COVID-19, a system that performs regular searches in databases, trial registries, preprint servers and websites relevant to COVID-19. All the searches covered the period until 25 August 2020. No date or language restrictions were applied. Two reviewers independently evaluated potentially eligible studies according to predefined selection criteria, and extracted data on study characteristics, methods, outcomes, and risk of bias, using a predesigned, standardized form. We performed meta-analyses using random-effect models and assessed overall certainty in evidence using the GRADE approach. A living, web-based version of this review will be openly available during the COVID-19 pandemic.
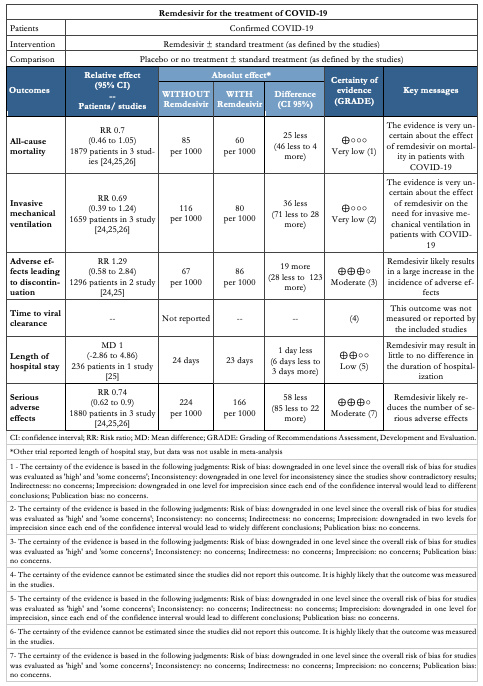
Results Our search strategy yielded 574 references. Finally, we included three randomized trials evaluating remdesivir in addition to standard care versus standard care alone. The evidence is very uncertain about the effect of remdesivir on mortality (RR 0.7, 95% CI 0.46 to 1.05; very low certainty evidence) and the need for invasive mechanical ventilation (RR 0.69, 95% CI 0.39 to 1.24; very low certainty evidence). On the other hand, remdesivir likely results in a large increase in the incidence of adverse effects in patients with COVID-19 (RR 1.29, 95% CI 0.58 to 2.84; moderate certainty evidence).
Conclusions The evidence is insufficient for the outcomes critical for making decisions on the role of remdesivir in the treatment of patients with COVID-19, so it is impossible to balance potential benefits, if there are any, with the adverse effects and costs.
PROSPERO registration number CRD42020183384
Main messages
- The evidence is very uncertain about the effects of remdesivir on mortality and the need for invasive mechanical ventilation in patients with COVID-19.
- Remdesivir likely results in a large increase in the incidence of adverse effects leading to discontinuation.
- Remdesivir may result in little to no difference in the duration of hospitalization.
- Multiple ongoing trials should shed light on the actual role of remdesivir in patients with COVID-19.
Introduction
COVID-19 is an infection caused by the SARS-CoV-2 coronavirus[1]. It was first identified in Wuhan, China, on 31 December 2019[2]; seven months later, more than fifteen million cases of contagion had been identified across 188 countries[3]. On 11 March 2020, the WHO characterized the COVID-19 outbreak as a pandemic[1].
While the majority of cases result in mild symptoms, some might progress to pneumonia, acute respiratory distress syndrome, and death[4],[5],[6]. The case fatality rate reported across countries, settings and age groups is highly variable, but it ranges from about 0.5% to 10%[7]. In hospitalized patients, it has been reported to be higher than 10% in some centers[8].
One of the strategies underway to identify effective interventions for COVID-19 is repurposing drugs that have been used for the treatment of other diseases. Remdesivir is among these investigational medications. It is a directly acting antiviral agent, initially developed for the treatment of Ebola virus during the 2014 outbreak in Western Africa[9]. Remdesivir displays antiviral activity against many RNA viruses, including SARS-CoV-2, in both in vitro[10] and animal studies[11].
Following the publication of the ACTT-1, a trial conducted by the National Institute of Allergy and Infectious Diseases (NIAID), the US Food and Drug Administration issued an emergency use authorization of remdesivir for the treatment of COVID-19[12].
However, the results of ACTT-1 were questioned immediately, particularly for the decision to stop it early for benefit[13]. On the other hand, the decision of the United States government to buy virtually all stocks of the drug generated an urgent need for independent, transparent information about the effects of remdesivir on COVID-19.
Using innovative and agile processes, taking advantage of technological tools, and resorting to the collective effort of several research groups, this living systematic review aims to provide a timely, rigorous and continuously updated summary of the evidence available on the effects of remdesivir in patients with COVID-19.
Methods
This manuscript complies with the 'Preferred Reporting Items for Systematic reviews and Meta-Analyses' (PRISMA) guidelines for reporting systematic reviews and meta-analyses[14] (see Appendix 1 - PRISMA Checklist).
A protocol stating the shared objectives and methodology of multiple evidence syntheses (systematic reviews and overviews of systematic reviews) to be conducted in parallel for different questions relevant to COVID-19 was published elsewhere[15]. The review was registered in PROSPERO with the number CRD42020183384, and a full protocol was made available[16].
Search strategies
Electronic searches
We used the search strategies already developed in the L·OVE (Living OVerview of Evidence) platform, a system that maps the evidence to different research questions. The full methods to maintain L·OVE are described in the website, but the process to devise the search strategies can be briefly described as:
● Identification of terms relevant to the population and intervention components of the search strategy, applying Word2vec technology[17] to the corpus of documents available in Epistemonikos Database.
● Discussion of terms with content and methods experts to identify relevant, irrelevant and missing terms.
● Creation of a sensitive boolean strategy encompassing all the relevant terms.
● Iterative analysis of articles missed by the boolean strategy, and refinement of the strategy accordingly.
All the information in the L·OVE platform comes from a repository developed and maintained by Epistemonikos Foundation through the screening of different sources relevant to COVID-19. At the time of releasing this article, this repository included more than 66 989 articles relevant to the Coronavirus disease, coming from the following databases, trial registries, preprint servers and websites relevant to COVID-19: Epistemonikos database, Pubmed, EMBASE, ICTRP Search Portal, Clinicaltrials.gov, ISRCTN registry, Chinese Clinical Trial Registry, IRCT - Iranian Registry of Clinical Trials, EU Clinical Trials Register: Clinical trials for covid-19, NIPH Clinical Trials Search (Japan) - Japan Primary Registries Network (JPRN) (JapicCTI, JMACCT CTR, jRCT, UMIN CTR), UMIN-CTR - UMIN Clinical Trials Registry, JRCT - Japan Registry of Clinical Trials, JAPIC Clinical Trials Information, Clinical Research Information Service (CRiS), Republic of Korea, ANZCTR - Australian New Zealand Clinical Trials Registry, ReBec - Brazilian Clinical Trials Registry, CTRI - Clinical Trials Registry - India, DRKS - German Clinical Trials Register, LBCTR - Lebanese Clinical Trials Registry, TCTR - Thai Clinical Trials Registry, NTR - The Netherlands National Trial Register,PACTR - Pan African Clinical Trial Registry, REPEC - Peruvian Clinical Trial Registry,SLCTR - Sri Lanka Clinical Trials Registry, medRxiv Preprints, bioRxiv Preprints, SSRN Preprints, WHO COVID-19 database.
The last version of the methods, the total number of sources screened, and a living flow diagram and report of the project is updated regularly on the website[18].
The repository is continuously updated[18], and the information is transmitted in real time to the L·OVE platform; however, it was last checked for this review the day before release on 25 August 2020. The searches covered the period from the inception date of each database, and no study design, publication status, or language restriction was applied.
The following strategy was used to retrieve from the repository the articles potentially eligible for this review: coronavir* OR coronovirus* OR betacoronavir* OR "beta-coronavirus" OR "beta-coronaviruses" OR "corona virus" OR "virus corona" OR "corono virus" OR "virus corono" OR hcov* OR covid* OR "2019-ncov" OR cv19* OR "cv-19" OR "cv 19" OR "n-cov" OR ncov* OR (wuhan* and (virus OR viruses OR viral)) OR sars* OR sari OR "severe acute respiratory syndrome" OR mers* OR "middle east respiratory syndrome" OR "middle-east respiratory syndrome" OR "2019-ncov-related" OR "cv-19-related" OR "n-cov-related" AND (remdesivir* OR "GS-5734" OR "GS 5734" OR GS5734*)
Other sources
In order to identify articles that might have been missed in the electronic searches, we proceeded as follows:
● Screened the reference lists of other systematic reviews.
● Scanned the reference lists of selected guidelines, narrative reviews, and other documents.
Eligibility criteria
We included randomized controlled trials evaluating patients infected with SARS-CoV-2 of any severity. The intervention of interest was remdesivir at any dosage, duration, timing or route of administration. The comparison of interest was a placebo (remdesivir plus standard of care versus placebo plus standard of care) or no treatment (remdesivir plus standard of care versus standard of care).
Our primary outcome of interest was all-cause mortality at longest follow-up. Secondary outcomes were invasive mechanical ventilation and adverse effects leading to discontinuation. We also extracted information on the following outcomes: time to viral clearance, length of hospital stay, and serious adverse effects.
We did not consider the outcomes as an inclusion criterion during the selection process. Any article meeting all the criteria except for the outcome criterion was preliminarily included and assessed in full text.
Selection of studies
The results of the searches in the individual sources were de-duplicated by an algorithm that compares unique identifiers (database ID, DOI, trial registry ID), and citation details (i.e. author names, journal, year of publication, volume, number, pages, article title, and article abstract). Then, the information matching the search strategy was sent in real-time to the classification tab in the L·OVE platform where at least two authors independently screened the titles and abstracts yielded against the inclusion criteria (Appendix 2). We obtained the full reports for all titles that appeared to meet the inclusion criteria or required further analysis and then decided about their inclusion.
We recorded the reasons for excluding trials in any stage of the search and outlined the study selection process in a PRISMA flow diagram that we adapted for the purpose of this project.
Extraction and management of data
Using standardized forms, two reviewers independently extracted the following data from each included trial: study design, setting, participant characteristics (including disease severity and age) and study eligibility criteria; details about the administered intervention and comparison, including dose, duration and timing (i.e. the time after diagnosis); the outcomes assessed and the time they were measured; the source of funding of the study and the conflicts of interest disclosed by the investigators; the risk of bias assessment for each individual study. We resolved disagreements by discussion, with one arbiter adjudicating unresolved disagreements.
Risk of bias assessment
The risk of bias for each randomized trial was assessed by using the 'risk of bias' tool (RoB 2.0: a revised tool to assess risk of bias in randomized trials)[19], considering the following domains of bias for each outcome result of all reported outcomes and time points: bias due to (1) the randomization process, (2) deviations from intended interventions (effects of assignment to interventions at baseline), (3) missing outcome data, (4) measurement of the outcome, and (5) selection of reported results.
Discrepancies between review authors were resolved by discussion to reach a consensus. If necessary, a third review author was consulted to achieve a decision.
Measures of treatment effect
For dichotomous outcomes, we expressed the estimate of the treatment effect of an intervention as risk ratios (RR) along with 95% confidence intervals (CI).
For continuous outcomes, we used the mean difference and standard deviation to summarize the data along with a 95% confidence interval. For continuous outcomes reported using different scales, the treatment effect was expressed as a standardized mean difference with 95% confidence interval.
Strategy for data synthesis
The results of the search and the selection of the studies is presented in the corresponding flow chart, according to recommendations of the PRISMA statement[14]. For any outcomes where it was not possible to calculate an effect estimate, a narrative synthesis is presented, describing the studies in terms of the direction and the size of effects, and any available measure of precision.
For any outcomes where data were available from more than one trial, we conducted a formal quantitative synthesis (meta-analysis) for studies clinically homogeneous using RevMan 5[20] and using the inverse variance method with the random-effects model. We assessed inconsistency by visual inspection of the forest plots and using the I² index.
Subgroup and sensitivity analysis
As few trials were found, we did not perform sensitivity or subgroup analysis.
Assessment of certainty of the evidence
The certainty of the evidence for all outcomes was judged using the Grading of Recommendations Assessment, Development and Evaluation working group methodology (GRADE Working Group)[21], across the domains of risk of bias, consistency, directness, precision and reporting bias. For the main comparisons and outcomes, we prepared a Summary of Findings (SoF) tables[22],[23].
Living evidence synthesis
An artificial intelligence algorithm deployed in the Coronavirus/COVID-19 topic of the L·OVE platform provides instant notification of articles with a high likelihood of being eligible. The authors review them, decide upon inclusion, and update the living web version of the review accordingly.
This review is part of a larger project set up to produce multiple parallel systematic reviews relevant to COVID-19[15].
Results
Results of the search
We conducted searches using L·OVE (Living OVerview of Evidence) platform for COVID-19, a system that maps PICO questions to a repository, maintained through regular searches in 27 databases, preprint servers, trial registries and websites relevant to COVID-19. All the searches covered the period until 25 August 2020. No date or language restrictions were applied.
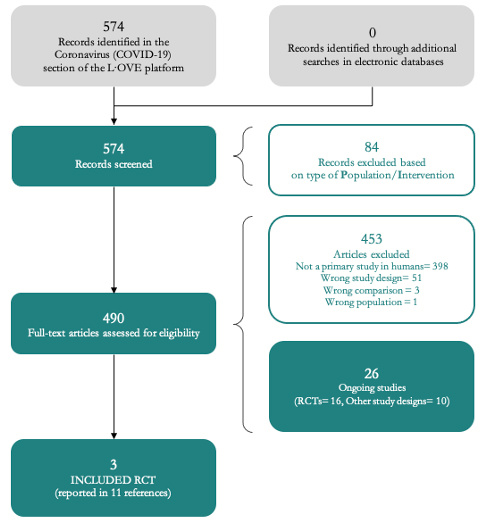
The search in the L·OVE platform yielded 574 records after removal of duplicates. We considered 489 as potentially eligible and obtained and evaluated their full texts. We finally included three randomized trials (11 references)[24],[25],[26].
The reasons for excluding studies at the time of full-text review were the following: not a primary study in humans (398 records); wrong study design (51 records), wrong comparison (three records) and wrong population (one record). We also identified 16 ongoing randomized trials.
The complete study selection process is summarized in the PRISMA flow chart (Figure 1) and the full list of included, excluded and ongoing trials is presented in Appendix 3.
 Full size
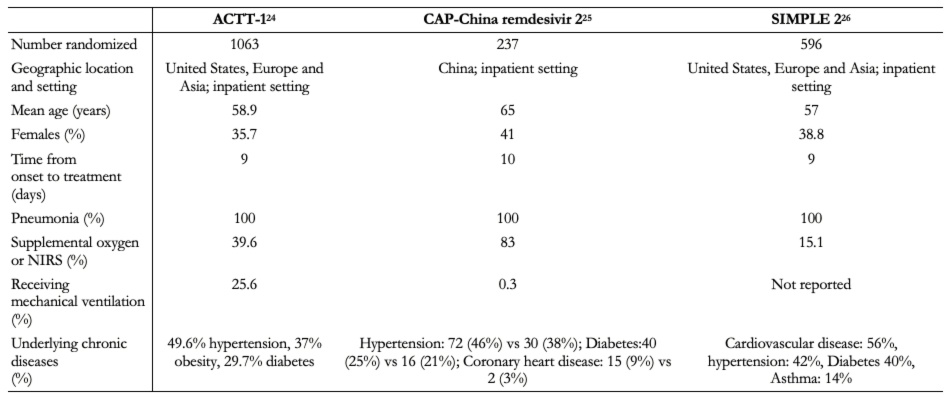
Full size Description of the included studies
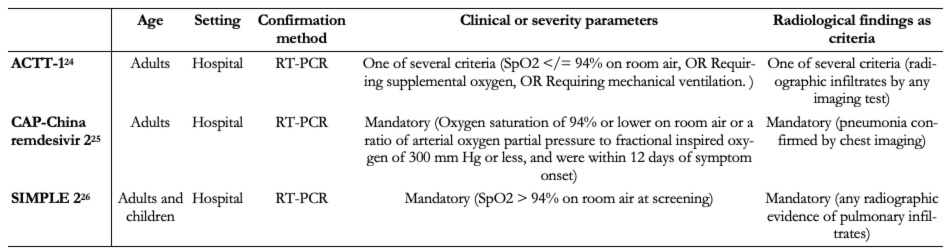
The three trials identified were the Adaptive COVID-19 Treatment Trial (ACTT-1[24]), the CAP-China remdesivir 2[25] and SIMPLE 2[26]. All trials evaluated inpatient adults. ACTT-1 required for inclusion that one of the following criteria were also fulfilled: SpO2 94% on room air. Tables 1 and 2 summarize the inclusion criteria of the trials and characteristics of the intervention. More details are presented in Appendix 3. Table 1 presents the complete inclusion criteria of the trials.
 Full size
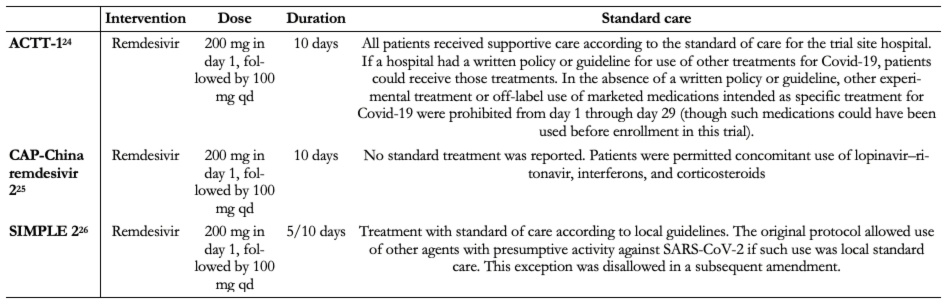
Full size All trials administered the same doses of remdesivir plus standard care[24],[25],[26]. One trial included two intervention arms of remdesivir (five-day and ten-day course of remdesivir)[26]. None of the trials provides further details regarding the standard care treatment delivered. Two trials reported that the standard of care was determined by the trial site hospital[24]. The other one only reported that concomitant use of lopinavir/ritonavir, interferons, and corticoids were permitted[25].
 Full size
Full size In total, trials included 1 896 hospitalized patients[24],[25],[26]. One trial was conducted in China[25], and the other two were multicenter trials conducted in several countries[24],[26]. All trials included patients with radiologically confirmed pneumonia[25],[26]. Baseline characteristics of participants regarding age, gender, and chronic disease were similar between studies, but the number of patients requiring supplemental oxygen or mechanical ventilation varied substantially between trials[24],[25].
 Full size
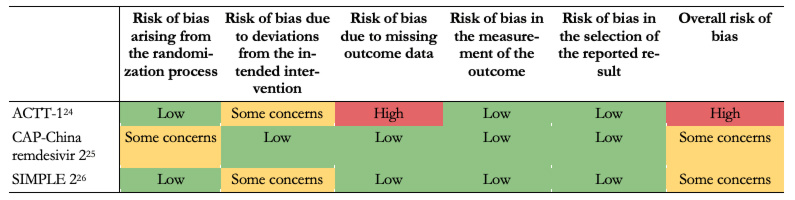
Full size Risk of bias in the included studies
We judge that the overall risk of bias was "high" for all outcomes regarding the ACTT-1 trial[24]. The study was judged to raise "some concerns'' in deviations from the intended intervention domain and "high" in bias due to missing outcome data. CAP-China remdesivir 2 trial overall risk of bias was "some concern" for all outcomes, because of problems in the randomization process[25]. SIMPLE 2 overall risk of bias was some concern for all outcomes due to deviations from intended interventions[26]. Table 4 summarizes the risk of bias assessments and details of each assessment are presented in Appendix 3.
 Full size
Full size Efficacy of remdesivir in the treatment of patients with COVID-19
The main results are summarized in the Summary of Findings table, presented at the beginning of the manuscript.
Primary outcome
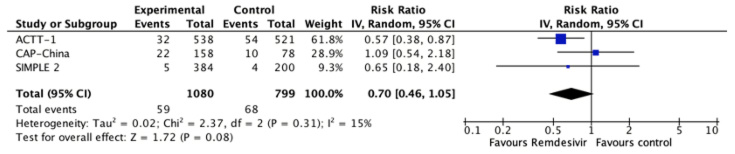
All-cause mortality
All studies reported this outcome[24],[25],[26] and the evidence is very uncertain about the effect of remdesivir on mortality (RR 0.7, 95% CI 0.46 to 1.05; very low certainty evidence).
 Full size
Full size Secondary outcomes
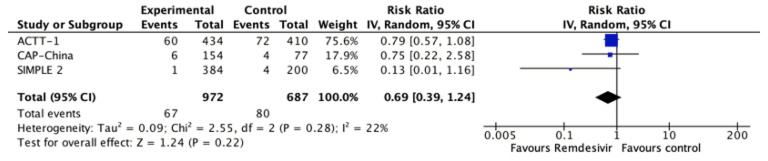
Invasive mechanical ventilation
All studies reported this outcome[24],[25],[26] and the evidence is very uncertain about the effect of remdesivir on the need for invasive mechanical ventilation (RR 0.69, 95% CI 0.39 to 1.24; very low certainty evidence).
 Full size
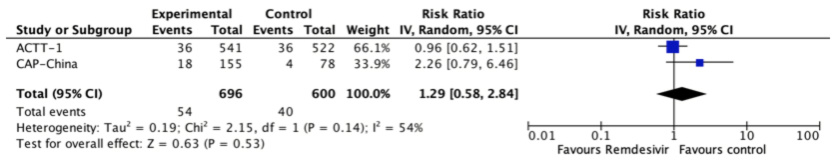
Full size Adverse effects leading to discontinuation
Two trials reported this outcome[24],[25] and remdesivir likely results in a large increase in the incidence of adverse effects (RR 1.29, 95% CI 0.58 to 2.84; moderate certainty evidence).
 Full size
Full size Time to viral clearance
This outcome was not measured or reported by the included studies.
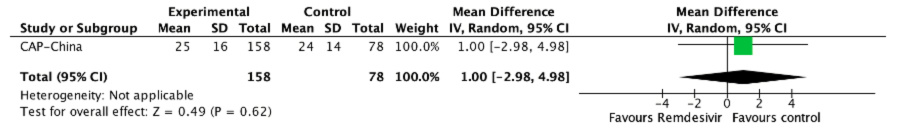
Length of hospital stay
Two studies reported this outcome[25],[26], but only one was usable for meta analysis[25]. SIMPLE 2 trial reported that there were no significant differences between the remdesivir and standard care groups in duration of hospitalization[25]. Quantitative synthesis showed that remdesivir might result in little to no difference in the duration of hospitalization (MD 1, 95% CI -2.86 to 4.86; low certainty evidence).
 Full size
Full size Other outcomes
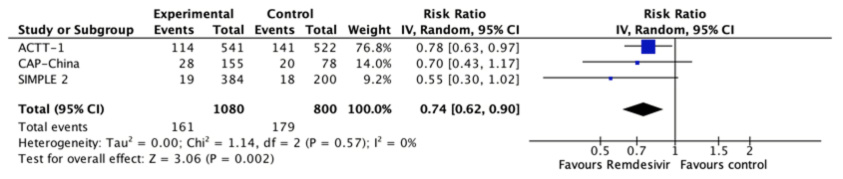
Serious adverse effects
All studies reported this outcome[24],[25],[26] and remdesivir likely
reduces the number of serious adverse effects (RR 0.74, 95% CI 0.62 to 0.9; moderate certainty evidence).
 Full size
Full size Discussion
We conducted a systematic review and identified three randomized trials that reported data on the effect of remdesivir in patients with COVID-19[24],[25],[26]. Even though remdesivir appears to be safe, the evidence is very uncertain about the impact on the outcomes critical for decision-making in moderate and severe patients—the more relevant clinical scenario for this drug, such as mortality and need of mechanical ventilation.
It is unfortunate not knowing yet if one of the pharmaceutical interventions that have sparked more interest is effective or not. One of the limitations comes from the lack of precision of the result for the main outcomes. The early termination of the ACTT-1 trial can be seen as a missed opportunity in this regard[25]. In addition, all the trials concluded enrollment before the release of the RECOVERY trial, which showed a mortality reduction with dexamethasone[27]. It is not clear if this factor would modify the effect, if any, of remdesivir.
By now, clinicians and other decision-makers are in a difficult position. The pressure to act is high, particularly after the US Food and Drug Administration issued an emergency use authorization of remdesivir for the treatment of COVID-19[12]. We anticipate that the range of recommendations from different organizations should range between a suggestion against its use and a weak recommendation for its use in severe cases, especially in settings without resource constraints.
There are at least 46 ongoing trials that we expect will provide data in the near future. Making sense of this information is not going to be an easy task. Systematic reviews are considered the gold standard to make sense of multiple trials addressing a similar scientific question, but the traditional model for conducting reviews has several limitations, including high demand for time and resources[28] and rapid obsolescence[29]. Amid the COVID-19 crisis, researchers should make their best effort to answer the urgent needs of health decision-makers without giving up scientific accuracy. Information is being produced at a vertiginous speed[30], so alternative models are needed.
One potential solution to these shortfalls is rapid reviews, a form of knowledge synthesis that streamlines or omits specific methods of a traditional systematic review in order to move faster. Unfortunately, in many cases, this speed comes at the cost of quality[31]. Furthermore, they do not solve the issue of obsolescence. Living systematic reviews do address that issue[32]. They are continually updated by incorporating relevant new evidence as it becomes available, at a substantial effort. So, an approach combining these two models might prove more successful in providing the scientific community and other interested parties with evidence that is actionable, rapidly and efficiently produced, up to date, and of the highest quality[33].
This review is part of a larger project set up to put such an approach into practice. The project aims to produce multiple parallel living systematic reviews relevant to COVID-19 following the higher standards of quality in evidence synthesis production[15]. We believe that our methods are well suited to handle the abundance of evidence that is to come, including evidence on the role of lopinavir/ritonavir for COVID-19.
During the COVID-19 pandemic, we will maintain the search and selection of evidence for this review continuously updated, as well as an update when conclusions change or whenever there are substantial updates. Our systematic review aims to provide a high-quality, up-to-date synthesis of the evidence that is useful for clinicians and other decision-makers.
Annexes

