Resúmenes Epistemonikos
← vista completaPublicado el 27 de diciembre de 2016 | http://doi.org/10.5867/medwave.2016.6819
¿Es efectivo y seguro el betabloqueo perioperatorio en pacientes sometidos a cirugía no cardíaca?
Is perioperative beta-blockade effective and safe in patients undergoing noncardiac surgery?
Abstract
Beta-blockade in patients undergoing noncardiac surgery has been widely recommended as a way to reduce cardiovascular adverse events during the perioperative period. However, studies have shown contradictory results. Searching in Epistemonikos database, which is maintained by screening multiple databases, we identified 22 systematic reviews comprising 131 studies addressing the question of this article, including 112 randomized trials. We combined the evidence using meta-analysis and generated a summary of findings following the GRADE approach. We concluded perioperative use of beta-blockers in patients undergoing noncardiac surgery, although probably decreases the risk of myocardial infarction, increases the risk of stroke and total mortality.
Problem
The increase of catecholamines that occurs during noncardiac surgery [1] causes an elevation of blood pressure and heart rate [2],[3],[4], which contributes to the occurrence of cardiovascular adverse events. Beta-blockers suppress the effect of the rise of catecholamines, thus it is thought its administration during perioperative period could prevent these events. Initial studies showed very promising results, which led this intervention to be widely recommended for a wide range of patients undergoing noncardiac surgery. However, further trials not only cast doubts about the benefits of administering beta-blockers during the perioperative period, but also warned of possible adverse effects such as stroke, hypotension and bradycardia, among others. Furthermore, some trials on which previous recommendations were based, have been questioned due to scientific misconduct of their authors. For all these reasons, the decision whether or not to use this intervention is debated up to this day.
Methods
We used Epistemonikos database, which is maintained by screening multiple databases, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found 22 systematic reviews [5],[6],[7],[8],[9],[10], |
|
What types of patients were included |
The 55 trials included adult patients undergoing any type of noncardiac surgery: gastrointestinal (22%), vascular (22%), gynecological (14.6%), chest (12.2%), trauma (7.3 %), neurological (7.3%), ENT (4.9%), maxillofacial (4.9%), oral (2.4%) and emergency surgery (2.4%). |
|
What types of interventions were included |
The type of beta-blocker most commonly used was metoprolol (35.1%), then esmolol (24.1%), atenolol (16.9%), labetalol (7.4%), bisoprolol (7.4%), propranolol (3.7%) and others (landiolol, nadolol and timolol, 5.4%). |
|
What types of outcomes |
The systematic reviews identified grouped outcomes as follows:
Postoperative follow-up of patients in different trials varied from the day of hospital discharge until 30 days after surgery. |
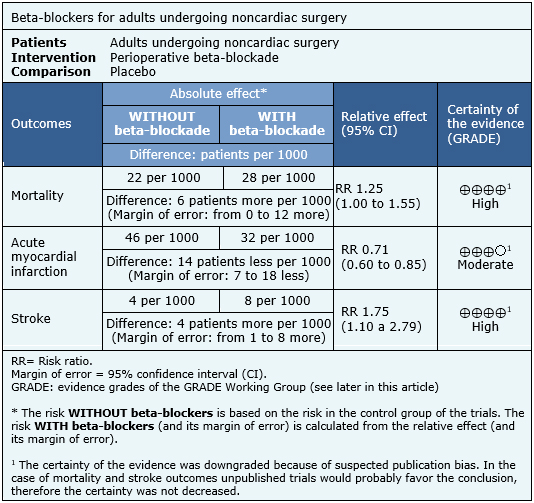
Summary of findings
The information on the effect of beta-blockers is based on the 29 randomized trials involving 12,644 patients, whose data could be included in a meta-analysis. All of the trials reported mortality [27],[28],[29],[31],[32],[33],[34],[36],[37],[38],[39], [40],[41],[42],[45],[46],[47],[52],[54],[56],[58],[59],[60],[62],[72],[74],[75],[77],[78], 26 trials reported perioperative myocardial infarction [27],[28],[29],[31],[33],[34],[39],[40],[41],[42],[45],[46],[47],[52],[54],[56],[58],[59],[60],[62],[63],[72],[74],[75],[77],[78] and 16 perioperative stroke [27],[28],[29],[40],[41],[42],[47],[56],[58],[59],[62],[72],[74],[75],[77],[78].The summary of findings is the following:
- Perioperative use of beta-blockers in patients undergoing noncardiac surgery increases mortality. The certainty of the evidence is high.
- Perioperative use of beta-blockers in patients undergoing noncardiac surgery probably decreases the risk of myocardial infarction. The certainty of the evidence is moderate.
- Perioperative use of beta-blockers in patients undergoing noncardiac surgery increases the risk of stroke. The certainty of the evidence is high.

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
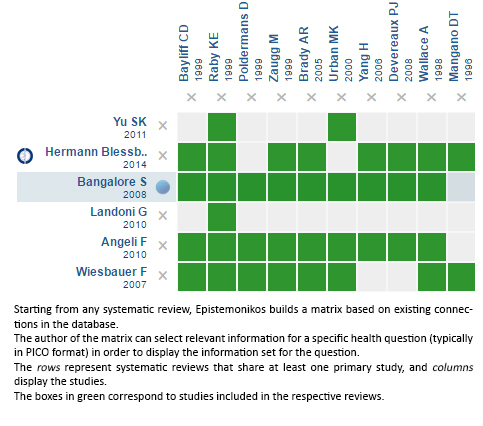
Follow the link to access the interactive version: Perioperative beta-blockers for noncardiac surgery
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.

