Research papers
← vista completaPublished on September 25, 2023 | http://doi.org/10.5867/medwave.2023.08.2709
Prevalence and factors associated with cervical cancer preventive screening in a Peruvian region
Prevalencia y factores asociados al tamizaje preventivo del cáncer cervical en una región de Perú
Abstract
Introduction Preventive screening for cervical cancer is the best available strategy to reduce the incidence and mortality from this neoplasm. However, the low proportion of women who undergo routine screening is a pending concern for healthcare systems worldwide.
Objective To estimate the prevalence and factors associated with preventive cervical cancer screening in a Peruvian region.
Methods Cross-sectional, multicenter study. It enrolled 1146 women users of healthcare centers in a Peruvian sanitary region. The dependent variable was the performance of cervical cancer preventive screening with Papanicolaou or visual inspection with acetic acid in the last two years. The independent variables were sociodemographic and socio-sanitary factors, knowledge about cervical cancer and human papillomavirus, attitudes and information towards screening tests. To evaluate the association between the variables, crude and adjusted prevalence ratios were calculated with generalized linear models of Poisson.
Results The overall prevalence of preventive screening was 50.5%. This was associated with being tested, having a higher education level and urban area of residence, using contraceptive methods, having health insurance, being recommended by healthcare personnel to be screened, and being concerned about developing cervical cancer. It was also associated with responding that this cancer is preventable, being aware of cervical cancer or human papillomavirus, and believing it can cause cervical cancer. In contrast, considering preventive screening risky was associated with not having the test.
Conclusions The proportion of women with preventive cervical cancer screening is low. In addition, certain associated modifiable factors were identified, which could improve preventive screening behaviors and rates.
Main messages
- Cervical cancer screening programs are being developed in Peru but do not yet show satisfactory results.
- This work proposes notions that will allow for more specific future studies in this area and seeks to contribute indirectly to increasing regional screening rates.
- Among others, the limitations of this study are the research design that did not allow for establishing causal relationships, the possible underestimation of results due to the possibility of bias due to self-reporting of variables, and the sample size and location, which may not be representative of the Peruvian national population.
Introduction
Cervical cancer is an ongoing public health concern worldwide. Although preventable, by 2020, it is the fourth cancer with the highest incidence in women globally and the ninth cancer with the highest mortality [1].
In Peru, 4270 new cases of this neoplasm were reported in 2022, and it is the fourth country with the highest mortality rate in South America [2,3]. At the same time, 2288 deaths were reported, representing 12.3% of deaths due to cancer in women nationwide [2,4]. Although Cervical smears in the country are considered an important, cost-effective intervention to detect cases of cervical cancer promptly, this neoplasm leads to cancer incidence in 2022 with 27% of the total number of cases [5]. The Peruvian Medical Association warns of increased cervical cancer [2]. This situation leads to the conclusion that the impact of cervical cancer screening is insufficient in developing countries [6].
The World Health Organization (WHO) recommends performing the cervical smear test and visual inspection with acetic acid as preventive screening tools for cervical cancer [7]. On the other hand, Peru, with a population of approximately 33 726 000 inhabitants, has a segmented and fragmented healthcare system consisting of public and private subsystems, where the largest public provider is the Ministry of Health. For this reason, the "Health Directive for the prevention of cervical cancer through early detection and treatment of premalignant lesions, including carcinoma in situ" recommends cervical smears every two years for women between 25 and 64 years of age and, as a complementary measure to increase coverage, visual inspection with acetic acid for women between 30 and 49 years of age. In addition, it suggests using molecular tests to detect human papillomavirus, the goal being to achieve preventive screening rates greater than or equal to 85% [8]. Although the healthcare directive is oriented to all subsystems, the study prioritized users of the public system under the Ministry of Health, as it is the main provider and the one with the widest population coverage in Peru.
Cervical cancer screening is key for preventing, detecting, and treating this neoplasm [8]. Early diagnosis could prevent 40% of cancer cases, especially in women not vaccinated against human papillomavirus [9]. However, the high proportion of diagnoses in advanced stages reflects the low success of the cervical cancer prevention and control action plan. This situation is common in developing countries, where cytology-based screening programs are less likely to be successful [10]. This is due to the persistence of fragmented healthcare systems that lack adequate resources and infrastructure [11,12].
The screening process has been linked to sociodemographic and socio-sanitary factors and the woman’s information and attitude towards the tests [13]. These factors may contribute to late diagnosis and high mortality rates.
Although routine Cervical smears have reduced mortality by 70 to 80% in all countries and by approximately 90% in developing countries, eradicating this cancer depends on its early identification and eliminating barriers to its timely detection [14]. These interventions have unique opportunities in healthcare settings since this level of attention enables a comprehensive approach to meeting health needs [15].
The proportion of women in the country who undergo preventive cervical cancer screening is poorly documented. Likewise, sociodemographic, socio-sanitary, and information and attitudinal factors could influence the decision to be screened for this type of cancer [6,13,14]. For this reason, estimating the proportion of women who have undergone preventive cervical cancer screening and evaluating associated sociodemographic, socio-sanitary, information, and attitudinal factors in Peruvian regions is necessary.
Methods
Study design and participants
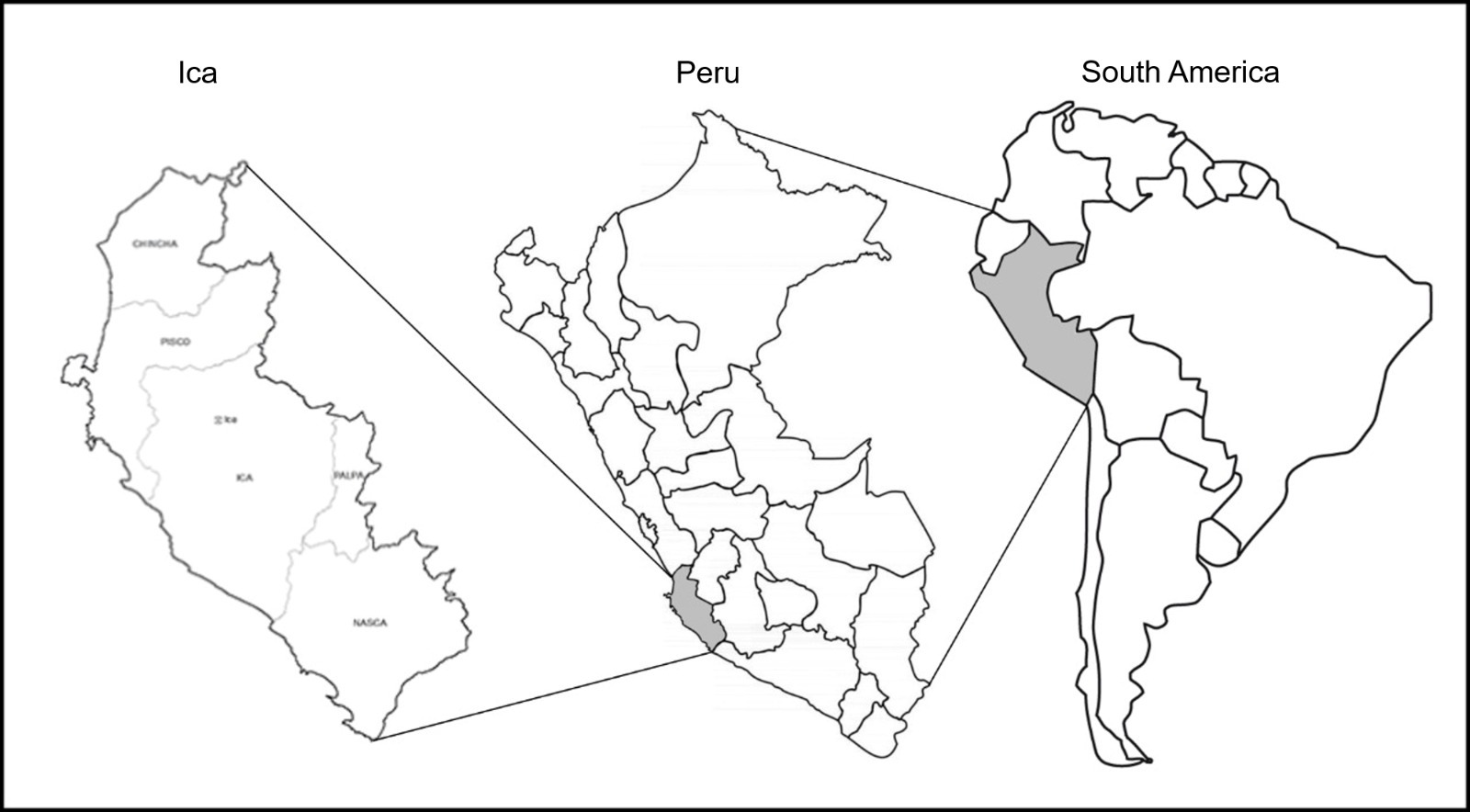
Quantitative cross-sectional study, conducted from August to December 2022. The population was delimited over a period of time, represented by female users aged 25 to 64 years who attended healthcare centers during the second semester of 2021 (more than 10 000 women) in the Ica Regional Health District. This district comprises five Peruvian provinces (Figure 1), covers an area of 21 328 square kilometers (1.7% of the Peruvian territory), with approximately 3.05% of the general population, and is considered the least poor of the Peruvian regions.
Geographic location of the Ica Region on the coast of Peru.
Study variables and instruments
A stratified and systematic probability sampling was carried out, which included two stages. It started with the mathematical formula of sample size for a proportion in an infinite or unknown population [16], a confidence level of 95%, precision of 3%, and an expected proportion of 50%, taking into account previous reports [8] and 7.4% expected loss. For this purpose, 1146 participants were estimated. Then, 12 of the 52 healthcare centers (representing the strata) were selected by random sampling, and a proportional sample was assigned to each one based on their attending population. The women users in each stratum were selected by systematic sampling. For this purpose, a skip interval k=N/n was defined (k: skip interval; N: population served; n: sample assigned). A random number between one and k was then chosen, which was used to begin selecting each of the women at the time of their admission to the healthcare center. Women were included if they met at least one of the following conditions: being 25 to 64 years old, pregnant [8], and agreeing to participate in the study. Women were excluded if they reported not having initiated sexual intercourse, having undergone total hysterectomy not associated with cervical cancer, having cervical cancer, and those who reported using other screening methods.
A questionnaire constructed by literature review was used, corresponding to the initial qualitative phase in the design and validation of the data collection instrument. This phase consisted of reviewing the literature and other instruments to select, modify, or translate questions from other languages and incorporate them into the questionnaire under construction. This proposal was presented to a team of five expert judges: two gynecologists and two obstetricians, all with doctoral degrees in public health, plus an expert in the design and validation of documentary instruments. All of them carried out the content validation of the instrument according to the criteria of relevance, sufficiency, pertinence, and clarity. This process made it possible to incorporate two variables or factors and improve the wording of some questions.
The dependent variable was the performance of preventive cervical cancer screening by cervical smear or visual inspection with acetic acid in the last two years [8]. The questions: "Have you ever had a cervical smear or visual inspection with acetic acid by an obstetrician or other healthcare professional in your life?" and "When was the last time you had a Cervical smear or visual inspection with acetic acid?" were used to determine who had undergone cervical cancer preventive screening in the last two years, assigning the variable "yes/no" categories.
Independent variables
We included age; number of children (none, 1, 2, 2, 3 or more), recategorized with/without children; pregnancy history (none, 1, 2, 3 or more), dichotomized with/without pregnancy; age of sexual debut, categorized as 12 to 17 (adolescent), 18 to 29 (youth) and 30 or more (adult); educational level (none/primary/secondary/secondary/higher), marital status (married/cohabiting, separated/divorced, single); region of origin (coast/sierra/rainforest) and area of residence (urban/rural).
Use of contraceptive method (yes/no); health insurance (Peruvian Social Health Insurance, EsSalud/Integral Health Insurance-SIS/Armed and Police Forces Health/Providing entity and private insurance/none), recategorized (with/without health insurance); received a recommendation from an obstetrician or other professional to be screened (yes/no); has any gynecological disease (yes/no); has family member/friend with cervical cancer (yes/no); feels worried about getting cervical cancer (very worried/somewhat worried/not very worried/not worried/not worried at all), recategorized considering the last two alternatives as "not worried" and the first two as "worried"
Cervical cancer awareness
Knowledge about cervical cancer and human papillomavirus was measured by four questions [17]:
-
Is it possible to prevent cancer?
-
Have you ever heard about cervical cancer?
If respondents answered yes to question "b", they were asked:
-
Have you ever heard of the human papillomavirus?
-
Do you think that HPV can cause cervical cancer?
Attitudes and awareness of cervical cancer and screening with cervical smears or visual inspection with acetic acid
To assess the level of information on cervical cancer awareness and screening using cervical smears or visual inspection with acetic acid, we asked: "Do you consider it necessary to have preventive screening, even if you feel well?" (yes/no); "Is it risky to have screening?" (yes/no); "Can early detection cure cervical cancer?" (yes, it can be cured/there is a high chance/there is a low chance/there is no chance of cure), the last two alternatives were recategorized as "no chance" and the first two as "yes"; "what is the probability of developing cervical cancer, regarding women your age?" (greater/equal or lesser probability of developing cervical cancer); "would you avoid preventive screening, for fear of being diagnosed?" (yes/no) "Do you consider screening tests uncomfortable?" (yes/no).
Application procedure
A pilot test was carried out to verify the functioning of the fieldwork. This test was carried out for processing reasons, demonstrating the absence of difficulties or limitations before applying the survey to the selected sample. The women users were recruited when they entered the healthcare centers.
In order to guarantee the quality of form filling, twelve surveyors with academic backgrounds in health sciences were duly trained. To be included in the study, the participant’s eligibility criteria were confirmed, and the purpose of the study and its procedures were explained to each participant. Informed consent was obtained, and the hetero-administered survey was carried out, ensuring privacy at all times.
Statistical analysis
A descriptive statistical analysis was applied with measures of absolute and relative frequencies for qualitative variables. Standard deviations, mean, median, and mode were also applied for quantitative variables. Hypothesis testing was also performed. For this purpose, differences in the distribution of variable proportions were evaluated with the Chi-square of homogeneity. Subsequently, Poisson generalized linear family models with logarithmic link function were used to avoid convergence problems and robust variance, to evaluate the association between the dependent variable with sociodemographic factors, socio-sanitary factors, cervical cancer and human papillomavirus awareness, and attitudes and information (previously dichotomized). In addition, four adjusted generalized linear models were used, a different one for each group of factors. An analysis of compliance with assumptions was included to ensure adequate interpretability. Crude and adjusted prevalence ratios with their 95% confidence intervals were calculated. All variables that met the following criteria were taken for adjustment: p < 0.05 in the crude model, the criterion of clinical interest and availability. Only the grouped age variable was excluded in the adjusted model, as it was considered that it did not meet these criteria. The Statistical Package for the Social Sciences for Windows version 25.0 in Spanish was used for data processing. A value of p < 0.05 was accepted as statistical significance. No confounding or interaction variables were identified during the statistical analysis. The Poisson distribution for the four regression models revealed the case of overdispersion.
Ethical aspects
The study was approved by the Ethics Committee of the Universidad Autónoma de Ica (CO-001-27-2022/CE). Consent to participate in the research was requested, and the women users were informed that their participation was voluntary and anonymous.
Results
A total of 1218 women participated in the survey (94.1% response rate). We excluded 48 cases of women who reported not having initiated sexual relations, 16 women who had undergone total hysterectomy not associated with cervical cancer, five reported having cervical cancer, and two cases who used other screening methods. The final sample consisted of 1146 participants, of whom 35.4% reported never having had a smear test or visual inspection with acetic acid. For the question "When did you last have a Cervical smear or visual inspection with acetic acid?", the mean was 2.32 years (SD: 1.49), median 2.0, and mode 1.0.
Within the sociodemographic factors, higher proportions of women were found to be married/cohabiting (72.3%) and came from the coastal region (79.3%). Regarding socio-sanitary factors, most reported not having a gynecological disease (91.8%) and not having a family member/friend with cervical cancer (82.2%). As for knowledge, the majority responded that it is possible to prevent cancer (92.9%) and that they had heard of cervical cancer (92.9%). As for attitudes and information about preventive screening, women consider it necessary to be screened, even if they feel well (89.9%), and that it is not risky to be screened (91.8%) (Table 1).
The prevalence of having undergone preventive screening was 50.5%. Regarding sociodemographic factors (Table 2), women with higher education (55.2%) and residents of urban areas (58.6%) showed higher screening rates. The hypothesis test shows that the number of children, pregnancies, educational level, marital status, and residential area showed significant differences (p-value < 0.05) between the study groups. In the bivariate regression analysis, a significantly higher prevalence ratio for screening was found in women with children and those who were pregnant. In the multiple regression analysis, a higher education level (adjusted prevalence ratio: 1.17: 95% CI: 1.04 to 1.32) and urban residence (adjusted prevalence ratio: 1.27: 95% CI: 1.10 to 1.47) were associated with being screened.
Regarding the socio-sanitary factors (Table 3), the highest proportion of preventive screening was found in women who used contraceptive methods (58.6%) and who received a recommendation from healthcare personnel to be screened (65.6%). The hypothesis test is shown, where the variables contraceptive method use, health insurance, received a recommendation from healthcare personnel to be screened, and concern about acquiring cervical cancer show significant differences (p-value < 0.05) in each study group. In the bivariate regression analysis, a significantly higher prevalence ratio for screening was found in the group that received a recommendation. The following were associated with being screened: using contraceptive methods (adjusted prevalence ratio: 1.28; 95% CI: 1.16 to 1.41), having health insurance (adjusted prevalence ratio: 1.31; 95% CI: 1.07 to 1.60), having received a screening recommendation (adjusted prevalence ratio: 4.80; 95% CI: 3.63 to 6.35), and being concerned about acquiring cervical cancer (adjusted prevalence ratio: 1.20; 95% CI: 1.06 to 1.36).
The association between cervical cancer awareness (Table 4) and a higher prevalence of preventive screening was found in those who responded that they had heard of cervical cancer (52.8%) and human papillomavirus (56.9%). The hypothesis test is shown, where the four variables referred to awareness show significant differences (p-value < 0.05) in each study group. In the bivariate regression analysis, a significantly higher prevalence ratio for screening was found in the group of women who had heard of the human papillomavirus. The following were linked to being screened: considering that it is possible to prevent cancer (adjusted prevalence ratio: 1.47; 95% CI: 1.03 to 2.12); having heard of cervical cancer (adjusted prevalence ratio: 2.18; 95% CI: 1.38 to 3.44): 1.38 to 3.44), human papillomavirus (adjusted prevalence ratio: 2.90; 95% CI: 2.15 to 3.91), and believing that human papillomavirus can cause cervical cancer (adjusted prevalence ratio: 1.09; 95% CI: 0.94 to 1.28).
In relation to attitudes and information regarding screening (Table 5), the majority of women who reported having undergone screening were those who did not consider these tests risky (52.9%) and those who thought that there was a possibility of curing cervical cancer with early detection (55.9%). The hypothesis test shows that five of the six variables referring to attitudes and information showed significant differences (p-value < 0.05) in each study group. In the bivariate regression analysis, a significantly higher prevalence ratio for screening was found in the group of women who recognized the possibility of curing cancer. Being screened was associated with considering that there is a possibility of curing cervical cancer with early detection (adjusted prevalence ratio: 1.90; 95% CI: 1.49 to 2.42) and thinking that being screened is risky was associated with not being tested (adjusted prevalence ratio: 0.52; 95% CI: 0.36 to 0.76).
Discussion
The findings confirm that five out of ten women have been screened for cervical cancer in the last two years (50.5%). In the 30 to 49 years of age group, visual inspection with acetic acid as an alternative screening test is very scarce. This is probably due to the lack of supplies or equipment, as in another coastal region of Peru [18]. However, it is mentioned that this strategy would not be the most recommended due to its limitations [6]. Nevertheless, the use of this method is not widespread, and it is expected that the practice of visual inspection with acetic acid will gradually increase in the Peruvian population.
Previous studies reveal that at least 50% of women in Peru have undergone a cervical smear in the last three years, which is lower in the highlands, jungle, and rural areas [18,19]. On the other hand, a recent Peruvian study reports that 52.4% of women had a cervical smear test in the last two years [17], results that are consistent with this study. However, this is not in accordance with an investigation that analyzed the 2019 Demographic and Family Health Survey [20] in Peru, which found that 67.6% of women were screened for cervical cancer at some point [20]. This can be explained by the fact that in the latter study, the age range started from the age of 12 years. As can be seen, the panorama of cervical cancer screening in the country presents variations and limitations regarding coverage and availability of resources. This reveals the need to improve strategies to optimize access and screening processes [17]. Considering these screening coverage figures (50% versus 52.4%) in the last three and two years, respectively, the variation is not substantial, and these low coverages would be linked to a higher incidence of cancer, as reported by the Peruvian Medical Association [2]. In this order, recent research reports low coverage or prevalence of preventive screening in various parts of the world [21,22,23,24,25,26,27,28].
Sociodemographic factors such as higher education (55.2%) and urban area of residence (58.6%) were associated with a higher proportion of screening compared to women without higher education (30%), primary (34.2%) and secondary (52.5%) respectively, together with rural residence (41.7%). The urban area of residence is the factor with the greatest impact due to its higher adjusted prevalence ratio. Research has shown that women with higher education, married, separated, and residing in an urban area are more likely to undergo screening [21]. These studies also show that higher education level was a significant predictor of screening acceptance [22], as observed in our study.
Socio-sanitary factors such as using contraceptive methods (58.6%), having health insurance (51.5%), having received a recommendation from healthcare personnel to be screened (65.6%), and feeling worried about acquiring cervical cancer (56.1%) were associated with a higher proportion of preventive screening. Contrary to those who did not use contraceptive methods (45%), did not have health insurance (41.9%), did not receive a recommendation for screening (13.3%), and did not feel worried about acquiring this type of cancer (39.4%). Regarding these factors, a lower risk of screening is reported in women who live in urban areas and do not use a contraceptive method [23] and a higher prevalence of screening with the use of condoms [24].
Most of the women who responded that it is possible to prevent cancer (52.4%) heard of cervical cancer (52.8%) and human papillomavirus (56.9%). This is associated with a higher proportion of screening. However, self-reported screening is considered low, as reported in several studies [17,24,25]. As expected, contrary responses such as it is not possible to prevent cancer (25.9%), not having heard of cervical cancer (21%), or human papillomavirus (18.6%) had higher rates of not being screened. Although at least 9 out of 10 Peruvian women had heard of cancer, there was an alarming lack of cervical cancer awareness [28,29]. The strengthening of the educational-communication component and the injection of resources as possible effective solutions should be emphasized.
In this line, a higher proportion of screening was associated with believing that it is possible to cure cervical cancer with early detection (55.9%), compared to the women who thought the opposite was true (26.4%). Likewise, lower screening was associated with women who believed screening tests were risky (23.4%) compared to those who believed they were safe (52.9%). In relation to these results, health beliefs, such as perceived benefits and motivation to undergo screening tests, were associated with the intention to undergo preventive screening [26], as were perceived risk and certain psychological factors [30].
The study’s limitations are that the research design did not allow for establishing causal relationships. However, characterizing and evaluating associated factors allows us to identify and address specific needs in the variables and groups analyzed since the study intends that knowledge of these factors and their degree of association with performing the screening may indirectly contribute to increasing screening rates in the region. The incorporation of a large number of factors potentially associated with the variable " screening performance" into the study makes it, to a certain extent, an exploratory study that will eventually allow for more specific studies. The possibility of measurement bias is present since the variables were self-reported, which could slightly underestimate the results considering previous studies [17]. Likewise, it is debatable whether the sample studied from a large region of Peru is representative of the national population. For this reason, we suggest conducting new studies evaluating this aspect, including a larger sample size and a sampling of all Peruvian regions. On the other hand, the questions on cervical cancer awareness only ask about cervical cancer and human papillomavirus but do not go deeper into the subject. However, this study is relevant considering that it analyzes the performance of preventive screening at the first level of care in its privileged position within healthcare systems.
Conclusions
At the primary healthcare level of the Peruvian health system, there is still a low prevalence of preventive cervical cancer screening, self-reported by female users.
In the group of sociodemographic factors, higher proportions of screening were reported by women residing in urban areas (58.6%). The associated factor with the greatest impact on screening was the urban area of residence (adjusted prevalence ratio: 1.27), followed by having a higher level of education (adjusted prevalence ratio: 1.17).
In the group of socio-sanitary factors, higher proportions of screening were found in women who were recommended by healthcare personnel to be screened (65.6%). The associated factor with the greatest impact on screening was having received a recommendation for screening (adjusted prevalence ratio: 4.80), followed by having health insurance (adjusted prevalence ratio: 1.31), using contraceptive methods (adjusted prevalence ratio: 1.28), and being concerned about acquiring cervical cancer (adjusted prevalence ratio: 1.20).
In the group of factors related to cervical cancer awareness, women who responded that they had heard of the human papillomavirus (56.9%) had higher screening rates. The factor associated with the greatest impact on screening was having heard of the human papillomavirus (adjusted prevalence ratio: 2.90) and cervical cancer (adjusted prevalence ratio: 2.18), followed by believing that it is possible to prevent cancer (adjusted prevalence ratio: 1.47) and believing that the human papillomavirus can cause cervical cancer (adjusted prevalence ratio: 1.09).
In the attitudinal and informational factors group, higher proportions of screening were found in those who believe there is a possibility of curing cervical cancer with early detection (55.9%). The factor associated with the greatest impact on screening was the latter factor (adjusted prevalence ratio: 1.90), followed by those who considered screening risky (adjusted prevalence ratio: 0.52).
Consequently, some factors could increase the proportion of women who undergo preventive screening; these factors should be considered to improve screening behaviors and rates.

