Reporte de caso
← vista completaPublicado el 28 de agosto de 2024 | http://doi.org/10.5867/medwave.2024.07.2917
Diagnóstico tardío de tuberculosis diseminada: reporte de caso
Late diagnosis of disseminated tuberculosis: A case report
Abstract
Introduction The lungs are most commonly involved in tuberculosis, but infection can also involve other organs through lymphohematogenous dissemination. The clinical presentation of disseminated tuberculosis is variable. Diagnosis is difficult, because clinical manifestations are diverse, more than 50% of patients present late, because microbiological testing relies on invasive procedures for mycobacterial culture and supportive histopathology.
Case report A 30-year-old male patient, deprived of his liberty, with no co-morbidities, was admitted to the hospital for severe pain in the left wrist, with a previous history of having received systemic glucocorticoids for 7 months. He developed clinical symptoms of pulmonary tuberculosis, in the pleura, in the joint of the left wrist and in the left testicle, and tests confirmed the presence of M. tuberculosis. He underwent surgery on the wrist and testicle and was also treated for susceptible tuberculosis. Concomitant sequelae of iatrogenic Cushing’s disease, chronic anemia and chronic inactive proctitis were diagnosed.
Conclusions Diagnosis of disseminated tuberculosis was difficult due to the non-specific clinical picture, limitations of confirmatory diagnostic tools and timely specialized evaluations. Prolonged use of systemic corticosteroids may have played a role in the dissemination of tuberculosis.
Main messages
- Disseminated tuberculosis is a life-threatening condition, especially if diagnosis and treatment are delayed.
- Only 1 to 2% of tuberculosis cases are disseminated.
- Diagnosing disseminated tuberculosis is challenging, as adequately selected specimens for bacteriological and molecular testing are needed.
- We present a case report of disseminated tuberculosis, which may shed some light on the approach on patient managment.
- Early diagnosis of disseminated tuberculosis prevents death and disabling sequelae.
Introduction
The lungs are the most common site of infection in tuberculosis, accounting for almost 70% of cases. Infection can also involve other organs through lymphohaematogenous dissemination [1,2]. Extrapulmonary sites include lymph nodes, pleura, kidneys, spine, joints, brain, meninges, peritoneum, intestine, liver, testis, ovaries, fallopian tubes, eyes (choroid) and pericardium [2,3]. Predisposing factors for disseminated TB include elderly patients, people with human immunodeficiency virus infection, alcohol abuse, diabetes, chronic liver or kidney failure, organ transplantation, immunosuppressive drugs, prolonged corticosteroids, pregnancy, and symptomatic tuberculosis lasting more than 12 weeks [4,5,6]. Disseminated tuberculosis is a progressive and potentially fatal disease. Tuberculosis spreads through lymphohaematogenous dissemination of Mycobacterium tuberculosis bacillus from primary tuberculosis or progression of untreated primary tuberculosis [1,6]. Of all tuberculosis cases, only 1-2% are of the disseminated [7].
The clinical presentation of disseminated tuberculosis is variable. Symptoms include sub-acute or chronic constitutional symptoms such as fever, weight loss, and night sweats, but may present as multi-organ failure. The duration of symptoms and signs prior is variable, and more than 50% of patients seek medical help several months after the onset of symptoms [8,9,10,11,12].
Diagnosis remains challenging because clinical manifestations are diverse, and microbiological testing relies on invasive procedures for mycobacterial culture and supportive histopathology. In addition, these tests are not available in most healthcare facilities [13].
The present report aims to portray the importance of timely diagnosis of tuberculosis to prevent multi-organ involvement with severe sequelae or death.
Case report
Male, 30 years old, single. Person deprived of liberty (prisoner). He was admitted for emergency hospitalization to the traumatology department of the Hospital Regional Docente de Trujillo on 15 April 2023 for presenting intense pain and signs of phlogosis in the left wrist.
The patient reported that in April 2022, he presented with a sensation of heaviness and numbness in her left wrist. Within a few hours, pain began to set in, and pain increased with its volume. He did not receive any treatment. Approximately one month later, he was treated by prison medical staff with the hypothesis of deep venous insufficiency. On that occasion, he was administered enoxaparin subcutaneously every 12 hours for a month, showing a slight improvement. As the discomfort persisted, a wrist fracture was suspected.
For this reason, he was taken to the "bonesetter" (empirical person) to "set" the fracture, who immobilized him with splints and bandages. From that moment on, the increase in volume of the wrist joint began to become more noticeable, and the pain became more intense, adding deformity and functional limitation. In August 2022, he began to feel a "lump" in the perianal area, which he played down. He was diagnosed with an anorectal fistula of "undefined" infectious cause, as bacteriological tests were not performed. The approach was to perform a fistulectomy. In October 2022, he attended the prison infirmary, where he was initially administered once daily dexamethasone plus diclofenac sodium via intramuscular route. Due to persistent pain, the dose was increased to every 12 hours for three months. This was the only way to control the pain. The patient continued to self-medicate with dexamethasone and diclofenac tablets orally every 12 hours for four months, during which time he presented weight gain of 12 kilos and signs compatible with iatrogenic untreated Cushing’s syndrome.
In February 2023, he began to notice a progressive increase in the volume of his left testicle without receiving medical attention. At the beginning of March, he was diagnosed with pulmonary tuberculosis at the penitentiary establishment with a positive smear test. No chest X-ray examination was carried out.
On 8 March 2023, the first phase of treatment for tuberculosis with a sensitive schedule was started. For two months, he was given a daily dose of 300 milligrams of isoniazid, 600 milligrams of rifampicin, 1600 milligrams of ethambutol, and 1875 milligrams of pyrazinamide.
In mid-April, he was transferred from the prison to the outpatient trauma clinic of the Regional Teaching Hospital of Trujillo and immediately transferred to the emergency department for hospitalization.
On admission, he presented with normal vital functions and was in apparently fair general condition. Oxygen saturation (SaO2) was 97% room air. He had a height of 1.75 meters, a weight of 65 kilograms, and a body mass index (BMI) of 21.
On preferential examination, he had linear purplish striae in the subcutaneous cellular tissue on the forearms and thighs (Figure 1). The head, neck, thorax, and abdomen were unremarkable. In the genitourinary area, the left testicle showed signs of flogosis, as did the left wrist. The left wrist also showed deformity and pain on digit pressure, and a "soft collection" measuring four by 4 centimeters was palpated (Figure 2), with limitation of joint movements.
Subcutaneous striae, sequelae of iatrogenic Cushing’s disease.

Left wrist injury.

The initial presumptive diagnoses were fracture of the left ulna and distal radius, osteomyelitis of the left wrist, and pulmonary tuberculosis under treatment.
During his hospitalization in the traumatology department, he was evaluated by the pulmonology department, which indicated that he should continue treatment for tuberculosis. He was also evaluated by the urology department, which requested testicular, renal, bladder, and prostate ultrasound scans, as well as smear microscopy and urine culture for Mycobacterium tuberculosis. Ten days later, he was re-evaluated by the pneumology service, referring to joint problems in the left wrist and pain, plus increased volume in the left testicle.
At this point, the patient had a diagnostic presumption of disseminated tuberculosis consisting of pulmonary, joint, and testicular involvement. Consequently, it was indicated to continue with antituberculosis treatment and to request smear microscopy, smear culture, and rapid sensitivity tests (real-time polymerase chain reaction) of secretion from wrist lesions and urine. Re-evaluation by urology was suggested, in addition to urgent surgery of the left wrist joint.
On 4 May, the patient underwent trauma surgery. The procedure included drainage of the left wrist abscess and surgical cleaning. Liquefied viscoelastic tissue and distorted, highly vascularised bone tissue were reported with no foul odor or purulent discharge. In addition, samples were taken from the lesion for bacteriological studies. The pathology report of the bone biopsy concluded with chronic osteomyelitis. The results of the tissue sample from the left wrist smear were positive.
After re-evaluation by urology, acute orchiepididymitis was diagnosed, ruling out epididymal tuberculosis. Treatment indicated 500 milligrams of levofloxacin every 24 hours orally for seven days, 15 milligrams of meloxicam orally for seven days, scrotal suspension, and re-evaluation at the end of treatment.
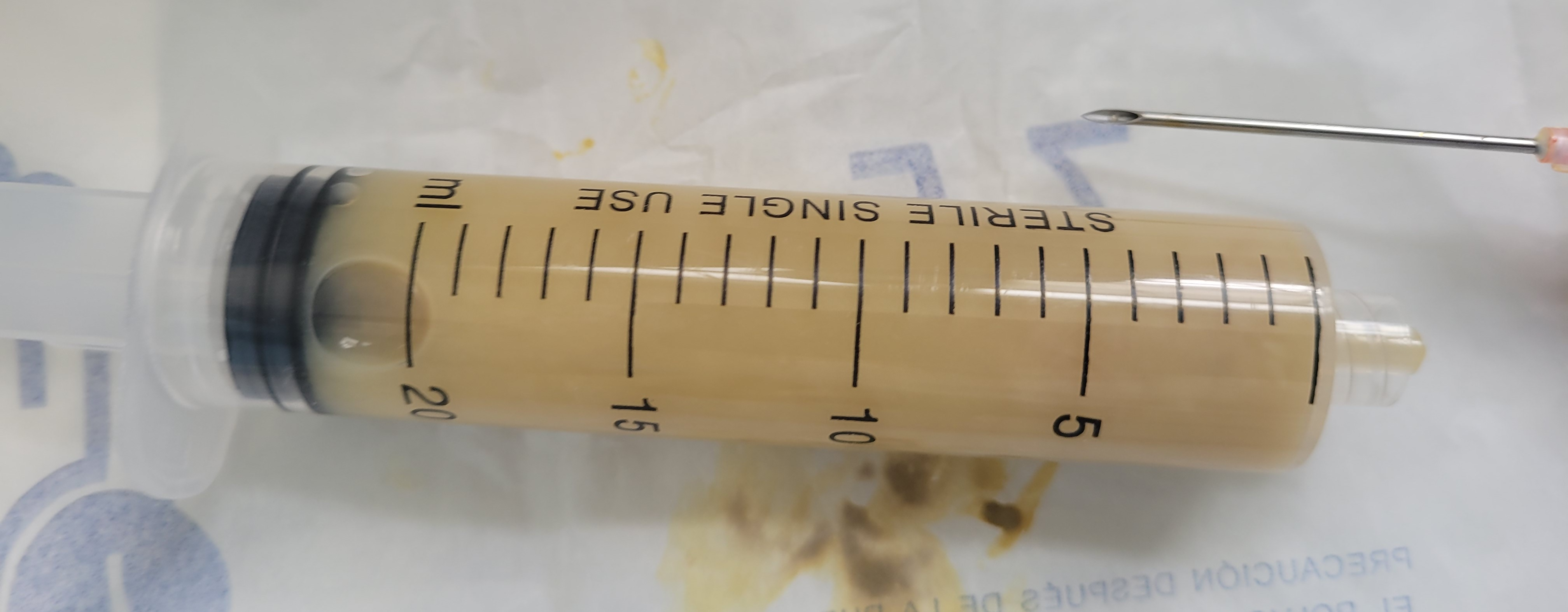
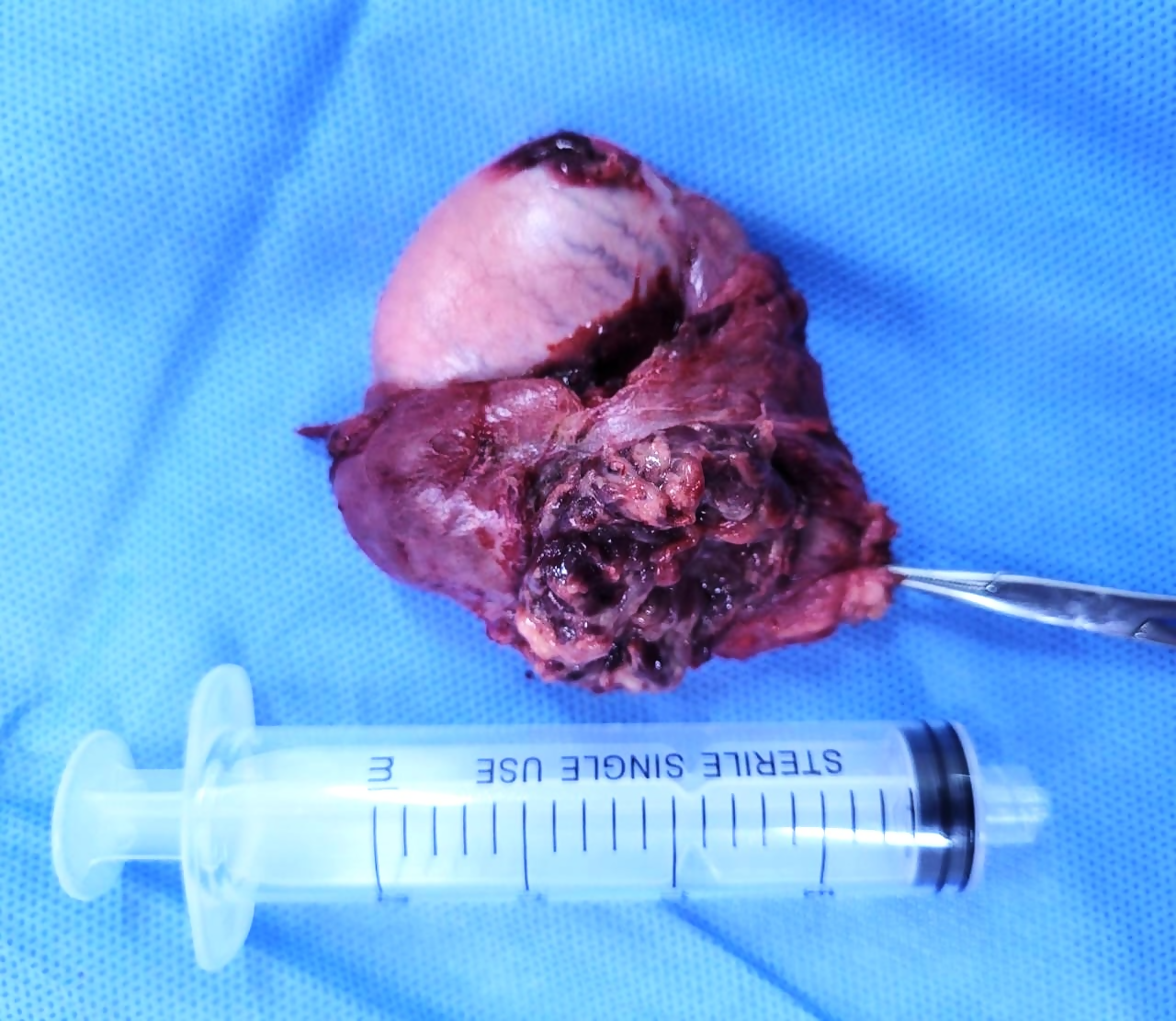
The urology department re-evaluated the case at the end of the indicated treatment, performing a puncture and aspiration of the left testicular abscess (Figure 3). The following day, the result of the secretion analysis showed a positive smear test. With the diagnosis of testicular tuberculosis, it was decided to perform a radical left orchidectomy (Figure 4). Tissue samples were sent for anatomical pathology and bacteriology studies. The anatomical pathology report concluded findings in the scrotum with chronic active inflammation, microabscesses, and non-caseating granulomas. In addition, areas of edema and interstitial vascular congestion were present in the testis.
Aspiration discharge from left testicular abscess.
Radical left orchidectomy.
The gastroenterology unit also performed proctosigmoidoscopy. This recorded findings of entero-cutaneous anorectal fistula. The biopsy report of the anal region concluded chronic inactive proctitis. The smear of secretion from the anorectal fistula was negative. The unit recommended symptomatic treatment and outpatient control.
The pneumology department indicated continuing the second phase of antituberculosis treatment with 300 milligrams of isoniazid and 600 milligrams of rifampicin, both administered daily for ten months. Finally, the scheme was structured in the first phase, which consisted of two months of isoniazid, rifampicin, ethambutol, and pyrazinamide daily. In the second phase, isoniazid and rifampicin for ten months, also daily (2HREZ /10HR), according to the Technical health standard for the comprehensive care of the person affected by tuberculosis, family and community 2023 [3].
With these findings, the patient was transferred to the infectious disease department for further treatment.
Other drugs the patient received were oxacillin at a dose of 2 grams intravenous every 6 hours for 21 days, 100 milligrams of intravenous ketoprofen every 12 hours for seven days, 100 milligrams of intravenous tramadol conditioned to the presence of pain once a day for one month.
At discharge, the patient was diagnosed with disseminated tuberculosis (pulmonary, bone, and testicular tuberculosis), with sequelae of iatrogenic Cushing’s disease and anorectal fistula, along with chronic inactive proctitis and mild chronic anemia.
Subsequently, in July 2023, he was checked by the infectious diseases department, which reported an improvement in the clinical picture of disseminated tuberculosis.
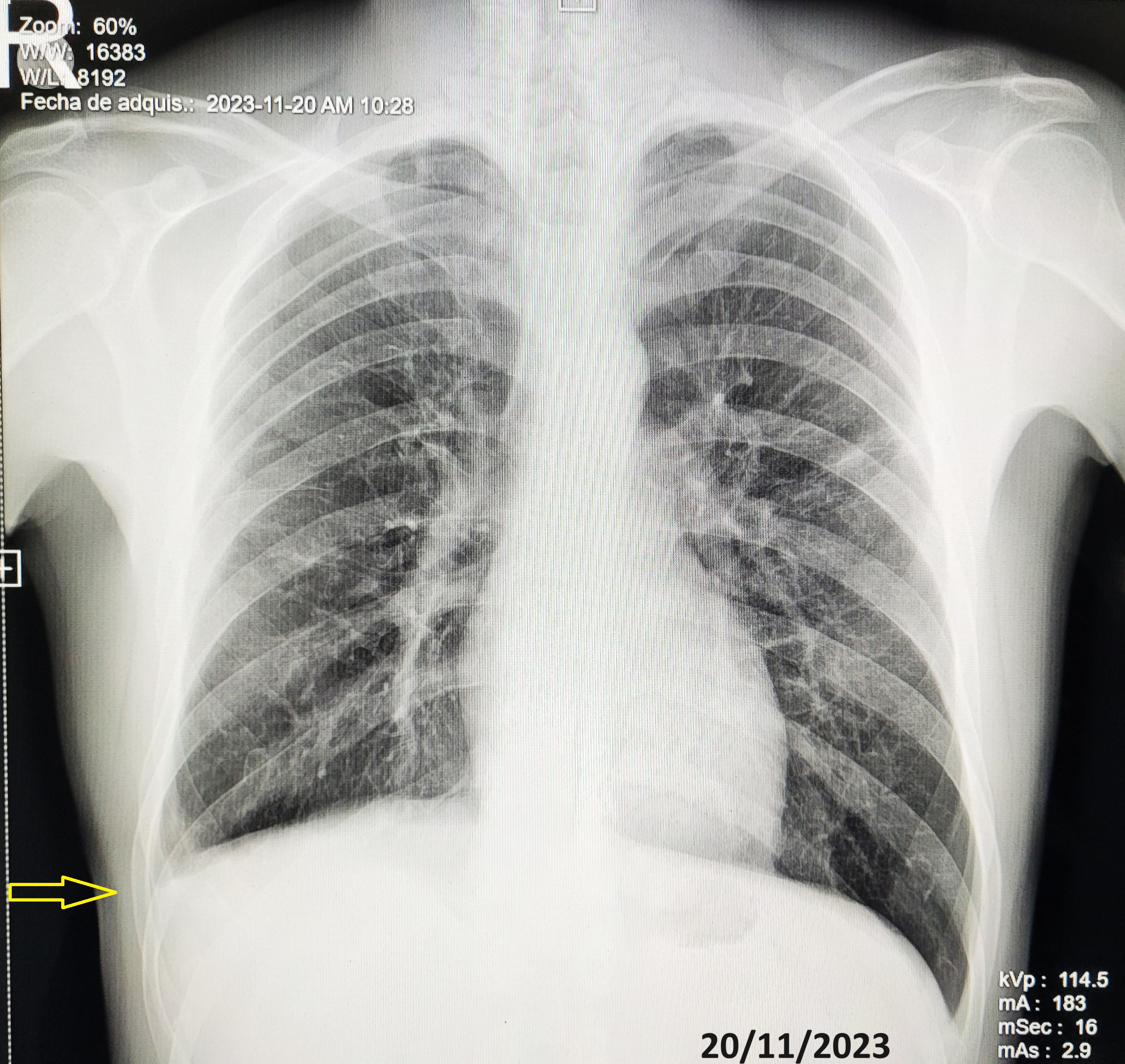
In November 2023, he was monitored by urology, traumatology, and pneumology. Urology reported the absence of the left testicle and the right testicle without alterations, with a good evolution. Traumatology, with the support of radiographic studies of the wrist, reported a good evolution of the tuberculous infection (Figure 5), indicating that it did not merit surgical intervention (arthrodesis), as there had been an ankylosis of the carpal joint (Figure 6). Nevertheless, they recommended avoiding excessive physical activity with the hand and wrist. For its part, pulmonology concluded that the patient adhered to the treatment did not present significant discomfort, and resulted in a good clinical, bacteriological, and radiological evolution. For these conclusions, the service relied on the results of the radiological study of the chest (Figure 7), the smear tests, and the negative sputum culture for acid-alcohol-resistant bacilli. Consequently, discharge was indicated upon completion of the antituberculosis treatment regimen.
Left wrist injury sequelae.

Sequelae of articular tuberculosis, absence of the carpus.

Pleural tuberculosis sequelae (pachypleuritis), right phrenic costophrenic angle obturation (arrow). No lesions in lung parenchyma.
The patient reported a significant improvement in his mood due to the remission of respiratory and testicular complaints, mainly because his self-care dependency was primarily resolved with the improvement of the left wrist injury. However, the patient stated that he was aware that he would be left with permanent functional limitations.
Table 1 summarises the main symptoms and signs, as well as the examination and treatments performed.
Discussion
Disseminated tuberculosis is the presence of two or more non-contiguous sites resulting from hematogenous dissemination of Mycobacterium tuberculosis. It occurs due to progressive primary infection or by reactivating a latent focus with subsequent dissemination [14]. It is rarely iatrogenic in origin [15]. Our clinical case fulfills these criteria to be considered disseminated tuberculosis since the presence of Mycobacterium tuberculosis was confirmed in the lungs, the wrist joint, and the testicle, in addition to the residual pachypleuritis secondary to pleural tuberculosis observed in the final radiological study. We could infer that the entero-cutaneous anorectal fistula was also caused by tuberculous infection, considering it is a frequent presentation [16,17]. This is despite the fact that the detection of Mycobacterium tuberculosis complex was not confirmed by specific tests, and only residual lesions were found due to previous surgical treatment.
Disseminated tuberculosis is a life-threatening condition, significantly if diagnosis and treatment are delayed [14,16]. The diagnosis was challenging in this case due to its non-specific clinical picture and the paucity of tools available to confirm the laboratory diagnosis. The low sensitivity of smear microscopy compounds is due to the time-consuming cultures and molecular tests unavailable in most facilities.
The subtle and non-specific clinical presentation of the present case, the limitation of confirmatory diagnostic tools, and the difficulty in getting out of prison for timely specialized evaluations would have led to this disorder of disseminated TB being underestimated.
The incidence of disseminated tuberculosis is not yet known precisely. However, among immunocompetent adults, it is estimated that this group accounts for less than 2% of all tuberculosis cases and up to 20% of all extrapulmonary tuberculosis cases [15]. Disseminated tuberculosis is a significant cause of morbidity and mortality in developing countries. It has become more frequent in different age groups due to several risk factors. These include human immunodeficiency virus infection, the use of biologic drugs, immunosuppressants and corticotherapy, alcoholism, chronic liver disease, chronic hemodialysis, diabetes mellitus, malignant neoplasms, and silicosis [14,15,16,17,18,19,20]. In our case, the patient was exposed to systemic glucocorticoids inappropriately (as an analgesic) and prolonged. This caused an alteration in his immune response and, consequently, would have favored the dissemination of Mycobacterium tuberculosis to different organs (pulmonary, pleural, bone, testicular, and ano-rectal).
The mechanism of Mycobacterium tuberculosis dissemination is not well understood [21]. One proposed mechanism is that tuberculous infection spreads through a pulmonary vein after eroding the alveolar epithelial cell layer [21,22]. When the bacteria reach the left side of the heart and enter the circulatory system, they multiply and infect extrapulmonary organs, causing disseminated systemic tuberculosis. Also, mycobacteria can damage the cells lining the alveoli and enter the lymph nodes. From there, it enters the systemic venous blood and circulates back to the lung through the right side of the heart, producing disseminated pulmonary tuberculosis with a miliary appearance [21,22]. The two forms of dissemination can occur independently or together.
Dissemination of tuberculosis rarely occurs as an iatrogenic infection. A few cases have been published describing tuberculosis dissemination following surgical intervention [15,23,24,25,26,27]. A non-health professional ("bonesetter") ’s empirical manipulation of the wrist joint could be considered an initial or primary iatrogenic infection. This is because he presented with non-specific symptoms and signs in the left wrist long before the clinical presentation of tuberculosis in the lungs and testis.
Histological examination revealed microscopically tuberculous granulomas with or without central caseification. Sometimes, alcohol-resistant bacilli can be found within macrophages or in areas of caseification [17,28]. These findings are consistent with those described in the reports of the anatomy-pathology studies performed on our patient.
Acid-fast smears, real-time polymerase chain reaction, mycobacterial culture, and histology are needed to confirm the diagnosis in patients with suspected disseminated tuberculosis [14]. Nucleic acid amplification testing by real-time polymerase chain reaction has been used as a rapid diagnostic tool for tuberculosis, as it detects Mycobacterium tuberculosis complex directly from patient samples in only two hours [29]. Therefore, all samples from our patient, both secretions and tissue, obtained by biopsy and surgical excision, were sent to the mycobacteria laboratory. These samples were used for smear microscopy, culture for mycobacterium tuberculosis, and molecular biology testing (real-time polymerase chain reaction for tuberculosis). Positive results were obtained, proving the presence of the bacillus Mycobacterium tuberculosis.
Other rapid and non-invasive tests have also been used on samples other than sputum. This is because measuring biomarkers such as adenosine deaminase and interferon ɣ is inconclusive in cases of extrapulmonary tuberculosis despite its validating and confirmatory role [30,31,32,33,34,35].
Histopathology remains an essential method for diagnosing tuberculosis [3,36]. It is the diagnostic tool that we have also used in the study of wrist joint and testicular lesions, the results of which contributed to the diagnosis of disseminated tuberculosis.
Conclusions
The diagnosis of disseminated tuberculosis was difficult due to the non-specific clinical picture. To confirm the occult diagnosis of extrapulmonary presentation, molecular testing, and histology were necessary.
Prolonged use of systemic corticosteroids would have influenced the dissemination of tuberculosis.
The limitation of confirmatory diagnostic tools and specialized evaluations promptly resulted in underestimating the involvement of various organs in tuberculosis.

